Electronic process:
- Corrected claims can be submitted electronically as an EDI 837 transaction with the appropriate frequency code. ...
- Check Claims on Link to resubmit corrected claims that have been paid or denied.
- If you received a letter asking for additional information, submit it using Claims on Link.
Full Answer
How to resubmit rejected claims?
To access this screen:
- Log on to FISS
- At the Main Menu screen, enter "01" and press <ENTER>
- At the Inquiry Menu screen, enter "12" and press <ENTER>
- At the Claim Summary Inquiry screen, type your National Provider Identifier (NPI) in the NPI field, the beneficiary's Medicare ID number in the HIC field, and FISS status/location R B9997 ...
Does Medicare accept corrected claim?
You can send a corrected claim by following the below steps to all the insurances except Medicare (Medicare does not accept corrected claims electronically). To submit a corrected claim to Medicare make the correction and resubmit as a regular claim (Claim Type is Default) and Medicare will process it.
What if Medicare denies my claim?
- Your bill will be sent directly to Medicare.
- The appeal must be filed within 120 days of receiving the Medicare Summary Notice (MSN) that shows that your claim was denied.
- If you disagree with a Medicare coverage decision in the MSN, you can appeal the decision.
What to do if Medicare denies your medical claim?
You can also take other actions to help you accomplish this:
- Reread your plan rules to ensure you are properly following them.
- Gather as much support as you can from providers or other key medical personnel to back up your claim.
- Fill out each form as carefully and exactly as possible. If necessary, ask another person to help you with your claim.

Can you file a corrected claim to Medicare electronically?
You can send a corrected claim by following the below steps to all insurances except Medicare (Medicare does not accept corrected claims electronically). To submit a corrected claim to Medicare, make the correction and resubmit it as a regular claim (Claim Type is Default) and Medicare will process it.
How do I correct a Medicare billing error?
If the issue is with the hospital or a medical provider, call them and ask to speak with the person who handles insurance. They can help assist you in correcting the billing issue. Those with Original Medicare (parts A and B) can call 1-800-MEDICARE with any billing issues.
How long do I have to submit a corrected claim to Medicare?
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share.
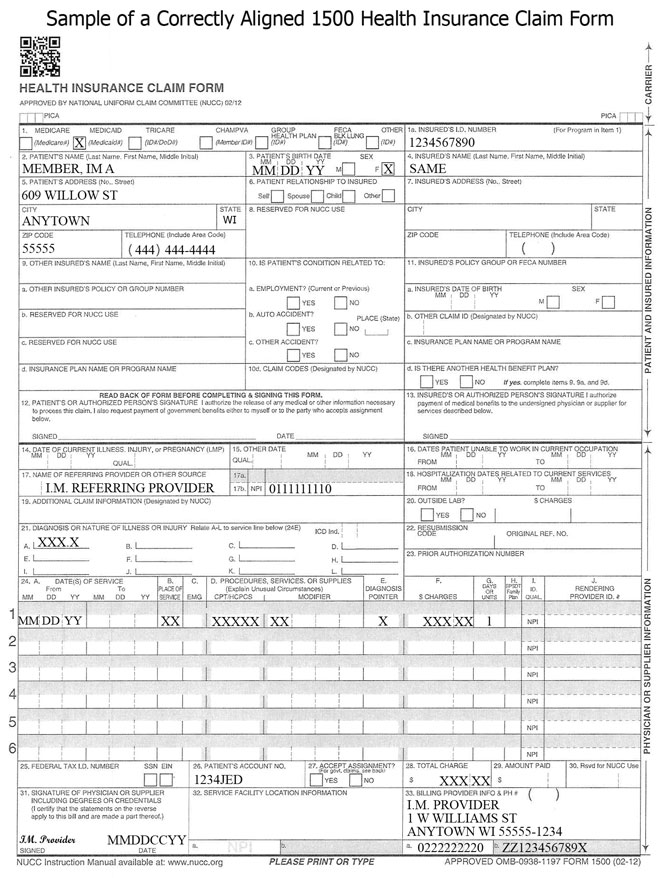
What is the resubmission code for a corrected claim for Medicare?
7Complete box 22 (Resubmission Code) to include a 7 (the "Replace" billing code) to notify us of a corrected or replacement claim, or insert an 8 (the “Void” billing code) to let us know you are voiding a previously submitted claim.
How do I submit a corrected claim to noridian?
ContactContact.855-609-9960.
Can I submit paper claims to Medicare?
The Administrative Simplification Compliance Act (ASCA) requires that as of October 16, 2003, all initial Medicare claims be submitted electronically, except in limited situations. Medicare is prohibited from payment of claims submitted on a paper claim form that do not meet the limited exception criteria. web page.
How do I fix an incorrectly processed claim?
