How does Medicare calculate secondary payment?
Jan 22, 2020 · Medicare qualifications The formula for determining a person’s qualification for Social Security and Medicare is the same. It is based on income earned and taxes paid for the duration of working life. The annual W-2 Form that U.S. employees receive includes not only year-to-date earnings but also taxes paid toward Social Security and Medicare.
How much Medicare tax do I pay?
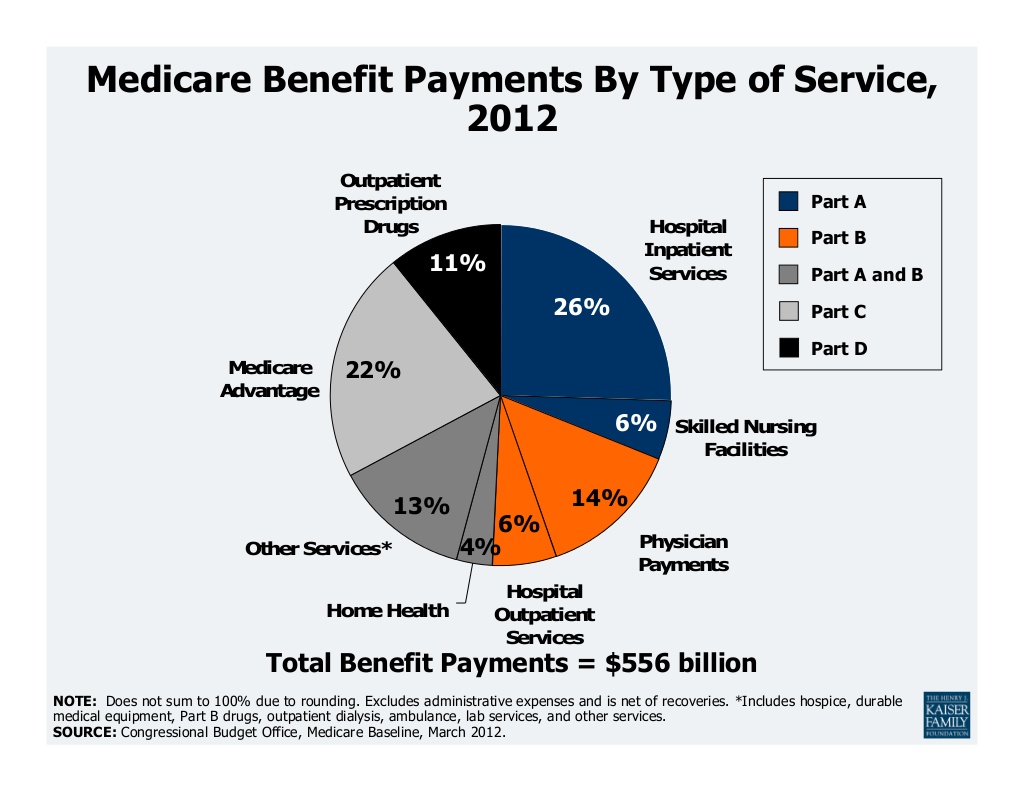
Dec 21, 2021 · Most of Medicare Part B – about 7% – is funded through U.S. income tax revenue. But the remaining 25% of Medicare Part B expenses are paid through your premium, which is determined by your income level. Medicare prices are quoted under the assumption you have an average income.
How does Medicare calculate my premium?
Feb 15, 2022 · Medicare Part B premiums are calculated based on your income. More specifically, they’re based on the modified adjusted gross income (MAGI) reported on your taxes from two years prior. This means your 2021 Medicare Part B premium may be calculated using the income you reported on your 2019 taxes.
How is a Medicare Secondary payment determined FAQ?
The establishment rate schedules are complex, multifunctional, and revised annually. The schedules for Medicare reimbursement rates are pre-determined base rates developed using a variety of factors that include the following. • Type of service or equipment provided. • The type of medical professional or facility.
What determines Medicare reimbursement?
The Centers for Medicare and Medicaid (CMS) sets reimbursement rates for all medical services and equipment covered under Medicare. When a provider accepts assignment, they agree to accept Medicare-established fees. Providers cannot bill you for the difference between their normal rate and Medicare set fees.
What are the Medicare limits for 2021?
Medicare beneficiaries earning more than $88,000 and couples earning more than $176,000 were affected by the 2021 change. “Medicare's 2021 income limits and corresponding surcharges apply to all beneficiaries with part B and/or part D coverage,” Worstell tells Parade.Nov 1, 2021
How does Medicare pricing work?
Since 1992, Medicare has set prices using the Resource-Based Relative Value Scale (RBRVS), which calculates the estimated amount of work and practice expense involved in delivering specific services. The original purpose of the RBRVS was to bring physician prices more into line with the costs of providing services.Oct 8, 2015
How are reimbursement rates determined?
