For example, if Medicare paid $100,000 in medical costs, and the claim was settled for $200,000 with the attorney receiving $66,000 in fees and $20,000 for costs, Medicare would normally reduce its lien by the percentages of fees and costs as compared to the total settlement.
How is a Medicare lien reduction determined?
How the Fees and Costs Lien Reduction is Determined: Normally, Medicare will reduce the amount it is seeking to reflect the amount paid in attorney fees and costs.
How do I handle a Medicare lien claim?
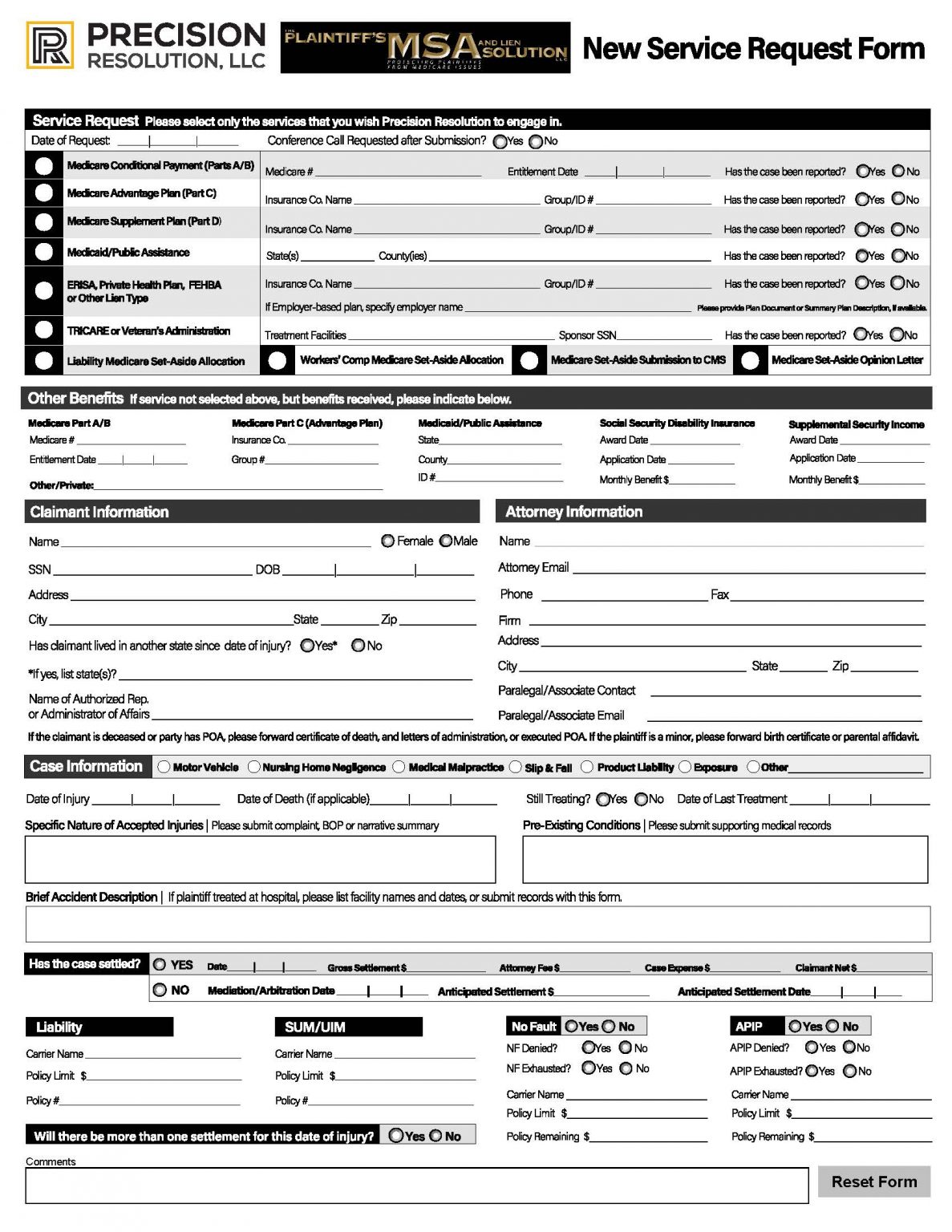
Step One: Obtain Medicare Information from the Client at the Initial Meeting and Warn Them that Medicare Liens are Difficult and Can Cause Delays throughout Their Case In addition to finding out information about any type of lien claim at your first meeting with the client, be sure to find out if the client receives Medicare benefits.
How can I get a lien reduction?
Your best chance at getting success in getting a lien reduction is to have the highest person on your law firm's food chain making the call. Why? Because it underscores just how important and necessary the reduction is.
What medical costs make up the Medicare lien?
