Medicare is always primary if it’s your only form of coverage. When you introduce another form of coverage into the picture, there’s predetermined coordination of benefits. The coordination of benefits will determine what form of coverage is primary and what form of coverage is secondary. The primary coverage will pay first, and the secondary coverage pays second.
Full Answer
How do you determine if Medicare is primary or secondary?
Sep 13, 2021 · Medicare is always primary if it’s your only form of coverage. When you introduce another form of coverage into the picture, there’s predetermined coordination of benefits. The coordination of benefits will determine what form of coverage is primary and what form of coverage is secondary.
Is Medicare always your primary insurance?
Sep 09, 2020 · CMS’ MSP fact sheet provides a general overview of the Medicare secondary payer provision for billing staff of providers, physicians, and other suppliers and furnishes guidance regarding whether Medicare is the primary or secondary payer based upon specific situational criteria. If the patient ….
Who is primary over Medicare?
Type of Insurance: Conditions: Primary: Secondary : 65+ with job-based insurance: Fewer than 20 employees: Medicare Employer: 20+ employees: Employer: Medicare : Disabled job-based insurance: Fewer than 100 employees: Medicare: Employer: 100+ employees: Employer: Medicare : Liability insurance: Liability-related claims: Liability: Medicare: Unrelated medical claims: …
Does Medicare have to be primary?
Nov 03, 2020 · 8 Things to Watch Out for if You Have Secondary Insurance 1. You’ll have to pay two premiums. 2. You may have two deductibles. 3. You’ll have two different health insurance companies to juggle. 4. You may have two different types of plans (HMO and PPO for example) and it can get confusing. 5. You’ll have to remember which is primary. 6.

How do I know if my Medicare is primary?
If the employer has 100 or more employees, then your family member's group health plan pays first, and Medicare pays second. If the employer has less than 100 employees, but is part of a multi-employer or multiple employer group health plan, your family member's group health plan pays first and Medicare pays second.
How do I know if Medicare is primary or secondary?
Medicare is always primary if it's your only form of coverage. When you introduce another form of coverage into the picture, there's predetermined coordination of benefits. The coordination of benefits will determine what form of coverage is primary and what form of coverage is secondary.
How do you determine which insurance is primary?
Primary insurance is a health insurance plan that covers a person as an employee, subscriber, or member. Primary insurance is billed first when you receive health care. For example, health insurance you receive through your employer is typically your primary insurance.Oct 8, 2019
Is Medicare always the primary payer?
If you don't have any other insurance, Medicare will always be your primary insurance. In most cases, when you have multiple forms of insurance, Medicare will still be your primary insurance.
Does Medicare become primary at 65?
Medicare is primary when your employer has less than 20 employees. Medicare will pay first and then your group insurance will pay second. If this is your situation, it's important to enroll in both parts of Original Medicare when you are first eligible for coverage at age 65.Mar 1, 2020
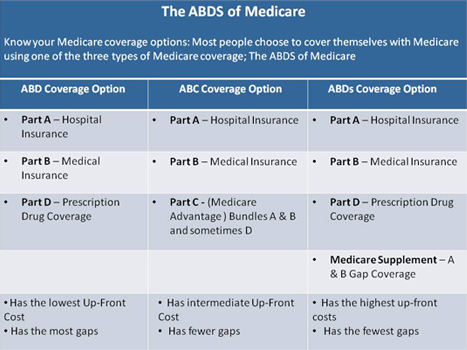
What type of insurance is Medicare?
Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles).
When two insurance which one is primary?
If you have two plans, your primary insurance is your main insurance. Except for company retirees on Medicare, the health insurance you receive through your employer is typically considered your primary health insurance plan.
What insurance is primary or secondary?
Primary insurance: the insurance that pays first is your “primary” insurance, and this plan will pay up to coverage limits. You may owe cost sharing. Secondary insurance: once your primary insurance has paid its share, the remaining bill goes to your “secondary” insurance, if you have more than one health plan.Jan 21, 2022
Can you have 2 primary insurances?
Yes, individuals can have coverage under two different health insurance plans. When two health insurance plan providers work together to pay the claims of one person, it's called coordination of benefits. The following situations are reasons employees would have dual insurance coverage: The employee is married.Feb 5, 2021
Does Medicare automatically forward claims to secondary insurance?
Medicare will send the secondary claims automatically if the secondary insurance information is on the claim. As of now, we have to submit to primary and once the payments are received than we submit the secondary.Aug 19, 2013
Can you have Medicare and Humana at the same time?