Payers assess quality based on patient outcomes as well as a provider's ability to contain costs. Providers earn more healthcare reimbursement when they're able to provide high-quality, low-cost care as compared with peers and their own benchmark data.
Is Medicare Part A free at age 65?
Most people age 65 or older are eligible for free Medical hospital insurance (Part A) if they have worked and paid Medicare taxes long enough. You can enroll in Medicare medical insurance (Part B) by paying a monthly premium. Some beneficiaries with higher incomes will pay a higher monthly Part B premium.
Does Social Security count as income for Medicare premiums?
Medicare premiums are based on your modified adjusted gross income, or MAGI. That's your total adjusted gross income plus tax-exempt interest, as gleaned from the most recent tax data Social Security has from the IRS.
How much does Medicare take out of Social Security?
What are the Medicare Part B premiums for each income group? In 2021, based on the average social security benefit of $1,514, a beneficiary paid around 9.8 percent of their income for the Part B premium. Next year, that figure will increase to 10.6 percent.Nov 22, 2021
Do I have to pay for Medicare Part A?
Most people don't pay a monthly premium for Part A (sometimes called "premium-free Part A"). If you buy Part A, you'll pay up to $499 each month in 2022. If you paid Medicare taxes for less than 30 quarters, the standard Part A premium is $499.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because the private insurance companies make it difficult for them to get paid for the services they provide.
Which of the following expenses would be paid by Medicare Part B?
Medicare Part B helps cover medically-necessary services like doctors' services and tests, outpatient care, home health services, durable medical equipment, and other medical services.Sep 11, 2014
Does Medicare pay more than billed charges?
Consequently, the billed charges (the prices that a provider sets for its services) generally do not affect the current Medicare prospective payment amounts. Billed charges generally exceed the amount that Medicare pays the provider.
How do hospitals negotiate prices with Medicare?
Medicare sets reimbursement rates for hospitals every year using the same formula that multiplies a base rate by a case mix adjustment and a hospital type adjustment then adding the outlier payments. Private payers, on the other hand, must negotiate hospital prices with providers, and the process is quite complex.May 13, 2019
How Are Medicare Premiums calculated?
Many individuals are wondering how medicare premiums are calculated. Medicare Part A is free to most beneficiaries and covers hospital stays, care...
How Is A Beneficiary’S Premium determined?
The Social Security Administration reviews a beneficiary’s most recent federal tax information in order to determine what their premium will be. Ba...
Beneficiary Premium Rates
Beneficiaries filing an individual tax return must pay a monthly premium of: 1. $146.90 with an income of $85,001-$107,000, 2. $209.80 with an inco...
How much of Medicare Part B is paid?
But the remaining 25% of Medicare Part B expenses are paid through your premium, which is determined by your income level. Medicare prices are quoted under the assumption you have an average income. If your income level exceeds a certain threshold, you will have to pay more.
What is Medicare Advantage?
Essentially: Medicare Advantage – Private plans that replace your Parts A, B, and in most cases, D. Also known as Part C. Medicare Part D – Prescription drug coverage plans, introduced in 2006. Generally, if you’re on Medicare, you aren’t charged a premium for Part A.
How much will Medicare premiums be in 2021?
There are six income tiers for Medicare premiums in 2021. As stated earlier, the standard Part B premium amount that most people are expected to pay is $148.50 month. But, if your MAGI exceeds an income bracket — even by just $1 — you are moved to the next tier and will have to pay the higher premium.
Why did Medicare Part B premiums increase in 2021?
That’s because 2021 Medicare Part B premiums increased across the board due to rising healthcare costs. Exactly how much your premiums increased though, isn’t based on your current health or Medicare plan or your income. Rather, it’s the soaring prices of overall healthcare.
What does IRMAA mean?
These additional Medicare premiums are all calculated through something called IRMAA, which stands for Income-Related Monthly Adjustment Amount. It is an additional amount that you may have to pay along with your Medicare premium if your modified adjusted gross income (MAGI) is higher than a certain threshold.
Why are Social Security beneficiaries paying less than the full amount?
In 2016, 2017, and 2018, the Social Security COLA amount for most beneficiaries wasn’t enough to cover the full cost of the Part B premium increases, so most enrollees were paying less than the full amount, because they were protected by the hold harmless rule.
How much is Part B 2021?
So most beneficiaries are paying the standard $148.50/month for Part B in 2021. The hold harmless provision does NOT protect you if you are new to Medicare and/or Social Security, not receiving Social Security benefits, or are in a high-income bracket.
How is Medicare Part B calculated?
