There are two ways to submit a receipt for reimbursement: Through the WageWorks EZ Receipts® mobile app. Use your mobile device to snap a photo of your receipts and submit them for reimbursement.
Full Answer
How do I generate a Medicare compliant invoice/receipt?
Processing an Appointment and Generating a Medicare Compliant Invoice/Receipt Anytime the client has an appointment with you simply click on the appointment in the calendar, select the Medicare service you provided, select the payment method they used (if any) and then click Save.
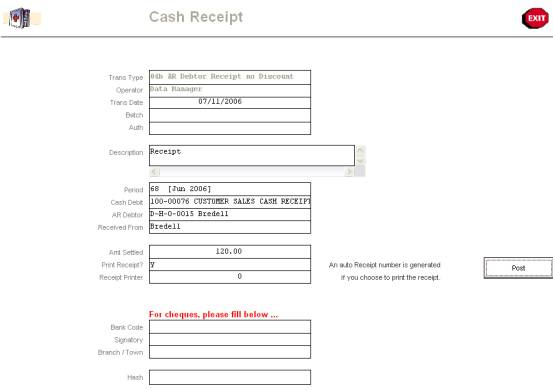
Do you get a monthly Medicare payment receipt?
We do not get monthly statements, just a deposit to our bank for the net amount. In order to get reimbursed by Aetna from the fund for the Medicare payment you need a monthly receipt showing the amount paid. Does anyone have any idea how to get such a receipt showing the monthly Medicare payment.
How do I setup my Medicare services?
Setup the services you provide ensuring you include a description of any Medicare Service / Item Number details. To do this go to Setup → Services and select Add Service. In the title or description, sections include the Medicare description e.g. "Standard Consultation 50min+" and in the Code section add the Medicare item code (such as 80110).
How do I automatically include my Medicare provider number on invoices?
To automatically include your Medicare Provider Number on all your invoices you produce navigate to Setup → Calendars, and then add your provider number details under the Insurers section (more details on adding your provider number can be found here)
How do you submit a bill to Medicare?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
Can you submit claims to Medicare electronically?
How to Submit Claims: Claims may be electronically submitted to a Medicare Administrative Contractor (MAC) from a provider using a computer with software that meets electronic filing requirements as established by the HIPAA claim standard and by meeting CMS requirements contained in the provider enrollment & ...
How do I get reimbursed for Medicare payments?
How do you file a Medicare reimbursement claim?Once you see the outstanding claims, first call the service provider to ask them to file the claim. ... Go to Medicare.gov and download the Patient Request of Medical Payment form CMS-1490-S.Fill out the form by carefully following the instructions provided.More items...
What is the first step in submitting Medicare claims?
The first thing you'll need to do when filing your claim is to fill out the Patient's Request for Medical Payment form. ... The next step in filing your own claim is to get an itemized bill for your medical treatment.More items...•
Does Medicare still accept paper claims?
The Administrative Simplification Compliance Act (ASCA) requires that as of October 16, 2003, all initial Medicare claims be submitted electronically, except in limited situations. Medicare is prohibited from payment of claims submitted on a paper claim form that do not meet the limited exception criteria. web page.
Where do I fax Medicare claims?
Complete all fields and fax to 877- 439-5479 or mail the form to the applicable address/number provided at the bottom of the page. Complete ONE (1) Medicare Fax / Mail Cover Sheet for each electronic claim for which documentation is being submitted. This form should not be submitted prior to filing the claim.
How do I get my $800 back from Medicare?
All you have to do is provide proof that you pay Medicare Part B premiums. Each eligible active or retired member on a contract with Medicare Part A and Part B, including covered spouses, can get their own $800 reimbursement.
How do you qualify for $144 back from Medicare?
How do I qualify for the giveback?Are enrolled in Part A and Part B.Do not rely on government or other assistance for your Part B premium.Live in the zip code service area of a plan that offers this program.Enroll in an MA plan that provides a giveback benefit.
How do I get my Medicare Part B reimbursement?
2. What document do I need to submit to receive my correct Part B reimbursement amount? You must submit a copy of your Social Security benefits verification statement (your “New Benefit Amount”) or a copy of a 2022 Centers for Medicare and Medicaid Services (CMS) billing statement.
What form is used to send claims to Medicare?
CMS-1500 claim formThe CMS-1500 claim form is used to submit non-institutional claims for health care services provided by physicians, other providers and suppliers to Medicare.
How are Medicare claims processed?
Your provider sends your claim to Medicare and your insurer. Medicare is primary payer and sends payment directly to the provider. The insurer is secondary payer and pays what they owe directly to the provider. Then the insurer sends you an Explanation of Benefits (EOB) saying what you owe, if anything.
How long does a Medicare claim take?
Using the Medicare online account When you submit a claim online, you'll usually get your benefit within 7 days.
When do I need to file a claim?
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020.
How do I file a claim?
Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
What do I submit with the claim?
Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items:
How Are Providers Reimbursed for Their Services?
If your provider (doctor, nurse, lab, etc.) accepts assignment, Medicare pays them for any covered services. That’s what “ accepts assignment ” means. It is an agreement between your provider and Medicare. The provider agrees to accept the Medicare-approved amount for the service and Medicare agrees to pay for the service.
What Do You Pay When Your Provider Accepts Assignment?
Providers who accept assignment agree to charge only the amount Medicare approves for a particular service. In other words, if the provider normally charges $150 for a service, but Medicare sets the rate at $100, the provider cannot charge more than $100.
When Do You File for Medicare Claim Reimbursement?
About the only time you need to file for Medicare claim reimbursement is if the provider does not accept assignment. In this instance, the provider can charge you more than the Medicare-approved amount. However, they can only add 15 percent to Medicare’s approved rate. This is known as an excess charge. Using our $100 vs.
How to File a Medicare Claim Reimbursement
To file a claim for reimbursement, you need to submit the proper form and backup documentation. First, download the Patient’s Request for Medical Payment form from the Centers for Medicare and Medicaid Services (CMS).
What If You Have a Medicare Advantage or Part D Plan?
The claims reimbursement process is different if you have either a Medicare Advantage or Part D plan. That is because these plans are offered through private insurance companies, not Medicare. The claims process varies according to your insurer. Check with your plan to determine your insurer’s unique claims process.
Getting Help with Your Medicare Claim Reimbursement
Even if you receive your benefits through an Advantage or Part D plan, you have the same rights as those who have Original Medicare. Contact your Medicare beneficiary ombudsman if you have an issue with your plan.
Step 2: confirm patient details
If you have multiple people listed on your Medicare card, select who received the service, followed by Next.
Step 6: sign out
From your homepage you can complete other transactions or select the myGov icon to return to myGov.
Recent Questions
How long does it take for Medicaid to begin once my mom is in the facility? This is now 5 weeks.
Popular Questions
How much can an elderly parent give as gifts without worrying about "look back" laws?
Related Questions
Does Illinois Medicaid provide caregivers in the home for a 39-year-old disabled female?
When Do I Need to File A Claim?
How Do I File A Claim?
- Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
What Do I Submit with The Claim?
- Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1. The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2. The itemized bill from your doctor, supplier, or other health care provider 3. A letter explaining in detail your reason for subm…
Where Do I Send The Claim?
- The address for where to send your claim can be found in 2 places: 1. On the second page of the instructions for the type of claim you’re filing (listed above under "How do I file a claim?"). 2. On your "Medicare Summary Notice" (MSN). You can also log into your Medicare accountto sign up to get your MSNs electronically and view or download them an...