
To pay your bill, you can: Log into (or create) your secure Medicare account. Sign up for Medicare Easy Pay. Check if your bank offers an online bill payment service to pay electronically from your savings or checking account. Mail your payment by check, money order, credit card, or debit card (using the coupon on your bill)
Can I bill Medicare for a new pessary?
Mar 01, 2001 · The ob/gyn orders the pessary from a private medical supplier and submits the bill to the DMERC. If you dont have a supplier number you cannot bill the DMERC for the pessary supply says Melanie Witt RN CPC MA ob/gyn coding expert and an independent coding educator based in Fredericksburg Va. Likewise you cannot obtain the pessary from a supplier sell it to …
What is the CPT code for pessary insertion?
Mar 05, 2010 · If this is your first visit, be sure to check out the FAQ & read the forum rules. To view all forums, post or create a new thread, you must be an AAPC Member. If you are a member and have already registered for member area and forum access, you can log in by clicking here. If you've forgotten your username or password use our password reminder ...
How does Medicare bill my doctor?
Feb 09, 2022 · Billing for the Pessary Itself: Bill in addition for the pessary itself if it is provided by the practice. There are two durable medical equipment codes for a pessary. A4561 is for a rubber pessary and A4562 is for a non-rubber pessary.
How do you choose a pessary for a patient?
Jan 06, 2018 · On vaginal exam, you note a shallow epithelial ulcer without bleeding. You recommend trial of a smaller pessary. You place a #1 gellhorn and ask the patient to strain. With straining the pessary is extruded from the vagina. Next you try a #2 gellhorn. The patient strains and the pessary remains in place. You then ask the patient to ambulate in
How do I bill Medicare for a pessary?
Are pessaries covered by Medicare?
What is the CPT code for pessary?
What is the ICD 10 code for pessary fitting?
What is the ICD 10 code for uterine prolapse?
N81. 4 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is code A4562?
A4562 is a valid 2022 HCPCS code for Pessary, non rubber, any type or just “Pessary, non rubber,any type” for short, used in Lump sum purchase of DME, prosthetics, orthotics.Jan 1, 2001
Can you bill for pessary cleaning?
What is the ICD 10 code for Cystocele?
What is a pessary check?
Is DME a pessary?
How do you insert a Gellhorn pessary?
How long does it take for Medicare to pay?
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020.
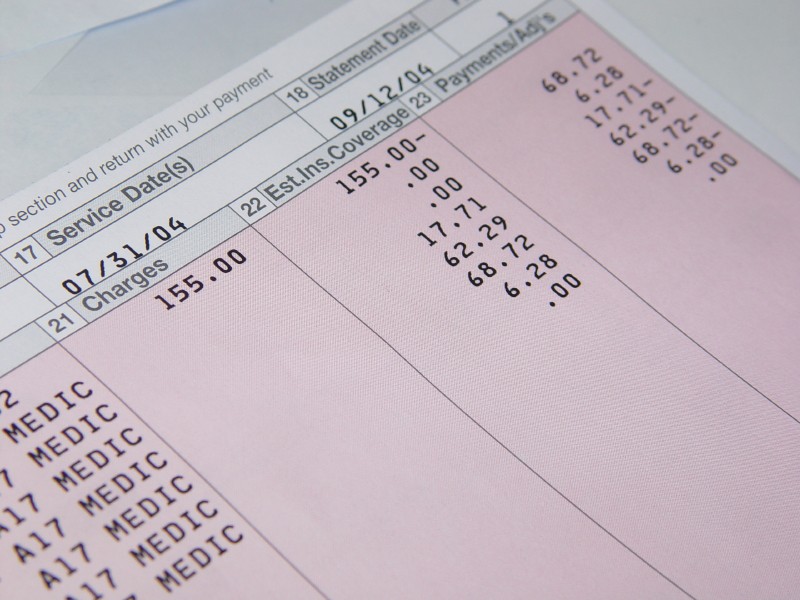
What is an itemized bill?
The itemized bill from your doctor, supplier, or other health care provider. A letter explaining in detail your reason for submitting the claim, like your provider or supplier isn’t able to file the claim, your provider or supplier refuses to file the claim, and/or your provider or supplier isn’t enrolled in Medicare.
