The best way to know which one you have is to call the number on the back of your insurance card. In some cases, it’s possible for someone to have both Medicare AND Medicaid. In order to enroll in both programs, the individual must meet the eligibility requirements for both programs.
How to confirm Medicaid benefits?
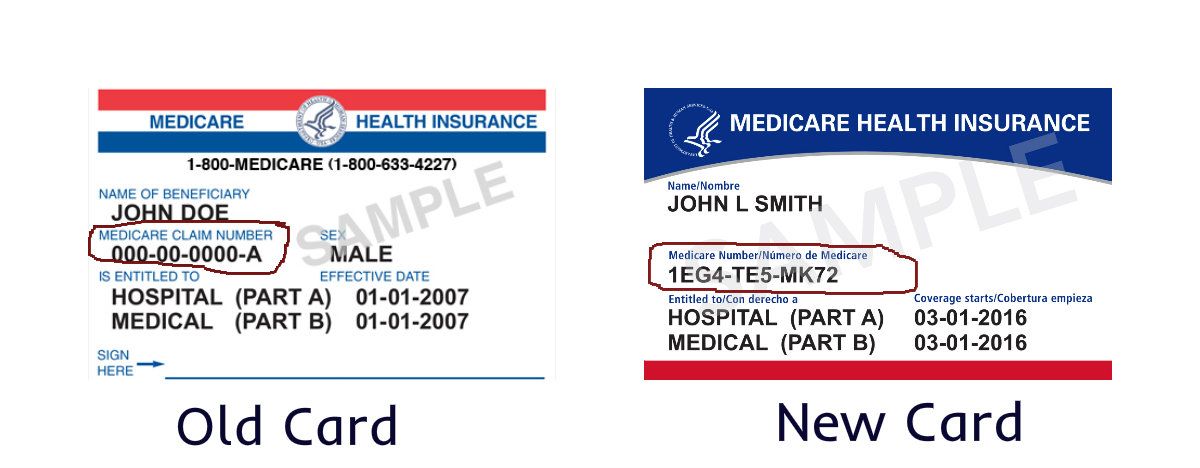
Apr 06, 2022 · Since Medicare is a national program, all Medicare insurance cards look the same. Here’s an example: People with Medicare Advantage will have two insurance cards: One for traditional Medicare, and one for their Medicare Advantage plan. Medicare Advantage cards will look different from each other, depending on the plan.
How do you get approved for Medicaid?
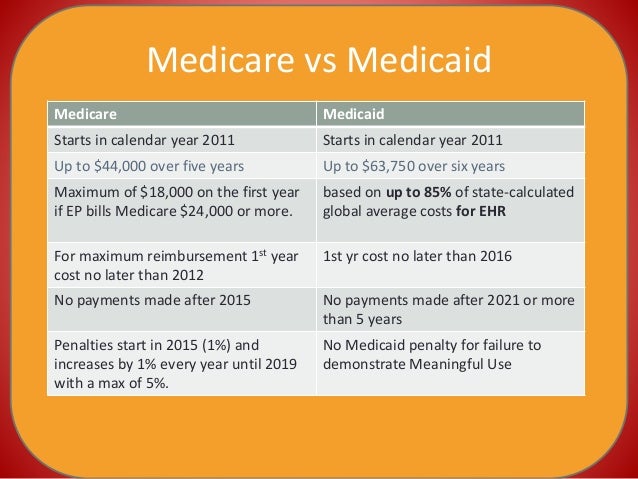
Aug 27, 2017 · Medicare and Medicaid have similar benefits and coverages but some people might have dual eligibility. This means that they qualify for both programs. If you are dually eligible, it is beneficial to coordinate the two programs. This way, they will cover your medical bills and hospital stays.
How can I Check my Medicaid status online?
