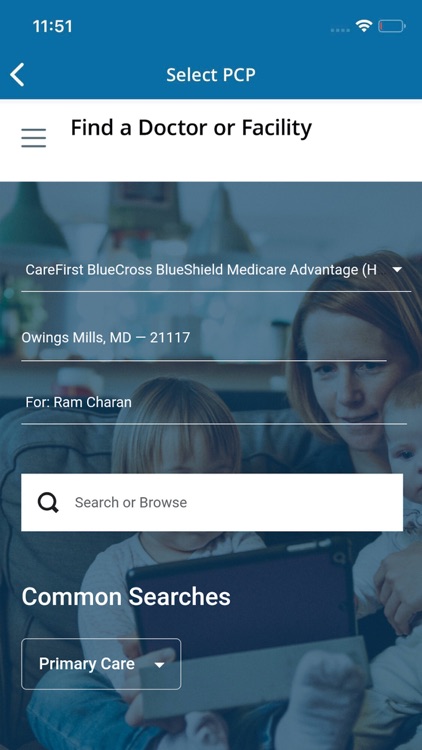
Medicare Advantage HMOs are based around in-network medical care. This means that you are given a list of in-network providers to choose from when you need medical services. If you decide to select a provider who is out of network, you may owe a higher cost or the full out-of-pocket amount for those services.
Full Answer
Do Medicare Advantage plans cover home health care?
Medicare pays a fixed amount for your care each month to the companies offering Medicare Advantage Plans. These companies must follow rules set by Medicare. Each Medicare Advantage Plan can charge different out-of-pocket costs . They can also have different rules for how you get services, like: Whether you need a referral to see a specialist
What are the benefits of home state health plan?
How do Medicare Advantage Plans work? When you join a Medicare Advantage Plan, Medicare pays a fixed amount for your coverage each month to the company offering your Medicare Advantage Plan. Companies that offer Medicare Advantage …
What are the benefits of Ambetter from home state health?
Home health services Medicare Advantage and home health All Medicare Advantage Plans must provide at least the same level of home health care coverage as Original Medicare, but they may impose different rules, restrictions, and costs. Depending on your plan, you may need to: Get care from a home health agency (HHA) that contracts with your plan
How do Medicare Advantage plans work?
Oct 01, 2021 · Welcome to Wellcare By Allwell from Home State Health's new Medicare Advantage website. We are simplifying Medicare so you can choose and use an affordable local plan that will help you achieve your best possible health. Shop for a Plan. Drug Search Tool. Member Quick Start Guide.
What happens if you get a health care provider out of network?
If you get health care outside the plan’s network, you may have to pay the full cost. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed. In most cases, you need to choose a primary care doctor. Certain services, like yearly screening mammograms, don’t require a referral. If your doctor or other health care provider leaves the plan’s network, your plan will notify you. You may choose another doctor in the plan’s network. HMO Point-of-Service (HMOPOS) plans are HMO plans that may allow you to get some services out-of-network for a higher copayment or coinsurance. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed.
What is a special needs plan?
Special Needs Plan (SNP) provides benefits and services to people with specific diseases, certain health care needs, or limited incomes. SNPs tailor their benefits, provider choices, and list of covered drugs (formularies) to best meet the specific needs of the groups they serve.
Can a provider bill you for PFFS?
The provider shouldn’t provide services to you except in emergencies, and you’ll need to find another provider that will accept the PFFS plan .However, if the provider chooses to treat you, then they can only bill you for plan-allowed cost sharing. They must bill the plan for your covered services. You’re only required to pay the copayment or coinsurance the plan allows for the types of services you get at the time of the service. You may have to pay an additional amount (up to 15% more) if the plan allows providers to “balance bill” (when a provider bills you for the difference between the provider’s charge and the allowed amount).
Do providers have to follow the terms and conditions of a health insurance plan?
The provider must follow the plan’s terms and conditions for payment, and bill the plan for the services they provide for you. However, the provider can decide at every visit whether to accept the plan and agree to treat you.
What are the benefits of Medicare Advantage?