How to file a medical claim?
Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1 The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2 The itemized bill from your doctor, supplier, or other health care provider 3 A letter explaining in detail your reason for submitting the claim, like your provider or supplier isn’t able to file the claim, your provider or supplier refuses to file the claim, and/or your provider or supplier isn’t enrolled in Medicare 4 Any supporting documents related to your claim
Does Medicare Advantage cover hospice?
Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Most Medicare Advantage Plans offer prescription drug coverage. , these plans don’t have to file claims because Medicare pays these private insurance companies a set amount each month.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
What is a pessary for?
A pessary is used to treat pelvic organ prolapse and for urinary incontinence. It provides support for the vaginal walls or uterus. A physician or non-physician practitioner (NPP) must first see the patient, take a history, examine the patient and decide if a pessary is the correct treatment.
What is the modifier code for E/M?
If both the evaluation, fitting and the insertion are done on the same calendar day, report both. Report the E/M service with modifier -25 and code 57160. The same diagnosis may be used for both services.
Can a psychologist bill Medicare for 90863?
Designed to allow prescribing psychologists to bill for pharmacologic management, code 90863 cannot yet be reported by psychologists when treating Medicare beneficiaries. Medicare, which does not have a separate category for prescribing psychologists, does not recognize prescribing or monitoring medication as part of a psychologist’s scope of practice. Code 90863 is an add-on code that captures prescribing and reviewing medication and must be billed along with a code for a psychotherapy service.
Does Medicare cover depression screening?
Medicare makes a limited number of screening services available to beneficiaries at no cost. Depression screening: Medicare covers one depression screening per year if the screening is done in a primary care setting (such as a physician’s office) that can provide follow-up treatment and referrals.
Does Medicare cover psychotherapy?
Medicare covers a psychiatric diagnostic interview, inpatient and outpatient psychotherapy services, psychotherapy for crisis situations and psychoanalysis. There are a number of different procedure codes for the various types of psychotherapy (i.e., individual, family, group) and MACs may have LCDs that set certain restrictions ...
What is an add on code?
Add-on codes identify an additional part of the treatment above and beyond the principal service . Both the principal service code and add-on code should be listed on the billing form.
What are complicating factors?
Complicating factors include, for example, difficult communication with acrimonious family members and engagement of verbally undeveloped children. These factors are typically found with patients who: Have others legally responsible for their care, such as minors or adults with guardians.
What is crisis psychotherapy?
Psychotherapy for Crisis. A crisis psychotherapy session requires urgent assessment and history of the crisis state, mental status exam and disposition. To be considered crisis psychotherapy, the presenting problem must be life-threatening or complex and require immediate attention to a patient in high distress.
What is the 90863 code?
Code 90863 is an add-on code that captures prescribing and reviewing medication and must be billed along with a code for a psychotherapy service. Outside of Medicare, 90863, pharmacologic management, including prescription and review of medication, when performed with psychotherapy services can be used only as add-on to primary psychotherapy ...
What is Medicare beneficiary?
The Medicare beneficiary when the beneficiary has obtained a settlement, judgment, award or other payment. The liability insurer (including a self-insured entity), no-fault insurer, or workers’ compensation (WC) entity when that insurer or WC entity has ongoing responsibility for medicals (ORM). For ORM, there may be multiple recoveries ...
How long does it take to appeal a debt?
The appeal must be filed no later than 120 days from the date the demand letter is received. To file an appeal, send a letter explaining why the amount or existence of the debt is incorrect with applicable supporting documentation.
Do you have to ask for reimbursement from Medicare?
If you are in a Medicare Advantage plan, you will never have to ask for reimbursement from Medicare. Medicare pays Advantage companies to handle the claims. In some cases, you may need to ask the company to reimburse you. If you see a doctor in your plan’s network, your doctor will handle the claims process.
Does Medicare reimburse doctors?
Medicare Reimbursement for Physicians. Doctor visits fall under Part B. You may have to seek reimbursement if your doctor does not bill Medicare. When making doctors’ appointments, always ask if the doctor accepts Medicare assignment; this helps you avoid having to seek reimbursement.
Does Medicare cover nursing home care?
Your doctors will usually bill Medicare, which covers most Part A services at 100% after you’ve met your deductible.