In this case, you're eligible for Medicaid because you're considered "medically needy." To be eligible as "medically needy," your measurable resources must also be under the resource amount allowed in your state. Call your state Medicaid program to see if you qualify and learn how to apply. Dual eligibility. If you have Medicare and full Medicaid coverage, most of your health …
How can you look up your Medicaid number?
You can see if you qualify for Medicaid 2 ways: Visit your state's Medicaid website. Use the drop-down menu at the top of this page to pick your state. You can apply right now and find out if you qualify. If you qualify, coverage can begin immediately. Fill out an application in the Health Insurance Marketplace.
How can you tell the difference between Medicaid and Medicare?
The easiest way to remember the difference between is Medicare is Medicaid largely supports people over 65 and Medicaid largely supports those with lower-income.Dec 13, 2013
How do you know if you have Medicare?
You will know if you have Original Medicare or a Medicare Advantage plan by checking your enrollment status. Your enrollment status shows the name of your plan, what type of coverage you have, and how long you've had it. You can check your status online at www.mymedicare.gov or call Medicare at 1-800-633-4227.
How do you know if you have Medicaid?
You can see if you qualify for Medicaid 2 ways:Visit your state's Medicaid website. Use the drop-down menu at the top of this page to pick your state. ... Fill out an application in the Health Insurance Marketplace. When you finish the application, we'll tell you which programs you and your family qualify for.
How do I know if I am automatically enrolled in Medicare?
You'll be automatically enrolled in Medicare Part A and Part B: If you are already getting benefits from Social Security or the Railroad Retirement Board. If you are younger than 65 and have a disability. If you have Lou Gehrig's disease, also called Amyotrophic Lateral Sclerosis, or ALS.Jan 28, 2020
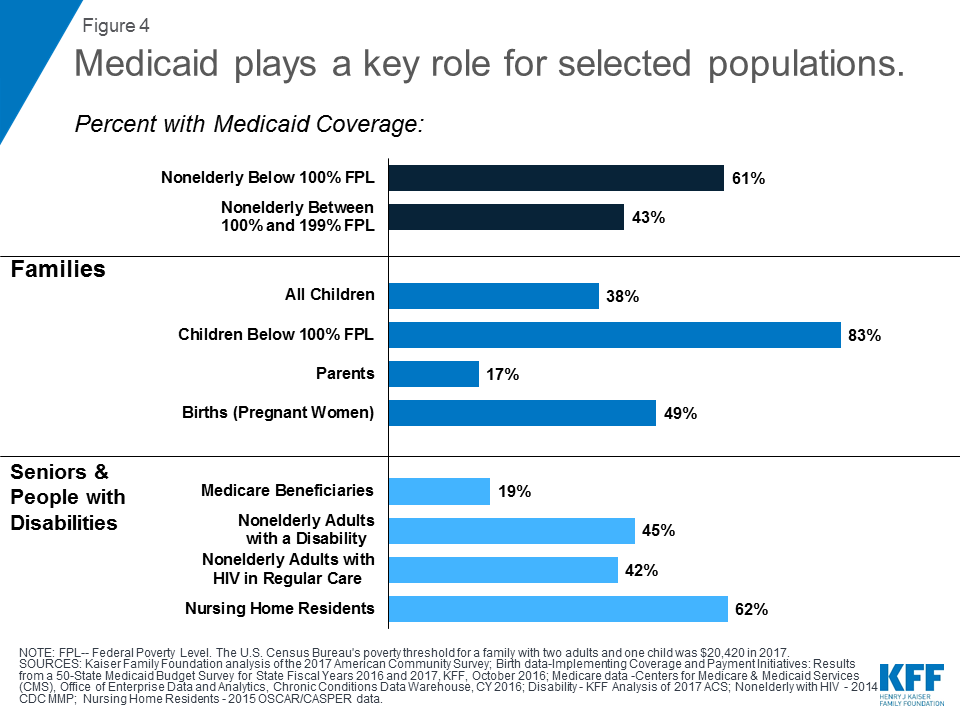
What is the purpose of poverty level?