Medicare Part B premiums are calculated based on your income. More specifically, they’re based on the modified adjusted gross income (MAGI) reported on your taxes from two years prior. This means your 2021 Medicare Part B premium may be calculated using the income you reported on your 2019 taxes. If your reported income was higher ...
How does Medicare Advantage work?
A Medicare Advantage plan could potentially help you save money on costs such as dental care, prescription drugs and other costs. A licensed insurance agent can help you compare the Medicare Advantage plans that are available where you live. You can compare benefits, coverage and the costs of each plan and then choose the right fit for your needs.
What is the late enrollment penalty for Medicare?
The Part A late enrollment penalty is 10 percent of the Part A premium, which you must pay for twice the number of years for which you were eligible for Part A but didn’t sign up. Medicare Part B. Medicare Part B is optional coverage, but if you don’t sign up when you’re first eligible, your late enrollment penalty will be calculated based on how ...
How much will Medicare pay in 2021?
If you paid Medicare taxes for fewer than 30 quarters, you will pay $471 per month for Part A in 2021.
What is the penalty for not enrolling in Part A?
The Part A late enrollment penalty is 10 percent ...
Does Medicare Advantage have a monthly premium?
Some Medicare Advantage plans offer $0 monthly premiums and $0 deductibles, and all Medicare Advantage plans must include an annual out-of-pocket cost limit. $0 premium plans may not be available in all locations.
Do high income people pay higher Medicare premiums?
Learn about other Medicare costs and how they are calculated. If you are a high-income earner, you could potentially pay higher premiums for Medicare Part B (medical insurance) and Medicare prescription drug coverage.
How much does Medicare pay for medical services?
The Medicare reimbursement rates for traditional medical procedures and services are mostly established at 80 percent of the cost for services provided. Some medical providers are reimbursed at different rates. Clinical nurse specialists are paid 85 percent for most of their billed services and clinical social workers are paid 75 percent ...
What is the original objective of Medicare?
The original objective was to establish a uniform payment system to minimize disparities between varying usual, customary, and reasonable costs. Today, Medicare enrollees who use the services of participating health care professionals will be responsible for the portion of a billing claim not paid by Medicare.
How many specialists are on the Medicare committee?
Medicare establishes the reimbursement rates based on recommendations from a select committee of 52 specialists. The committee is composed of 29 medical professionals and 23 others nominated by professional societies.
Why use established rates for health care reimbursements?
Using established rates for health care reimbursements enables the Medicare insurance program to plan and project for their annual budget. The intent is to inform health care providers what payments they will receive for their Medicare patients.
How much can Medicare increase from current budget?
By Federal statute, the Medicare annual budget request cannot increase more than $20 million from the current budget.
Who needs to be a participant in Medicare?
To receive reimbursement payments at the current rates established by Medicare, health care professionals and service companies need to be participants in the Medicare program.
Does Medicare accept all recommendations?
While Medicare is not obligated to accept all of the recommendations, it has routinely approved more than 90 percent of the recommendations. The process is composed of a number of variables and has been known for lack of transparency by the medical community that must comply with the rates.
What is Medicare for people 65 and older?
Medicare is the federal health insurance program for people who are 65 or older, certain younger people with disabilities, and people with End Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant). Medicare coverage is broken down into different parts.
How much is Medicare Part B 2020?
Most beneficiaries enrolled in Part B in 2020 will have a premium of $144.60/month. Medicare Part B premiums are calculated as a share of Part B program costs.
When is Medicare 2020?
October 16, 2020 at 8:07 AM. If you’re currently on Medicare or reaching the age where you are considering Medicare, it’s important to understand the basics. Furthermore, you should consider how premiums are calculated in order to have an idea of what kind of premium you’ll be looking at. Here is a quick guide showing you what Medicare is, ...
Does Medicare cover hospice?
Medicare Part A is free to most beneficiaries and covers hospital stays, care in a skilled nursing facility, hospice care, and some health care. However, premiums for Part B and Part D depend on a beneficiary’s income. In other words, beneficiaries with higher incomes pay higher premiums.
What is the O-HIP1 PAY through O-HIP6 PAY field?
The O-HIP1 PAY through O-HIP6 PAY fields will display the separate payment amounts for each part of the SCIC. A subtotal amount of all these payments is reported in the SUM field. In other respects this payment report is similar to a typical claim:
What happens if you don't meet the therapy threshold?
That is, the PC Pricer changes the HIPPS code you entered to reflect the HIPPS code that applies for fewer than 10 therapy visits. This change appears on the payment report in the following fields:
Does LUPA claim vary from typical claims?
The entry of LUPA claims does not vary from the entry of typical claims. Enter all the required claim fields, including the HIPPS code of the claim and the numbers of visits.
What is the SGR for Medicare?