Some Medicare Advantage plans may offer an expanded list of benefits that include: 1 Transportation to doctor's appointments 2 Grab bars in home bathrooms 3 Healthier food options 4 Air conditioners for people with asthma 5 Home-delivered meals 6 Home health aides to help with daily activities like dressing or eating 7 Caregiver support services
What is home health aide?
Home health aides to help with daily activities like dressing or eating. Caregiver support services. Call today to speak with a licensed insurance agent who can help you compare Medicare Advantage plans that are available where you live. You may be able to find a plan that covers home health care, caregiver support and more.
What is part time skilled nursing?
Part-time skilled nursing care. Physical therapy, speech-language pathology, or occupational therapy services. Home health services are only covered by Medicare when they are specific, safe and an effective treatment for your health condition.
Who is Christian Worstell?
Christian Worstell is a licensed insurance agent and a Senior Staff Writer for MedicareAdvantage.com. He is passionate about helping people navigate the complexities of Medicare and understand their coverage options. .. Read full bio
What is part time home health aide?
Part-time home health aide care. Medical social services. Physical and occupational therapy. Speech-language pathology services. Home health services are typically covered only if they are considered medically necessary by your doctor. A home health care agency can help you coordinate your home health services.
Does Medicare cover assisted living?
Although the housing cost charged by an assisted living facility will not be covered by Medicare, residents of assisted living homes can still benefit from Medicare coverage for certain services.
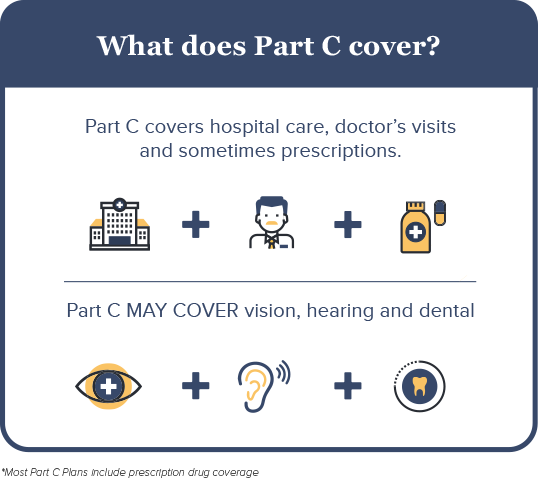
What are the different Medicare Parts?
Medicare Parts A, B, C, and D all give you different kinds of benefits and can combine in different ways. To top it off, some plans have multiple titles. For instance, Medicare Parts A and B are collectively known as Original Medicare; Medicare Part C is commonly called Medicare Advantage.
Is Medicare Advantage the same as Medicare Part B?
Medicare Advantage plans are required to offer the same benefits as Medicare Part A and Medicare Part B plans.⃰ But whereas Part A and Part B offer a fixed set of benefits based on government regulations, Medicare Advantage plans can offer any additional benefits the private insurance company chooses.
Can Medicare be used out of state?
While some Medicare Advantage plans can be used out of state, these plans usually don’t provide coverage outside of the U.S. Seniors who are traveling out of the country may choose to purchase travel medical insurance. In limited circumstances, Medicare Advantage plans provide coverage outside of the U.S. For example, if seniors are traveling ...
Does Medicare cover travel?
Some Medicare Advantage plans provide special coverage for travelers. These benefits may be called visitor or travel benefits, depending on the plan. Seniors who are enrolled in these plans may be able to use their coverage outside of their home state.
Do seniors need to see doctors?
Generally, seniors need to see doctors who are in their Medicare Advantage plan’s network. Before traveling out of state, seniors should contact their plan to find out if there are any in-network providers at their destination. Seniors who see out-of-network providers may need to pay the full cost of any services they receive.
Is Medicare available in all 50 states?
Search. Page Reviewed / Updated – August 11, 2020. Original Medicare can be used in all 50 states, as well as in the District of Columbia, American Samoa, Guam, the Northern Mariana Islands, Puerto Rico and the Virgin Islands. The same isn’t true for Medicare Advantage plans. These plans have defined service areas and may not cover out-of-state ...