This measurement helps determine who is eligible for certain programs and benefits. The federal poverty level plays a role in eligibility and Medicaid services.
What are the requirements for Medicaid?
Medicaid eligibility is available to low-income families, pregnant women, children, the elderly, people with disabilities, and those who receive Supplemental Security Income (SSI). Because this program has firm income eligibility requirements, laws for eligibility vary depending upon the state in which you live. Typically, eligibility follows the following criteria: 1 Applicants must meet federal and state requirements including residency, immigration status, and proof of citizenship 2 Applicants must meet financial need requirements on both federal and state levels
What is original Medicare?
Original Medicare is the standard Medicare program that the federal government offers. The government will directly pay for any health care services you receive. You can see any doctor or hospital that accepts Medicare. Here's how it works:
When does Medicare open?
Enrollment for Medicare is only open during certain times. In some cases, folks automatically enroll in Medicare when they turn 65. Some people are even automatically enrolled in Medicare when they turn 65. The 7 Month Initial Enrollment Period starts 3 months before turning 65, includes your birthday month, and ends 3 months after turning 65. It is important to know about all of your options so that when the time comes you know just what you want before applying for Medicare through Social Security.
What is the role of the primary payer in medical insurance?
The primary payer pays for your medical bills and then sends the remaining amount to the second payer.
How old do you have to be to get medicare?
Medicare is available to any US citizen or permanent legal resident who has been in the US for at least 5 years and is at least 65 years old. In certain situations, it also may cover people with disabilities. For those who are younger than 65 to be eligible for Medicare you must:
Is Medicare and Medicaid the same?
Medicare and Medicaid have similar benefits and coverages but some people might have dual eligibility. This means that they qualify for both programs. If you are dually eligible, it is beneficial to coordinate the two programs. This way, they will cover your medical bills and hospital stays.
What is extra help?
And, you'll automatically qualify for. Extra Help. A Medicare program to help people with limited income and resources pay Medicare prescription drug program costs, like premiums, deductibles, and coinsurance. paying for your.
Which pays first, Medicare or Medicaid?
Medicare pays first, and. Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources. Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid. pays second.
What is original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). or a.
Does Medicare cover prescription drugs?
. Medicaid may still cover some drugs and other care that Medicare doesn’t cover.
Does Medicare have demonstration plans?
Medicare is working with some states and health plans to offer demonstration plans for certain people who have both Medicare and Medicaid and make it easier for them to get the services they need. They’re called Medicare-Medicaid Plans. These plans include drug coverage and are only in certain states.
Does Medicare Advantage cover hospice?
Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Most Medicare Advantage Plans offer prescription drug coverage. . If you have Medicare and full Medicaid, you'll get your Part D prescription drugs through Medicare.
Can you get medicaid if you have too much income?
Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid. The "spend down" process lets you subtract your medical expenses from your income to become eligible for Medicaid. In this case, you're eligible for Medicaid because you're considered "medically needy."
How much does Medicare Part B cost?
For Medicare Part B (medical insurance), enrollees pay a monthly premium of $148.50 in addition to an annual deductible of $203. In order to enroll in a Medicare Advantage (MA) plan, one must be enrolled in Medicare Parts A and B. The monthly premium varies by plan, but is approximately $33 / month.
What is Medicare and Medicaid?
Differentiating Medicare and Medicaid. Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. Since it can be easy to confuse the two terms, Medicare and Medicaid, it is important to differentiate between them. While Medicare is a federal health insurance program ...
What is dual eligible?
Definition: Dual Eligible. To be considered dually eligible, persons must be enrolled in Medicare Part A, which is hospital insurance, and / or Medicare Part B, which is medical insurance. As an alternative to Original Medicare (Part A and Part B), persons may opt for Medicare Part C, which is also known as Medicare Advantage.
What is the income limit for Medicaid in 2021?
