How Do I Get a Prior Authorization?
- Talk to Your Provider's Office. The first thing you'll need to do to start the process of getting prior authorization is...
- Fill Out Paperwork. You will probably be asked to fill out some forms that your provider's office will use to submit the...
- Get Organized. As you're gathering and completing paperwork as part of your prior...
What does Medicare require prior authorization?
- Blepharoplasty
- Botulinum toxin injections
- Panniculectomy
- Rhinoplasty
- Vein ablation
Does Medicare require prior authorization?
Traditionally, both parts of Original Medicare (Medicare Parts A and B) rarely require pre-approval. Originally, Medicare Part A required no prior authorization whatsoever. Now however, the law has been changed to allow this process for certain limited Durable Medical Equipment items on very rare occasions.
How to enroll in Medicare if you are turning 65?
- You have no other health insurance
- You have health insurance that you bought yourself (not provided by an employer)
- You have retiree benefits from a former employer (your own or your spouse’s)
- You have COBRA coverage that extends the insurance you or your spouse received from an employer while working
Where to get free Medicare advice?
- You have full Medicaid coverage.
- You get help from a Medicare savings program.
- You receive Supplemental Security Income (SSI) benefits from the Social Security Administration.
What is prior authorization Medicare?
Prior authorization is a requirement that a health care provider obtain approval from Medicare to provide a given service. Prior Authorization is about cost-savings, not care. Under Prior Authorization, benefits are only paid if the medical care has been pre-approved by Medicare.
What is the prior authorization process?
Prior authorization—sometimes called precertification or prior approval—is a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage.
How long does it take for Medicare to approve a procedure?
Medicare takes approximately 30 days to process each claim. Medicare pays Part A claims (inpatient hospital care, inpatient skilled nursing facility care, skilled home health care and hospice care) directly to the facility or agency that provides the care.
What does needing prior authorization mean?
Prior authorization is an approval of coverage from your insurance company, not your doctor. It's a restriction put in place to determine whether or not they will pay for certain medicines. It doesn't affect cash payment for prescriptions. Plus it's only required on those prescriptions when billed through insurance.
How long does a prior authorization take?
Prior authorization decisions will typically be reviewed in five business days. This is sufficient time to work with your treating physician.
How can I speed up my prior authorization?
16 Tips That Speed Up The Prior Authorization ProcessCreate a master list of procedures that require authorizations.Document denial reasons.Sign up for payor newsletters.Stay informed of changing industry standards.Designate prior authorization responsibilities to the same staff member(s).More items...
Does traditional Medicare require prior authorization?
Traditional Medicare, in contrast, does not require prior authorization for the vast majority of services, except under limited circumstances, although some think expanding use of prior authorization could help traditional Medicare reduce inappropriate service use and related costs.
What services does not require prior authorization?
No pre-authorization is required for outpatient emergency services as well as Post-stabilization Care Services (services that the treating physician views as medically necessary after the emergency medical condition has been stabilized to maintain the patient's stabilized condition) provided in any Emergency Department ...
How do I submit an authorization to Medicare?
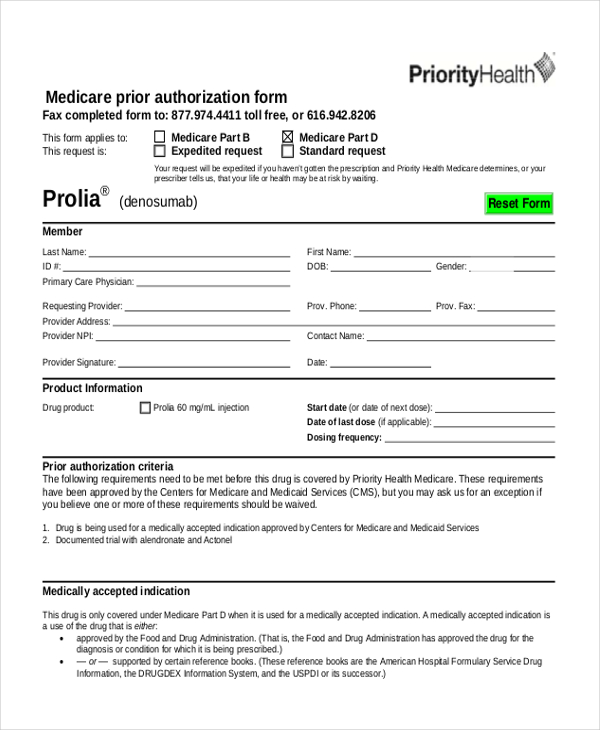
To do so, you can print out and complete this Medicare Part D prior authorization form, known as a Coverage Determination Request Form, and mail or fax it to your plan's office. You should get assistance from your doctor when filling out the form, and be sure to get their required signature on the form.
What is the difference between pre-authorization and prior authorization?
Sometimes they are called pre-approvals, or prior approvals, or prior authorizations, but they all mean the same thing. This practice is common in all types of insurance, even with government-sponsored coverage like Medicare, Medicaid, and Tricare.