Determining What Medical Costs Make Up the Medicare Lien: Medicare is only allowed to seek reimbursement of medical costs attributed to the treatment and care for the injuries suffered as a result of the incident giving rise to the personal injury claim.
Can you negotiate Medicare liens?
This means that if you get a settlement, you will have to pay back Medicare before anything else gets taken out. While you can get the lien reduced, paying back Medicare after a settlement is not optional. The only path around a Medicare lien is to negotiate the lien to zero.
What is Medicare lien resolution?
Medicare “liens” are a well-known part of every personal injury lawyer's settlement checklist. If a law firm obtains a settlement, judgment, or award for a Medicare beneficiary and Medicare paid for that individual's injury-related medical care, Medicare must be reimbursed for payments it made on a conditional basis.
What are Medicare liens?
A Medicare lien results when Medicare makes a “conditional payment” for healthcare, even though a liability claim is in process that could eventually result in payment for the same care, as is the case with many asbestos-related illnesses.
What are Medicare procurement costs?
In individual cases, Medicare will reduce or offset its lien for part of what's called “procurement costs.” Procurement costs are the costs typically incurred pursuing a personal injury claims (such as court costs, attorney's fees, and other case expenses).
Do you ever have to pay Medicare back?
The payment is "conditional" because it must be repaid to Medicare if you get a settlement, judgment, award, or other payment later. You're responsible for making sure Medicare gets repaid from the settlement, judgment, award, or other payment.
Why would I get letter from CMS?
In general, CMS issues the demand letter directly to: The Medicare beneficiary when the beneficiary has obtained a settlement, judgment, award or other payment.
How far back can Medicare recoup payments?
(1) Medicare contractors can begin recoupment no earlier than 41 days from the date of the initial overpayment demand but shall cease recoupment of the overpayment in question, upon receipt of a timely and valid request for a redetermination of an overpayment.
Does Medicare Subrogate?
Subrogation rules are written into the statutes that govern Medicare and Medicaid. Virtually always, if Medicare or Medicaid paid medical expenses incurred because of a personal injury, there will be at least some subrogation payment from a personal injury judgment or settlement.
Does Medicare have a statute of limitations?
FEDERAL STATUTE OF LIMITATIONS For Medicaid and Medicare fraud, federal law establishes (1) a civil statute of limitations of six years (42 U.S.C. § 1320a-7a(c)(1)), and (2) a criminal statute of limitations of five years (18 U.S.C. § 3282).
What are procurement costs?
Procurement costs are the expenses your organization incurs to provide the goods or services your customers expect.
How do providers get reimbursed by Medicare?
Traditional Medicare reimbursements When an individual has traditional Medicare, they will generally never see a bill from a healthcare provider. Instead, the law states that providers must send the claim directly to Medicare. Medicare then reimburses the medical costs directly to the service provider.
How do I get reimbursed from Medicare?
How to Get Reimbursed From Medicare. To get reimbursement, you must send in a completed claim form and an itemized bill that supports your claim. It includes detailed instructions for submitting your request. You can fill it out on your computer and print it out.
How long does it take for Medicare to pay final demand?
Medicare's final demand amount will account for the reduction for a share of attorneys' fees and costs. Send them a check for amount requested within 60 days, or interest will accrue.
What is the black hole in Medicare?
It takes FOREVER to get a response from the black hole that is known as Medicare's Benefits Coordination and Recovery Contractor. The BCRC collects the information for Medicare and opens the file with the Medicare Secondary Payor Recovery Center (MSPRC).
Can you self calculate Medicare payment?
You can also self-calcula te your conditional payment amount if you meet certain eligibility criteria. Use this form to indicate that you meet the criteria, and what you calculate to be the conditional payment amount, and send it in to the Medicare address listed on the form.
Does Medicare move quickly?
As you will see, Medicare does not move quickly in providing information at any step of this process. Warning your client at the outset will prevent many anxious calls from your client at the end of your case when they are wondering why they have not gotten their settlement money.
Can you groan at a lien on Medicare?
If you have any experience in personal injury cases, chances are you groan with frustration at even the thought of handling a case involving a Medicare lien. And with good reason. In my experience, getting information out of Medicare is like pulling teeth, to put it mildly. If you start early, and remain organized, ...
Can you stop Medicare from holding up settlement check?
If you start early, and remain organized, you can prevent Medicare from holding up your settlement check at the end of your case, which can happen if you do not have Medicare's final demand when it's time for the adjuster to issue the settlement check.
Final Conditional Payment Process
The Final Conditional Payment process permits you to obtain time and date stamped final conditional payment summary documents before reaching settlement and ensures that relatedness disputes are addressed within 11 business days of receipt of dispute documentation.