In most cases, as of 2021, the individual income limit for institutional Medicaid (nursing home Medicaid) and Home and Community Based Services (HCBS) via a Medicaid Waiver is $2,382 / month. The asset limit is generally $2,000 for a single applicant.
How old do you have to be to qualify for medicare?
Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare. Applicants must also be at least 65 years old. For persons who are disabled or have been diagnosed with end-stage renal disease or Lou Gehrig’s disease (amyotrophic lateral sclerosis), there is no age requirement. Eligibility for Medicare is not income based. Therefore, there are no income and asset limits.
How to apply for medicaid?
How to Apply. To apply for Medicare, contact your local Social Security Administration (SSA) office. To apply for Medicaid, contact your state’s Medicaid agency. Learn about the long-term care Medicaid application process. Prior to applying, one may wish to take a non-binding Medicaid eligibility test.
Does Medicare provide long term care?
Long-Term Care Benefits. Medicaid provides a wide variety of long-term care benefits and supports to allow persons to age at home or in their community. Medicare does not provide these benefits, but some Medicare Advantage began offering various long term home and community based services in 2019. Benefits for long term care may include ...
What is Medicaid Spousal Impoverishment?
Spousal Impoverishment : Protects the spouse of a Medicaid applicant or beneficiary who needs coverage for long-term services and supports (LTSS), in either an institution or a home or other community-based setting, from becoming impoverished in order for the spouse in need of LTSS to attain Medicaid coverage for such services.
What is dual eligible for Medicare?
Eligibility for the Medicare Savings Programs, through which Medicaid pays Medicare premiums, deductibles, and/or coinsurance costs for beneficiaries eligible for both programs (often referred to as dual eligibles) is determined using SSI methodologies..
What is MAGI for Medicaid?
MAGI is the basis for determining Medicaid income eligibility for most children, pregnant women, parents, and adults. The MAGI-based methodology considers taxable income and tax filing relationships to determine financial eligibility for Medicaid. MAGI replaced the former process for calculating Medicaid eligibility, ...
What is 209b spending?
In addition to states with medically needy programs, 209 (b) states also must allow a spenddown to the income eligibility levels eligibility groups based on blindness, disability, or age (65 and older), even if the state also has a medically needy program. Thirty-six states and the District of Columbia use spenddown programs, ...
What is Medicaid coverage?
Medicaid is the single largest source of health coverage in the United States. To participate in Medicaid, federal law requires states to cover certain groups of individuals. Low-income families, qualified pregnant women and children, and individuals receiving Supplemental Security Income (SSI) are examples of mandatory eligibility groups (PDF, ...
How long does medicaid last?
Benefits also may be covered retroactively for up to three months prior to the month of application, if the individual would have been eligible during that period had he or she applied. Coverage generally stops at the end of the month in which a person no longer meets the requirements for eligibility.
How many people are covered by medicaid?
Medicaid is a joint federal and state program that, together with the Children’s Health Insurance Program (CHIP), provides health coverage to over 72.5 million Americans, including children, pregnant women, parents, seniors, and individuals with disabilities. Medicaid is the single largest source of health coverage in the United States.
What is the difference between Medicare and Medicaid?
The benefit is the plan will have very low copays and very few additional fees. Medicare is for those aged 65 and older or those with disabilities or specific medical conditions. Medicaid is for people of any age, with or without medical conditions, so long as they meet the state’s economic conditions.
How are Medicare premiums paid?
Premiums are typically paid on a monthly basis. In the federal Medicare program, there are four different types of premiums. ... , deductibles, copays, and more. Medicaid assists with these costs, but you may be required to use an approved Medicaid health plan.
What percentage of Medicare beneficiaries are eligible for Medicaid?
Around 20 percent of Medicare beneficiaries are also eligible for Medicaid. They are called dual-eligible. You would need to apply for each one separately to determine if you can qualify for both. Dual-eligibles are categorized based on whether they receive full or partial Medicaid benefits.
What percentage of Medicare is covered by deductible?