Which of the following are needed to submit a prior authorization request for medical equipment?
Which of the following are needed to submit a prior authorization request for medical equipment? scanning the files and electronically cataloging to the patient's file. You just studied 16 terms!
Why is it important to get preauthorization if the patient's insurance requires you to do so?
Before certain procedures can be preformed or a patient hospitalization, many insurance companies require precertification's or preauthorization. If this is not done, insurance claims will be denied.
What is prior authorization in Medicare?
Medicare Prior Authorization. Prior authorization is a requirement that a health care provider obtain approval from Medicare to provide a given service. Prior Authorization is about cost-savings, not care. Under Prior Authorization, benefits are only paid if the medical care has been pre-approved by Medicare.
Do Medicare Advantage plans require prior authorization?
Private, for-profit plans often require Prior Authorization. Medicare Advantage (MA) plans also often require prior authorization to see specialists, get out-of-network care, get non-emergency hospital care, and more.
What is pre claim review?
Under pre-claim review, the provider or supplier submits the pre-claim review request and receives the decision prior to claim submission; however, the provider or supplier can render services before submitting the request. A provider or supplier submits either the prior authorization request or pre-claim review request with all supporting medical ...
What is CMS in Medicare?
The Centers for Medicare & Medicaid Services (CMS) runs a variety of programs that support efforts to safeguard beneficiaries’ access to medically necessary items and services while reducing improper Medicare billing and payments. Through prior authorization and pre-claim review initiatives, CMS helps ensure compliance with Medicare rules.
What Are The Negative Effects Of Prior Authorization
Perhaps the most significant negative effect is that prior authorization delays patient access to care. It adds a speed bump to the patient journey, and can lead some patients to forgo treatment.
Adhere To The Guideline Provided For Submission
Your prior authorization request may not get approved if you fail to follow the plans instruction. Accordingly, you must meet the criteria specified in the plans policy before attempting to submit the PA form. In that regard, check to see that you tick every box before they take the form for submission.
Does Medicare Require Prior Authorizations
Beneficiaries with Original Medicare generally do not need to obtain a prior authorization form for most Medicare services, such as doctors visits, hospitalizations, diagnostic studies or treatments.
Submit Thorough And Accurate Info
When you submit a prior authorization request, make sure the information you submit is totally accurate and is thorough. Prior authorization requests can be denied or delayed because of seemingly mundane mistakes.
Medicare Part D Prior Authorization
Often, even top Part D prescription drug plans need prior authorization for coverage on specific drugs. Different policies have varying rules, so youll need to contact the carrier directly to confirm coverage.
When Claims Are Denied For No Authorization
Even as billers work diligently to reduce claims denials, payers are expanding the number of visit types and procedures that require prior authorization leading to an upswing in denials for some practices. It is estimated that 80% of denied claims have to do with no authorization being obtained, or authorizations being requested improperly.
Submit New Prior Authorization Request
Part A users may submit a request for a new Prior Authorization request by completing and uploading the Prior Authorization coversheet. As of June 17, 2020, Prior Authorizations are only required for certain Hospital Outpatient Department services.
Why do we need prior authorization?
Prior authorization can help protect a beneficiary’s rights to covered Medicare benefits, and it can also act as a means of reducing improper billing, waste and fraud within the Medicare system . It also helps to cut down on over-utilization of unnecessary care.
Do you need prior authorization for Medicare Part C?
It’s not uncommon, however, for beneficiaries of Medicare Advantage (Medicare Part C) plans and Medicare Part D Prescription Drug plans to need prior authorization before receiving some types of care. Prior authorization is most common for getting certain prescription drugs covered by your plan.
What is Medicare prior authorization?
There are many confusing terms that are used when discussing Medicare health insurance, among them is the term “prior authorization.” This term refers to the requirement which states that a healthcare provider must obtain approval from the Medicare program itself in order to provide a given medical service or treatment.
When does Medicare require prior authorization?
Traditionally, both parts of Original Medicare (Medicare Parts A and B) rarely require pre-approval. Originally, Medicare Part A required no prior authorization whatsoever. Now however, the law has been changed to allow this process for certain limited Durable Medical Equipment items on very rare occasions.
How long does it take for prior authorization to come into effect?
Depending on the way in which your forms are submitted, it may take several days to a week for prior authorization to take effect and allow coverage for your medical equipment, prescription medication, and other treatment and service needs, to begin.
How to request a prior authorization?
When your doctor submits your request for prior authorization or appeals a rejected prior authorization, they should: 1 Include clinical information that shows the reviewer you’ve met the guidelines for the test, service, or drug you’re requesting. Don't assume the reviewer knows anything about your health other than what you're submitting. 2 If you haven't met the guidelines, submit information explaining why not.
What to do if your doctor denied your prior authorization?
If your request for prior authorization has been denied, you have the right to know why. You can ask your doctor’s office, but you might get more detailed information by asking the medical management company that denied the request in the first place.
What happens if you don't get authorization from your health insurance?