Does Medicare cover out of network doctors?
Coverage for out-of-network doctors depends on your Medicare Advantage plan. Many HMO plans do not cover non-emergency out-of-network care, while PPO plans might. If you obtain out of network care, you may have to pay for it up-front and then submit a claim to your insurance company.
How long does it take for Medicare to process a claim?
Medicare claims to providers take about 30 days to process. The provider usually gets direct payment from Medicare. What is the Medicare Reimbursement fee schedule? The fee schedule is a list of how Medicare is going to pay doctors. The list goes over Medicare’s fee maximums for doctors, ambulance, and more.
Who is Lindsay Malzone?
Lindsay Malzone is the Medicare expert for MedicareFAQ. She has been working in the Medicare industry since 2017. She is featured in many publications as well as writes regularly for other expert columns regarding Medicare.
How to pay Medicare premiums?
Follow the instructions on the bill to pay the total amount due, so Medicare gets your payment by the 25th of the month. To pay your bill, you can: 1 Log into (or create) your secure Medicare account to pay by credit card or debit card 2 Sign up for Medicare Easy Pay, a free service that automatically deducts your premium payments from your savings or checking account each month 3 See if your bank offers an online bill payment service to pay electronically from your savings or checking account 4 Mail your payment by check, money order, credit card, or debit card (using the coupon on your bill)
What is the April bill?
If you get a bill each month, the bill you get in April is for May coverage. If you get a bill every 3 months, the bill you get in April is for May, June, and July coverage. Your bill may also include premiums for past months if you missed a payment, if you're getting your first bill, or if you had a change in your premium amount.
Is Medicare the primary payer?
Medicare remains the primary payer for beneficiaries who are not covered by other types of health insurance or coverage. Medicare is also the primary payer in certain instances, provided several conditions are met.
What is Medicare Secondary Payer?
Medicare Secondary Payer (MSP) is the term generally used when the Medicare program does not have primary payment responsibility - that is, when another entity has the responsibility for paying before Medicare. When Medicare began in 1966, it was the primary payer for all claims except for those covered by Workers' Compensation, ...
When did Medicare start?
When Medicare began in 1966 , it was the primary payer for all claims except for those covered by Workers' Compensation, Federal Black Lung benefits, and Veteran’s Administration (VA) benefits.
What is ESRD in Medicare?
End-Stage Renal Disease (ESRD): Individual has ESRD, is covered by a GHP and is in the first 30 months of eligibility or entitlement to Medicare. GHP pays Primary, Medicare pays secondary during 30-month coordination period for ESRD. Individual has ESRD, is covered by a Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA plan) ...
How long does ESRD last on Medicare?
Individual has ESRD, is covered by a GHP and is in the first 30 months of eligibility or entitlement to Medicare. GHP pays Primary, Medicare pays secondary during 30-month coordination period for ESRD.
Why is Medicare conditional?
Medicare makes this conditional payment so that the beneficiary won’t have to use his own money to pay the bill. The payment is “conditional” because it must be repaid to Medicare when a settlement, judgment, award or other payment is made. Federal law takes precedence over state laws and private contracts.
What is the purpose of MSP?
The MSP provisions have protected Medicare Trust Funds by ensuring that Medicare does not pay for items and services that certain health insurance or coverage is primarily responsible for paying. The MSP provisions apply to situations when Medicare is not the beneficiary’s primary health insurance coverage.

When Do I Need to File A Claim?
- You should only need to file a claim in very rare cases
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicar… - If your claims aren't being filed in a timely way:
1. Contact your doctor or supplier, and ask them to file a claim. 2. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got. If it's close to the end of the time limit and yo…
How Do I File A Claim?
- Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
What Do I Submit with The Claim?
- Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1. The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2. The itemized bill from your doctor, supplier, or other health care provider 3. A letter explaining ...
Where Do I Send The Claim?
- The address for where to send your claim can be found in 2 places: 1. On the second page of the instructions for the type of claim you’re filing (listed above under "How do I file a claim?"). 2. On your "Medicare Summary Notice" (MSN). You can also log into your Medicare accountto sign up to get your MSNs electronically and view or download them anytime. You need to fill out an "Author…