In fact, from the beginning, Medicare was designed to cover only about 80 percent of a beneficiary’s major medical expenses. All other costs, typically in the form of deductibles. A deductible is an amount a beneficiary must pay for their health care expenses before the health insurance policy begins to pay its share....
What is Medicare Part B?
If not, you will pay a monthly premium for Part A. With Part B. Medicare Part B is medical coverage for people with Original Medicare. It covers doctor visits, specialists, lab tests and diagnostics, and durable medical equipment. Part A is for hospital inpatient care....
How can low income people get help with prescriptions?
The first and most important way is to apply for the Social Security Administration’s Extra Help program . This program provides low-income subsidies (LIS) to those who need them.
How old do you have to be to get Medicare?
Since Medicare is a government insurance program, anyone aged 65 or older can apply and receive insurance through this program.
How long does Medicare AEP last?
The Medicare AEP lasts from October 15 to December 7 every year. During this time, Medicare beneficiaries may do any of the following: Change from Original Medicare to a Medicare Advantage plan. Change from Medicare Advantage back to Original Medicare. Switch from one Medicare Advantage plan to another.
What are the benefits of Medicare Advantage?
Most Medicare Advantage plans offer additional benefits not covered by Original Medicare, such as dental, vision and prescription drug coverage. Medicare Part D provides coverage for prescription medications, which is something not typically covered by Original Medicare.
What is an annual review of Medicare?
An annual review of your Medicare coverage can help you determine if your plan combination is right for your needs. For example, if you’re spending a considerable amount of money on prescription drugs, a Medicare Part D plan or a Medicare Advantage plan with prescription drug coverage may be something to consider.
What is Medicare Part B?
Medicare Part B is medical insurance and provides coverage for outpatient appointments and durable medical equipment. Part B is optional, but is required for anyone wanting to enroll in Medicare Part C, Part D or Medicare Supplement Insurance. Part A and Part B are known together as “Original ...
Is Medicare Part A and Part B the same?
Part A and Part B are known together as “Original Medicare.”. Medicare Part C, also known as Medicare Advantage, provides all the same benefits as Medicare Part A and Part B combined into a single plan sold by a private insurance company.
Who is Christian Worstell?
Christian Worstell is a licensed insurance agent and a Senior Staff Writer for MedicareAdvantage.com. He is passionate about helping people navigate the complexities of Medicare and understand their coverage options. .. Read full bio
What is a dual eligible special needs plan?
If you are dual eligible, you are can enroll in a dual eligible special needs plan (D-SNP) that covers both Medicare and Medicaid benefits. These plans may also pay for expenses that Medicare and Medicaid don’t over individually, including over-the-counter items, hearing aids, and vision or dental care. Beneficiaries who are dual eligible can ...
What is dual eligible Medicare?
Beneficiaries with Medicare and Medicaid are known as dual eligibles – and account for about 20 percent of Medicare beneficiaries (12.1 million people). Dual eligibles are categorized based on whether they receive partial or full Medicaid benefits. Full-benefit dual eligibles have comprehensive Medicaid coverage, ...
Is Medicare the same as Medicaid?
The federal government oversees Medicare eligi bility – meaning it is the same in each state. But states set their own eligibility rules for Medicaid and the MSPs (within federal guidelines) – and income limits for these programs vary widely.
Do seniors qualify for medicaid?
Many seniors who live in nursing homes are dual eligible: they qualify for Medicare based on their age, and Medicaid because of their financial circumstances.
Does Medicare cover long term care?
But this is not the case for things Medicare doesn’t cover, like long-term care . If Medicaid is covering a beneficiary’s long-term care, Medicare will still be the primary payer for any Medicare-covered services – like skilled nursing care or physical therapy.
Who is Josh Schultz?
Josh Schultz has a strong background in Medicare and the Affordable Care Act. He coordinated a Medicare ombudsman contract at the Medicare Rights Center in New York City, and represented clients in extensive Medicare claims and appeals.