If you don’t get permission from your health plan, your health insurance won’t pay for the service. You’ll be stuck paying the bill yourself. Although your doctor's office will make the prior authorization request and work with your insurer to get approval, it's also in your best interest to understand how this process works ...
Why is my prior authorization request denied?
Prior authorization requests can be denied or delayed because of seemingly mundane mistakes.
What to do if you don't know which benefits management company is handling your prior authorization request?
If you’re not sure which benefits management company is handling your prior authorization request, your health plan will point you in the right direction But, don’t count on your health plan personnel to be able to make the decision about approving or denying your request. Save your breath until you speak to the person who actually makes ...
Does health insurance require prior authorization?
While it’s your health insurance company that requires pre-authorization, it’s not necessarily your health insurance company that makes the decision about whether your prior authorization request is approved or denied. Although a few health plans still do prior authorizations in-house, many contract these tasks out to benefit management companies.
Can insurance require prior authorization for mental health?
For example, an insurer cannot require prior authorization to determine medical necessity for mental health or substance abuse treatments if they don't have a similar protocol for medical/surgical treatments. 1.
How long does it take to get a prior authorization?
Please note that all initial prior authorization decisions should be made in no more than 10 days. In cases where that timeframe could seriously jeopardize the life or health of the beneficiary, you may request an expedited review. Decisions for substantiated expedited reviews should be made within 2 business days.
When will phase 2 of DME start?
Phase II will begin October 21, 2019 and expands prior authorization of these codes to the remaining states and territories.
When is the CMS call for pressure reducing support surfaces?
CMS will host a call to discuss the addition of pressure reducing support surfaces to the Required Prior Authorization List on Tuesday, June 4, 2019 from 2:00 p.m. to 3:30 p.m. Eastern Time (ET). For more information, please visit the Special Open Door Forums webpage.
When will LLPs be approved?
Prior Authorization for LLPs will be implemented in two phases. Phase one will begin May 11, 2020 in one state from each DME MAC jurisdiction: California, Michigan, Pennsylvania, and Texas. Phase two will begin October 8, 2020 and expands prior authorization of these codes to all of the remaining states and territories.
When is L5856 required?
Additionally, prior authorization will be required for certain Lower Limb Prosthetics (L5856, L5857, L5858, L5973, L5980, and L5987), with dates of service on or after September 1, 2020 in California, Michigan, Pennsylvania, and Texas. On December 1, 2020, prior authorization for these codes will be required in all of the remaining states ...
When will the DMEPOS process end?
Given the importance of medical review activities to CMS’ program integrity efforts, CMS will discontinue exercising enforcement discretion for the Prior Authorization Process for Certain Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) items beginning on August 3, 2020, regardless of the status of the public health emergency. For Power Mobility Devices and Pressure Reducing Support Surfaces that require prior authorization as a condition of payment, claims with an initial date of service on or after August 3, 2020 must be associated with an affirmative prior authorization decision to be eligible for payment.
When does pre-authorization for outpatients start?
Pre-authorizations have recently been introduced to certain hospital procedures conducted on an outpatient basis, under a new program that took effect on July 1, 2020. This applies to a limited number of hospital outpatient department (OPD) services. The following hospital OPD services will require prior authorization, ...
Do you need a preauthorization for Medicare?
For the overwhelming majority of healthcare services under original Medicare, pre-author izations are not required. Pre-authorizations can be used to deter fraud with respect to durable medical equipment. Pre-authorizations have recently been introduced to certain hospital procedures conducted on an outpatient basis, ...
Can pre-authorizations be difficult?
For pre-Medicare health insurance policy owners, pre-authorizations by an insurance carrier, prior to many healthcare services, is standard practice. In many cases, pre-authorizations can be difficult to obtain, and/or policyholders can experience delays in receiving services.
Does Medicare require pre-authorization?
For the overwhelming majority of healthcare services under original Medicare, pre-authorizations are not required.
What services require pre-certification?
For example, services that may require pre-certification include outpatient and inpatient hospital services, observation services, invasive procedures, CT, MRI and PET scans, and colonoscopies. Patients are responsible for knowing the pre-certification requirements of their health plans. Mayo Clinic highly recommends that you contact your insurance ...
Can you get a reduced insurance payment if you have not been authorized?
Patients' plans that require prior authorization or pre-certification may provide only a reduced insurance payment if not previously authorized. In such cases, the patient will be financially responsible for more — possibly all — of the provided services. A pre-service deposit may be required for nonauthorized visits.
Does Mayo Clinic cover pre-certification?
Your Mayo Clinic doctor will decide which procedures, tests and other consultations you may need. However, many health plans require pre-certification and sometimes predetermination of medical necessity prior to care being rendered. In addition, some services may not be a covered benefit for some plans. Investigating coverage requirements and ...
Do you need a pre-service deposit for Mayo Clinic?
A pre-service deposit may be required for nonauthorized visits. To avoid paying a pre-service deposit or experiencing either denial of payment or a reduction of benefits, Mayo Clinic highly recommends you contact your insurance carrier prior to services to determine plan requirements or limitations to receiving care at the Mayo Clinic site ...