Under current law, Medicare’s physician fee-schedule payments are subject to a formula, called the Sustainable Growth Rate (SGR) system, enacted in 1987 as a tool to control spending. For more than a decade this formula has called for cuts in physician payments, reaching as high as 24 percent.
Does Medicare have a fee for service?
Current payment systems in traditional Medicare have evolved over the last several decades, but have maintained a fee-for-service payment structure for most types of providers. In many cases, private insurers have modeled their payment systems on traditional Medicare, including those used for hospitals and physicians.
Does Medicare use prospective payment systems?
Medicare uses prospective payment systems for most of its providers in traditional Medicare. In general, these systems require that Medicare pre-determine a base payment rate for a given unit of service (e.g., a hospital stay, an episode of care, a particular service).
OASIS to HHRG
Home health agencies are paid under the Home Health Prospective Payment System which uses a complex model to calculate episodic payment for up to 60 days of skilled home care services. The rates for each certification period are calculated using the OASIS document, a set of questions used to perform a comprehensive assessment.
Rates and Amounts Set by CMS
At the end of every year the Department of Health and Human Services and the Centers for Medicare and Medicaid Services release the Final Rule outlining changes to the Medicare and Medicaid Programs for the following year. Information includes any policy related changes, new program requirements and rate changes.
Per Visit Rates
The last character of the HIPPS score is the severity level calculation which indicates the Non Routine Supply add on amount. There are 6 severity levels, each with its own amount calculation. This is what CMS expects you will be paying for supplies for the episode based on the patient's condition as described in the OASIS.
What is a DRG in Medicare?
DRG stands for diagnosis-related group. Medicare's DRG system is called the Medicare severity diagnosis-related group, or MS-DRG, which is used to determine hospital payments under the inpatient prospective payment system (IPPS). It's the system used to classify various diagnoses for inpatient hospital stays into groups and subgroups ...
When do hospitals assign DRG?
When you've been admitted as an inpatient to a hospital, that hospital assigns a DRG when you're discharged, basing it on the care you needed during your hospital stay. The hospital gets paid a fixed amount for that DRG, regardless of how much money it actually spends treating you.
What is a DRG relative weight?
DRGs with a relative weight of less than 1.0 are less resource-intensive to treat and are generally less costly to treat. DRG’s with a relative weight of more than 1.0 generally require more resources to treat and are more expensive to treat.
How much did nonprofit hospitals make in 2017?
The largest nonprofit hospitals, however, earned $21 billion in investment income in 2017, 4 and are certainly not struggling financially. The challenge is how to ensure that some hospitals aren't operating in the red under the same payment systems that put other hospitals well into the profitable realm.
Which has higher labor costs, Knoxville or Manhattan?
For example, a hospital in Manhattan, New York City probably has higher labor costs, higher costs to maintain its facility, and higher resource costs than a hospital in Knoxville, Tennessee. The Manhattan hospital probably has a higher base payment rate than the Knoxville hospital.
Does a hospital make money on DRG?
If a hospital can effectively treat you for less money than Medicare pays it for your DRG, then the hospital makes money on that hospitalization. If the hospital spends more money caring for you than Medicare gives it for your DRG, then the hospital loses money on that hospitalization. David Sacks/Stone/Getty Images.
Does Medicare increase hospital base rate?
Each of these things tends to increase a hospital’s base payment rate. Each October, Medicare assigns every hospital a new base payment rate. In this way, Medicare can tweak how much it pays any given hospital, based not just on nationwide trends like inflation, but also on regional trends.
What is MSP payment?
MSP Payment Calculation Examples. The Medicare Secondary Payer (MSP) process may pay secondary benefits when a physician, supplier, or beneficiary submits a claim to the beneficiary's primary insurance and the primary insurance does not pay the entire charge. Medicare will not make a secondary payment if the physician/supplier accepts, ...
What can a provider collect when a provider accepts assignment?
What Can the Provider Collect When a Provider Accepts Assignment? Providers cannot collect more than the "obligated to accept" amount of the primary insurance if the physician/supplier accepts, or is obligated to accept, the primary insurance payment as full payment.
What happens if you don't accept Medicare Part B deductible?
If there is no "obligated to accept" amount from the primary insurance the provider cannot collect more than the higher amount of either the Medicare physician fee schedule or the allowed amount of the primary payer when the beneficiary's Medicare Part B deductible has been met (see examples 1 and 2).
What is an allowed amount?
Allowed Amount (SA): The allowed amount is the amount the primary insurance company allowed for the submitted charges. This may also be referred to on an EOB as eligible charges. This amount should equal the OTAF amount.
Is Medicare a supplemental insurance?
Important: Medicare is not a supplemental insurance, even when secondary, and Medicare's allowable is the deciding factor when determining the patient's liability. The payment information received from the primary insurer will determine the amount Medicare will pay as secondary payer.