Self-Calculated Conditional Payment Amount
The Self-Calculated Conditional Payment Amount enables you to self-calculate the demand amount before settlement in certain situations. The following conditions must be met for Medicare to provide the demand amount before settlement is reached:
Fixed Percentage Option
If a settled case meets certain eligibility criteria, you or your attorney or other representative may request that Medicare’s demand amount be calculated using the Fixed Percentage Option. The Fixed Percentage Option offers a simple, straightforward process to obtain the amount due to Medicare.
What is included in a demand letter for Medicare?
The demand letter also includes information on administrative appeal rights. For demands issued directly to beneficiaries, Medicare will take the beneficiary’s reasonable procurement costs (e.g., attorney fees and expenses) into consideration when determining its demand amount.
What is Medicare beneficiary?
The Medicare beneficiary when the beneficiary has obtained a settlement, judgment, award or other payment. The liability insurer (including a self-insured entity), no-fault insurer, or workers’ compensation (WC) entity when that insurer or WC entity has ongoing responsibility for medicals (ORM). For ORM, there may be multiple recoveries ...
How long does interest accrue?
Interest accrues from the date of the demand letter, but is only assessed if the debt is not repaid or otherwise resolved within the time period specified in the recovery demand letter. Interest is due and payable for each full 30-day period the debt remains unresolved; payments are applied to interest first and then to the principal. Interest is assessed on unpaid debts even if a debtor is pursuing an appeal or a beneficiary is requesting a waiver of recovery; the only way to avoid the interest assessment is to repay the demanded amount within the specified time frame. If the waiver of recovery or appeal is granted, the debtor will receive a refund.
How long does it take to appeal a debt?
The appeal must be filed no later than 120 days from the date the demand letter is received. To file an appeal, send a letter explaining why the amount or existence of the debt is incorrect with applicable supporting documentation.
Who has the right to appeal a demand letter?
This means that if the demand letter is directed to the beneficiary, the beneficiary has the right to appeal. If the demand letter is directed to the liability insurer, no-fault insurer or WC entity, that entity has the right to appeal.
Can CMS issue more than one demand letter?
For ORM, there may be multiple recoveries to account for the period of ORM, which means that CMS may issue more than one demand letter. When Medicare is notified of a settlement, judgment, award, or other payment, including ORM, the recovery contractor will perform a search of Medicare paid claims history.
What is Medicare lien?
To enforce this right to reimbursement, a “Medicare lien” will attach to judgment or settlement proceeds that are awarded as compensation for the accident. This means that if you get a settlement, you will have to pay back Medicare before anything else gets taken out.
How much can Medicare fine for reporting?
Additionally, Medicare can fine the “Responsible Reporting Entity,” usually the insurer, up to $1,000 for each day that they are out of compliance with Medicare’s reporting requirements. That is some harsh medicine. It leaves insurance companies stone terrified.
How does a lien work in personal injury?
How Medicare Liens Work in Personal Injury Cases. If you are injured in an accident and Medicare pays for some of your treatment, you will be obligated to reimburse Medicare for these payments if you bring a personal injury claim and get financial compensation for the accident. To enforce this right to reimbursement, ...
How much did Meyers Rodbell pay for malpractice?
Under the terms of the agreement entered into with the U.S. Attorney’s Office for the District of Maryland, Meyers Rodbell had to pay the $250,000 for the Medicare lien in the malpractice case. The firm was also required to adopt certain policies for handling Medicare liens in future cases.
How long does it take for a personal injury claim to be reported to Medicare?
Any settlement or payment must be reported to Medicare within 60 days and their valid lien amount must be paid.
Does Medicare enforce a lien?
Medicare Actively Enforces These Liens. If a Medicare lien is not properly handled and paid off, Medicare is permitted to file against the defendant, the plaintiff, or the plaintiff’s counsel. If Medicare is forced to bring suit against a party to collect its lien, in some situations it is entitled to a civil penalty of two times the amount owed.
Does Medicare have a lien on personal injury settlements?
If a Medicare beneficiary receives a personal injury settlement, they will be required to reimburse Medicare for any payments made on their behalf. To enforce this requirement, the law gives Medicare an automatic priority lien against any settlement proceeds in personal injury cases.
How long does it take for Medicare to resolve a lien?
Resolving the Medicare Lien Can Take Months: Normally, Medicare liens take three or more months to resolve.