Depending on where you live, you may be able to find a Medicare plan from Humana that suits your needs. Unlike Original Medicare (Part A and Part B), which is a federal fee-for-service health insurance program, Humana is a private insurance company that contracts with Medicare to offer benefits to plan members.
Does Medicare cover copays from primary insurance?
Medicare will normally act as a primary payer and cover most of your costs once you're enrolled in benefits. Your other health insurance plan will then act as a secondary payer and cover any remaining costs, such as coinsurance or copayments.
What Is Medicare Primary Insurance?
Medicare Primary insurance simply means that Medicare pays first. Whether Medicare pays first or second depends on what types of other health cover...
Medicare Expects You to Know Who Is Primary
You see, Patricia didn’t realize that since her employer has less than 20 employees, Medicare would be her primary coverage. By failing to enroll i...
to Enroll Or Not to Enroll?
Not everyone needs to enroll in Medicare right when they turn 65. Many people continue to work past age 65 and have access to employer coverage thr...
When Medicare Is Secondary
Secondary insurance pays after your primary insurance. It serves to pick up costs that the primary coverage didn’t cover. For example, if your prim...
Feeling Unsure About When Is Medicare Primary?
Figuring all this out is enough to give anyone a headache – we know! Fortunately Boomer Benefits has helped tens of thousands of Medicare beneficia...
What is the age limit for a GHP?
Is age 65 or older, and is covered by a group health plan (GHP) through current employment or spouse’s current employment…. The employer has fewer than 20 employees…. Is age 65 or older, and is covered by a GHP through current employment or spouse’s current employment….
Is Medicare a cobra?
Medicare. Is age 65 or older OR is disabled and covered by Medicare and COBRA…. The patient is entitled to Medicare…. Medicare. COBRA. First Coast Service Options (First Coast) strives to ensure that the information available on our provider website is accurate, detailed, and current.
What is the difference between Medicare and Medicaid?
Eligible for Medicare. Medicare. Medicaid ( payer of last resort) 1 Liability insurance only pays on liability-related medical claims. 2 VA benefits and Medicare do not work together. Medicare does not pay for any care provided at a VA facility, and VA benefits typically do not work outside VA facilities.
Is Medicare a secondary insurance?
When you have Medicare and another type of insurance, Medicare is either your primary or secondary insurer. Use the table below to learn how Medicare coordinates with other insurances. Go Back. Type of Insurance. Conditions.
What is an EPO plan?
An Exclusive Provider Organization (EPO) is a managed care plan where services are covered only if you go to doctors, specialists and hospitals in the plan’s network. The only exception to this rule is in the case of an emergency. Health Insurance 15 Ways to Improve Your Gut Health.
How does coordination of benefits work?
The way coordination of benefits works is that when you have a health insurance claim, it should go first to the primary plan. That insurer will pay what it owes. If there’s a remainder, then that bill goes to the second insurer, which pays what it owes. You’ll then be responsible for what’s left over, if anything.
What is primary insurance?
Primary insurance means that it pays first for any healthcare services you receive. In most cases, the secondary insurance won’t pay unless the primary insurance has first paid its share. There are a number of situations when Medicare is primary.
When does Medicare end for ESRD?
You would then re-enroll when you turn 65. Typically Medicare due to ESRD will end 36 months after you’ve had your kidney transplant unless you also qualify for Medicare due to age or other disability.
Is Medicare primary or secondary?
Then of course there is employer coverage. If you have active employer coverage, whether Medicare is primary or secondary also depends on the size of the insurance company.
What is tricare for life?
You Have Tricare-for-Life. Tricare-for-Life (TFL) is for military retirees and their spouses who are also eligible for Medicare. In this scenario, Medicare is the primary insurance for any care you receive at non-military providers, so you need to enroll in both Part A and B.
Does Tricare cover vision?
People with Tricare sometimes also choose Medicare Advantage plans. Some Advantage plans include routine dental or vision benefits, and this may appeal to members with Tricare. Tricare for life will help to pick up some of the copays associated with Medicare Advantage.
Does medicaid pay first?
Medicaid is assistance with healthcare costs for people with low incomes. Medicaid never pays first. It will only pay after Medicare and or employer group health coverage has first paid. Not all Medicare providers accept Medicaid though. It’s important that you ask providers if they participate in Medicaid before seeking care. Otherwise, you may be responsible for the portions that Medicaid can’t cover.
Is Medicare a part of Medicaid?