Make Changes, Add Reference/Resubmission Numbers, and Then Resubmit: To resolve a claim problem, typically you will edit the charges or the patient record, add the payer claim control number, and then resubmit or “rebatch” the claim.
What is the difference between a corrected claim and a replacement claim?
A corrected or replacement claim is a replacement of a previously submitted claim (e.g., changes or corrections to charges, clinical or procedure codes, dates of service, member information, etc.). The new claim will be considered as a replacement of a previously processed claim.
Under what circumstances should a corrected claim be submitted?
A corrected claim should only be submitted for a claim that has already paid, was applied to the patient's deductible/copayment or was denied by the Plan, or for which you need to correct information on the original submission.
What is the process for claim resubmission?
When you resubmit a claim, you are creating a new claim and sending it to the payer. The payer receives the claim and treats it as a new claim. To resubmit a claim, it needs to be placed back into the Bill Insurance area.
How do I submit a corrected claim to 1500?
CMS-1500 should be submitted with the appropriate resubmission code (value of 7) in Box 22 of the paper claim with the original claim number of the corrected claim. Include a copy of the original Explanation of Payment (EOP) with the original claim number for which the corrected claim is being submitted.
What is the difference between resubmission code 6 and 7?
What is the difference between frequency code 6 and frequency code 7? Frequency code 6 is corrected claim and frequency code 7 is replace submitted claim.
How long does it take for Medicare to process a correction?
In general, Medicare claims must be filed to the Medicare claims processing contractor no later than 12 months, or 1 calendar year, from the date the services were furnished. This includes resubmitting corrected claims ...
How long does a clerical error reopening last?
Note: Effective May 1, 2019, requests to conduct a clerical error reopening will be limited to one year from the initial determination date with the exception of reporting an overpayment.
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
How long does it take for a RTP claim to be corrected?
The RTP claim is not corrected within 180 days (or no longer appears in the Claim Correction screen) and becomes inactive (IB9997)
When is a justification statement required for a claim adjustment?
A justification statement is required if the adjustment is submitted beyond the timely filing limit.
How to access RTP claims in DDE?
To access RTP claims in the DDE Claims Correction screen, select option 03 (Claims Correction) from the Main Menu and the appropriate menu selection under Claims Correction (21 – Inpatient, 23 – Outpatient, 25 – SNF).
What to do if you overpay a MSP?
If you identify an overpayment (e.g., due to a billing error or MSP involvement), you should submit an electronic adjustment or void the claim.
How long is RTP available for correction?
RTP claims remain in this location (TB9997) and are available for correction for 180 days.
What is claim adjustment?
The claim adjustment process is used to make corrections to processed or rejected claims. Adjustment claims may be submitted via DDE or your electronic software.
How to adjust a claim in DDE?
To adjust a claim via DDE, select option 03 (Claims Correction) from the Main Menu and the appropriate menu selection under Claim Adjustments (30 – Inpatient, 31 – Outpatient, 32 – SNF).
What is the responsibility of Medicare providers to ensure the information submitted on your billing transactions (claims, adjustments, and cancel?
Note:It is the responsibility of Medicare providers to ensure the information submitted on your billing transactions (claims, adjustments, and cancels) are correct, and according to Medicare regulations. CGS is required by the Centers for Medicare & Medicaid Services (CMS) to monitor claim submission errors through data analysis, and action may be taken when providers exhibit a pattern of submitting claims inappropriately, incorrectly or erroneously. Providers should be aware that a referral to the Office of Inspector General (OIG) may be made for Medicare fraud or abuse when a pattern of submitting claims inappropriately, incorrectly, or erroneously is identified.
What happens when a claim is submitted to the FISS?
When a claim is submitted into the FISS, it processes through a series of edits to ensure the information submitted on the claim is complete and correct. If the claim has incomplete, incorrect or missing information, it will be sent to your Return to Provider (RTP) file for you to correct. Claims in the RTP file receive a new date of receipt when they are corrected (F9’d) and are subject to the Medicare timely claim filing requirements. See the “Note” on page 7 of this chapter for additional information on Medicare timely filing guidelines.
How long does a claim stay in status after being suppressed?
After suppressing the view of a claim, it will no longer display in the RTP file; however, when viewing the Claim Inquiry (option 12) or Claim Count Summary (option 56) screens, the claim may still appear in status/location T B9997 for several weeks, until FISS purges suppressed claims to the “I” status.
How long is a claim in RTP?