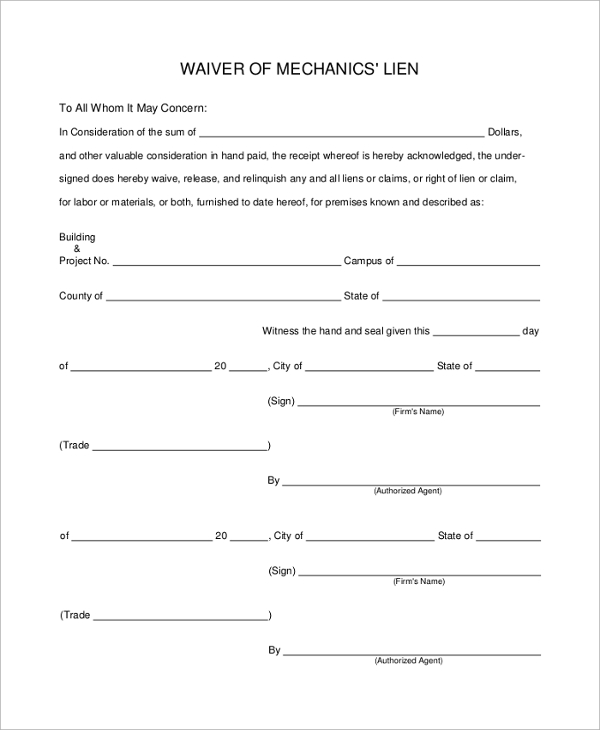
What is the Medicare lien waiver process?
One great feature of the Medicare lien waiver process is that each time an appeal is made, the appeal is reviewed by a new group of individuals who take a “new look” at the material and are not guided by the decisions of the individuals who may have denied the waiver in an earlier evaluation. Thus, the applicant gets more than one bite ...
How long does it take for a lien to be settled?
Normally, Medicare liens take three or more months to resolve. Occasionally, the lien is settled in less time, but if Medicare is seeking reimbursement for unrelated treatments, such that your attorney and Medicare are involved in a negotiation of what medical expenses are “related” and which are not, the process can take considerably longer.
Why is Medicare a barrier to settlement?
While resolving Medicare liens in most personal injury cases is a straight-forward process, sometimes the Medicare lien presents a barrier to settlement because the payment required is unreasonable in light of the facts of the particular case or claim. This article is intended to provide an overview of how Medicare liens are handled in ...
Can Medicare reimburse medical bills?
Medicare is only allowed to seek reimbursement of medical costs attributed to the treatment and care for the injuries suffered as a result of the incident giving rise to the personal injury claim. Many Medicare recipients go to the doctor’s office or are admitted to the hospital for numerous health issues, some of which are completely unrelated ...
Does Medicare reduce attorney fees?
Normally, Medicare will reduce the amount it is seeking to reflect the amount paid in attorney fees and costs. For example, if Medicare paid $100,000 in medical costs, and the claim was settled for $200,000 with the attorney receiving $66,000 in fees and $20,000 for costs, Medicare would normally reduce its lien by the percentages ...
Does Blue Cross have liens?
Other insurance entities may also have liens, such a Medi-Cal or your private insurance company (such as Blue Cross, or Anthem). While similar to Medicare liens, such liens are handled differently. Please call with any questions you may have regarding this article of the handing of personal injury cases in general.
How much can a lien claim be in California?
Civil Code section 3040 (c) (2) provides that if the insured (your client) retains an attorney, the lien claim cannot exceed "one-third of the moneys due to the enrollee or insured under any final judgment, compromise, or settlement agreement.".
Why was the lien reduced to one sixth of the amount?
There, the court reduced the lien claim to one-sixth of the amount because the recovery by the plaintiff in that case was only one-sixth of the value of the case due to plaintiff's comparative fault, as evidenced by the stipulation of the parties.
What to do if medical bills are not included in settlement offer?
If, for whatever reason, certain medical bills are not part of the settlement offer, point that out to the lien claimant and advise that they should not be included in the lien claim. You may also have a situation where there is a significant amount of wage loss or pain and suffering, and the defendant's policy is limited.
Can a lien be more than the cost to perfect the lien?
For example, in California, under Cal. Civil Code section 3040, health insurance liens can be no more than the cost to perfect the lien and the amount actually paid for non-capitated charges, and 80% for capitated charges (i.e. Kaiser, a system in which a medical provider is given a set fee per patient).
Can you have multiple lien claims?
If you have multiple lien claims, particularly when you have a limited 3rd party policy from which to recover funds, it can be beneficial to figure out a proportionate share of the statutory cap for each lien claim.

Final Conditional Payment Process
Self-Calculated Conditional Payment Amount
- The Self-Calculated Conditional Payment Amount enables you to self-calculate the demand amount before settlement in certain situations. The following conditions must be met for Medicare to provide the demand amount before settlement is reached: 1. The claim and settlement must be for an injury caused by physical trauma. The settlement cannot involv...
Fixed Percentage Option
- If a settled case meets certain eligibility criteria, you or your attorney or other representative may request that Medicare’s demand amount be calculated using the Fixed Percentage Option. The Fixed Percentage Option offers a simple, straightforward process to obtain the amount due to Medicare. It eliminates time and resources typically associated with the Medicare Secondary Pa…