Medicare is primary to Medicaid. People who qualify for Medicaid can get help paying for their Medicare Part B and D premiums. If your income is low and you think you might be eligible, contact your state Medicaid office for an application. To learn more about Medicare vs Medicaid, click here.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
Does Medicare pay for secondary insurance?
should send the bill to Medicare for secondary payment. Medicare will pay based on what the group health plan paid, what the group health plan allowed, and what the doctor or health care provider charged on the claim. You'll have to pay any costs Medicare or the group health plan doesn't cover.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What happens if a group health plan doesn't pay?
If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment. Medicare may pay based on what the group health plan paid, what the group health plan allowed, and what the doctor or health care provider charged on the claim.
What happens if you have two health insurance plans?
If you carry two health insurance plans and have deductibles with each plan, you’re responsible for paying both of them when you make a claim. In other words, don’t expect that if you pay a deductible on one plan, it will eliminate your obligation for the deductible on the other plan.
What is secondary insurance?
Secondary insurance. The secondary health insurance payer covers bills that the primary insurance payer didn’t cover. However, it is crucial to remember that the secondary insurance company may not pay all of the rest of your bills. You may be responsible for some health care costs.
What is the process of coordinating health insurance?
That way, both health plans pay their fair share without paying more than 100% of the medical costs. This process is called coordination of benefits.
How does COB work?
Here’s how COB works when there’s a health insurance claim: It first goes to the primary plan. The insurer pays what it owes. If there’s money still left on the bill, it then goes to the secondary insurer, which picks up what it owes.
Who pays the medical bill?
The primary insurance payer is the insurance company responsible for paying the claim first. When you receive health care services, the primary payer pays your medical bills up to the coverage limits. The secondary payer then reviews the remaining bill and picks up its portion.
Is Medicare considered primary?
Medicare and a private health plan – Typically, Medicare is considered primary if the worker is 65 or older and his or her employer has less than 20 employees. A private insurer is primary if the employer has 20 or more employees.
Can a child stay on their parents' health insurance?
A child under 26 - The Affordable Care Act lets children stay on their parents’ health plan until they turn 26. That could result in a child having her own health plan through an employer while remaining on the family’s plan. In that case, the child’s health plan is primary and the parents’ plan is secondary.
What is Medicare reporting?
Reporting Other Health Insurance. If you have Medicare and other health insurance or coverage, each type of coverage is called a "payer.". When there is more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" to pay.
Is Medicare a secondary payer?
You. Medicare may be your secondary payer. Your record should show whether a group health plan or other insurer should pay before Medicare. Paying claims right the first time prevents mistakes and problems with your health care plans. To ensure correct payment of your Medicare claims, you should:
What is a COB in Medicare?
The Medicare Coordination of Benefits (COB) program wants to make sure Medicare pays your claims right the first time, every time. The Benefits Coordination & Recovery Center (BCRC) collects information on your health care coverage and stores it in your Medicare record.
What is a secondary claim development questionnaire?
The Medicare Secondary Claim Development Questionnaire is sent to obtain information about other insurers that may pay before Medicare. When you return the questionnaire in a timely manner, you help ensure correct payment of your Medicare claims.
How long is ESRD primary?
If you have ESRD and have Medicare and group health insurance, including coverage from a former employer, the group plan is primary for the first 30 months of your eligibility for Medicare, after which Medicare becomes primary.
Is Medicare the primary insurance?
In some cases, Medicare is the primary payer, which means it is responsible for paying for covered charges before any other plans, which are called secondary payers ...
Is Medicare a primary or secondary payer?
In some cases, Medicare is the primary payer, which means it is responsible for paying for covered charges before any other plans, which are called secondary payers because they're responsible only for covered charges left unpaid by the primary payer. In other cases, the other plan is primary and Medicare is secondary.
Is Medicare primary for a 65 year old?
Many people who have reached age 65 have Medicare as well as coverage provided by their own or their spouse's current employer. In such cases, the group health plan is the primary payer unless the employer has less than 20 employees, in which case, Medicare is primary.
Is Medicare Supplements the same as Medicare Advantage?
Medicare supplements, also referred to as Medigap policies, are designed to cover the deductibles and co-insurance required by Medicare; thus, Medicare is always primary relative to Medicare supplements. Medicare Advantage plans, on the other hand, replace Medicare .
Is tricare covered by Medicare?
If you’re covered both by Medicare and TRICARE, a program for the uniformed services and their families, TRICARE covers services provided by military and other federal facilities, and Medicare is primary for covered services from non-federal providers. TRICARE usually pays Medicare deductibles and co-insurance, ...
Can you make Medicare primary?
Making Medicare Primary. If you’re in a situation where you have Medicare and some other health coverage, you can make Medicare primary by dropping the other coverage. Short of this, though, there’s no action you can take to change Medicare from secondary to primary payer.