NOTE: Claims are available in your RTP file for up to 36 months (see the “Note” below regarding timely filing). After 36 months, the claim will purge off of FISS. If you choose not to correct the claim in RTP, we strongly encourage you to suppress the view of the claim, wMIDh will remove the claim from your RTP file sooner. This will help to limit the number of claims that are viewable in your RTP file, and will assist you in avoiding duplicate claim submission errors. Refer to the “Suppress View” information later in this chapter. As a Medicare provider, you are accountable to ensure the information you submit on your claim is correct, and according to Medicare regulations. When claims are corrected from the RTP file, a new receipt date is assigned. Therefore, it is important to remember that Medicare timely claim filing requirements apply. Correct your claims as soon as possible. The “# DAYS” field on Map 1741 tells you how long the claim has been in your RTP file. If the #DAYS field is blank, the claim just went to the RTP file during the nightly system cycle. Additional information about timely filing requirements is available on the “Timely Claim Filing Requirements” (https://www. cgsmedicare.com/Articles/COPE18411.html ) CGS Web page.
Can you delete a claim in FISS?
Occasionally, you may have claims in RTP that you do not need to correct. Although FISS does not allow you to delete a claim in RTP, we strongly recommend that you suppress the view of a claim you choose not to correct to avoid duplicate billing errors. Suppressed claims will move to the status/location I B9997 (I=inactivated), and will no longer appear on your list of claims in your RTP file. The following steps explain how to suppress the view of a claim.
Can you adjust a claim after it has been processed?
At times, you may need to adjust a claim after it has been processed to make changes (e.g., add or remove services). Claim adjustments can be made to paid or rejected claims (i.e., status/ location P B9997 or R B9997). However, adjustments cannot be made to:
Can I reverse a B9997 claim?
This action cannot be reversed. Please make sure that you want to suppress the view of the claim before following the steps below. Suppressed claims (I B9997 status/location) will still appear when viewing claims in option 12 (Claim Summary Inquiry screen).
What is a redetermination in Medicare?
A redetermination is a written request, for a first level appeal, to the Medicare administrative contractor to review claim data when you are dissatisfied with the original claim determination. The redetermination is an independent process to re-evaluate the claim.
How long does it take to reopen a claim?
The claim can be reopened within one year from the date of the initial determination or redetermination for any reason or within four years from the date of the initial determination or redetermination for good cause:
What happens if you request a redetermination?
If the request for a redetermination is not approved or unfavorable, you will receive a letter notifying you of the decision. Requesting a redetermination.
What is general inquiry?
A general inquiry is a written correspondence initiated by you that includes questions related to Medicare billing, processing or payments. There may be times that a redetermination cannot be accepted and the request will be forwarded to the general inquires department for a response to you.
What is a clerical error reopening?
A clerical error reopening is a process that allows you to correct minor errors or omissions.
What happens if you accept a claim reopening?
If the request for a claim reopening is not approved, you will receive a letter notifying you of the decision.
Can a reopening be granted to add items or services that were not previously billed?
A reopening shall not be granted to add items or services that were not previously billed.

Claim Corrections
- You should only need to file a claim in very rare cases
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020. C…
Claim Adjustments
Claim Voids/Cancels
Clerical Error Reopenings
Overpayments
- The claim adjustment process is used to make corrections to processed or rejected claims. Adjustment claims may be submitted via DDE or your electronic software.
- Processed and rejected claims are finalized claims and appear on the RA. If a new claim is submitted, it will reject as a duplicate of the original claim.
- To determine the reason a claim/line item rejected, review the specific reason code assigned and/or the RA.
- The claim adjustment process is used to make corrections to processed or rejected claims. Adjustment claims may be submitted via DDE or your electronic software.
- Processed and rejected claims are finalized claims and appear on the RA. If a new claim is submitted, it will reject as a duplicate of the original claim.
- To determine the reason a claim/line item rejected, review the specific reason code assigned and/or the RA.
- Claim adjustments are subject to the same timely filing limit as new claims (i.e., within one calendar year of the "through" date of service on the claim). A justification statement is required if...
Medical Review Additional Development Request
- The claim void/cancel process is only used if a processed claim should never have been submitted.
- To cancel a claim via DDE, select option 03 (Claims Correction) from the Main Menu and the appropriate menu selection under Claim Cancels (50 – Inpatient, 51 – Outpatient, 52 – SNF).
- Void/cancel claims must contain:
Redeterminations
- The claim reopening process is available to correct clerical errors when the claim is beyond the timely filing limit.
- CMS defines clerical errors (including minor errors or omissions) as human or mechanical errors on the part of the provider or the contractor, such as:
- To request a claim reopening, complete the Clerical Error Reopening Request formand mail it along with the c…
- The claim reopening process is available to correct clerical errors when the claim is beyond the timely filing limit.
- CMS defines clerical errors (including minor errors or omissions) as human or mechanical errors on the part of the provider or the contractor, such as:
- To request a claim reopening, complete the Clerical Error Reopening Request formand mail it along with the corrected claim form to the J15 Part A Claims Department address listed on the form.
- To submit a claim reopening via DDE or your electronic software, please reference the following: