- Medicare Part C plans are run by private insurance companies and work similarly to other private health insurance plans
- Plans often cover more benefits than traditional Medicare plans, including vision, dental, hearing, and prescription drug coverage
- Plans put an annual cap on out-of-pocket expenses, unlike standard Medicare
Full Answer
What is Medicare Part C and how is it funded?
Mar 02, 2020 · That means that one out of every three Medicare beneficiaries has a Part C policy. You can purchase Medicare Advantage (MA), or Medicare Part C, plans from a private insurance provider that offers them. Plans differ from company to company but they all must adhere to Medicare rules, and they must be provided by a company that is Medicare-certified.
What are the advantages of Medicare Part C?
Aug 02, 2021 · Medicare Advantage Plans, sometimes called “Part C” or “MA Plans,” are offered by private companies approved by Medicare. If you join a Medicare Advantage Plan, the plan will provide all of your Part A (Hospital Insurance) and Part B (Medical Insurance) coverage. Medicare Advantage Plans may offer extra coverage, such as vision, hearing, dental, and/or health and …
What do you need to know about Medicare Part C?
Medicare Advantage Plan (Part C) A type of Medicare-approved health plan from a private company that you can choose to cover most of your Part A and Part B benefits instead of Original Medicare. It usually also includes drug coverage (Part D). Refer to Medicare glossary for more details. for your health coverage.
How much does Medicare Part C cost per month?
Medicare Advantage Plans, sometimes called "Part C" or "MA Plans," are offered by Medicare-approved private companies that must follow rules set by Medicare. If you join a Medicare Advantage Plan, you'll still have Medicare but you'll get most of your Part A and Part B coverage from your Medicare Advantage Plan, not Original Medicare. These "bundled" plans include …
See more
Medicare Advantage, or Medicare Part C, is a type of Medicare plan that uses private health insurance to cover all the services you’d receive under Medicare Parts A …
What is Medicare Part C and how does it work?
Medicare Advantage, or Medicare Part C, is a type of Medicare plan that uses private health insurance to cover all the services you'd receive under Medicare Parts A and B. Anyone who is eligible for original Medicare Parts A and B is eligible for the Medicare Advantage programs in their area.
What is the patient responsibility for Medicare Part C?
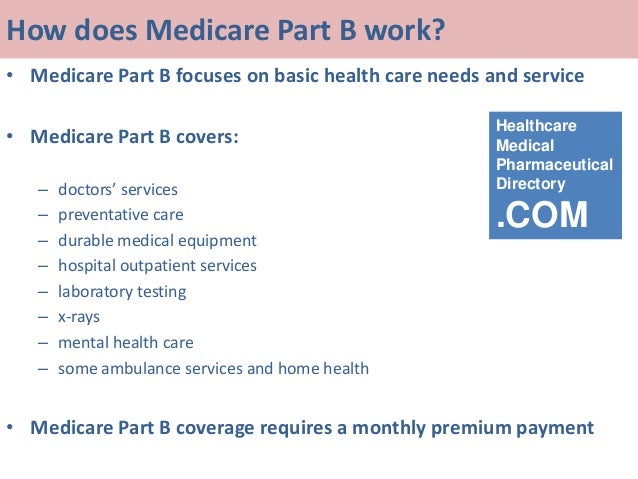
Medicare Part C outpatient coverage doctor's appointments, including specialists. emergency ambulance transportation. durable medical equipment like wheelchairs and home oxygen equipment. emergency room care.
Why do people choose Medicare Part C?
Medicare Part C is a great option for people interested in coverage for prescription drugs, vision and dental services, and more. The cost of a Part C plan depends on a variety of factors, including monthly and yearly costs, copayments, and your medical needs.
Does Medicare Part C cover 20%?
Medicare Part C covers all of the same Part A and B services that you get from Medicare. You will have both hospital and outpatient benefits. However, instead of paying deductibles and 20% of your medical services, you will pay the plan's copays.
Does Medicare Part C cover prescriptions?
Unlike Original Medicare, Medicare Part C generally offers coverage for prescription drugs you take at home. The exact prescription drugs that are covered are listed in the plan's formulary. Formularies may vary from plan to plan.
Is Medicare Part C deducted from Social Security?
Beneficiaries may elect deduction of Medicare Part C (Medicare Advantage) from their Social Security benefit. Some Medicare Advantage plans include a reduction in the Part B premium. Social Security takes that reduction into account, as soon as we are notified of the reduction by CMS.Aug 10, 2011
What is the difference between Medicare Part C and Part D?
Medicare part C is called "Medicare Advantage" and gives you additional coverage. Part D gives you prescription drug coverage.
Is Medicare Part C the same as supplemental insurance?
These are also called Part C plans. Medicare Supplement insurance policies, also called Medigap, help pay the out-of-pocket expenses not covered by Original Medicare (Part A and B). It is not part of the government's Medicare program, but provides coverage in addition to it.Oct 1, 2021
Is Medicare C the same as Medicare Advantage?
A Medicare Advantage is another way to get your Medicare Part A and Part B coverage. Medicare Advantage Plans, sometimes called "Part C" or "MA Plans," are offered by Medicare-approved private companies that must follow rules set by Medicare.
What are the best Medicare Part C plans?
Medicare Part C plansProviderRatingHighlightsKaiser Permanente5.0Top-rated plans Limited availabilityAARP/ UnitedHealthcare4.2Large network of providers Includes great add-onsCigna4.2Strong customer satisfaction Limited network of providersHumana4.0Widely available High rate of complaints2 more rows•Jan 24, 2022
What is Medicare Part A deductible for 2021?
Medicare Part A Premiums/Deductibles The Medicare Part A inpatient hospital deductible that beneficiaries will pay when admitted to the hospital will be $1,484 in 2021, an increase of $76 from $1,408 in 2020.Nov 6, 2020
What are the negatives of a Medicare Advantage plan?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan; if you decide to switch to Medigap, there often are lifetime penalties.
How does Original Medicare work?
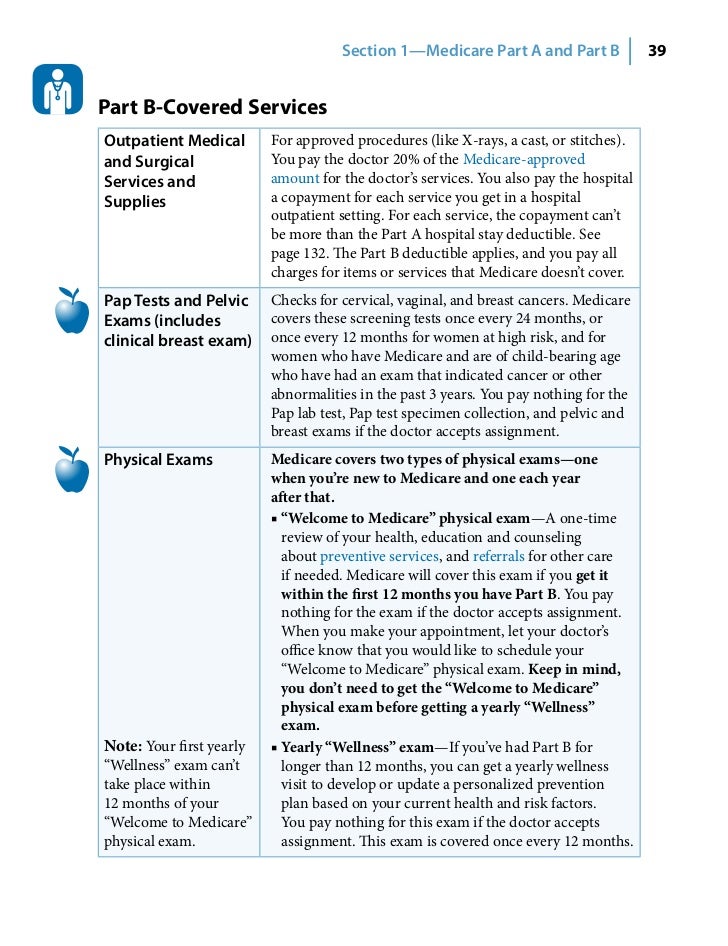
Original Medicare covers most, but not all of the costs for approved health care services and supplies. After you meet your deductible, you pay your share of costs for services and supplies as you get them.
How does Medicare Advantage work?
Medicare Advantage bundles your Part A, Part B, and usually Part D coverage into one plan. Plans may offer some extra benefits that Original Medicare doesn’t cover — like vision, hearing, and dental services.
What is Medicare Advantage Plan?
Medicare Advantage Plans, sometimes called "Part C" or "MA Plans," are an “all in one” alternative to Original Medicare. They are offered by private companies approved by Medicare. If you join a Medicare Advantage Plan, you still have. Medicare.
Can't offer drug coverage?
Can’t offer drug coverage (like Medicare Medical Savings Account plans) Choose not to offer drug coverage (like some Private Fee-for-Service plans) You’ll be disenrolled from your Medicare Advantage Plan and returned to Original Medicare if both of these apply: You’re in a Medicare Advantage HMO or PPO.
What happens if you don't get a referral?
If you don't get a referral first, the plan may not pay for the services. to see a specialist. If you have to go to doctors, facilities, or suppliers that belong to the plan for non-emergency or non-urgent care. These rules can change each year.
Does Medicare cover dental?
Covered services in Medicare Advantage Plans. Most Medicare Advantage Plans offer coverage for things Original Medicare doesn’t cover, like some vision, hearing, dental, and fitness programs (like gym memberships or discounts). Plans can also choose to cover even more benefits. For example, some plans may offer coverage for services like ...
What is Medicare Advantage?
Medicare Advantage, or Medicare Part C, is a type of Medicare plan that uses private health insurance to cover all the services you’d receive under Medicare Parts A and B. Anyone who is eligible for original Medicare Parts A and B is eligible for the Medicare Advantage programs in their area.
What benefits can I expect on Medicare Advantage?
Medicare Advantage covers everything that original Medicare covers. However, Advantage plans also cover hearing, vision, and dental care — which aren’t covered under original Medicare. Depending on the plan, Medicare Advantage may also cover things like gym memberships, transportation, and adult day-care.
How do I enroll in a Medicare Advantage Plan?
Even if you’re happy with your current health care coverage, you should review your plan during open enrollment to see if you’re overpaying or if your benefits will be changing in the coming year.
Get started now
Interested in learning more about Medicare Advantage plans? WebMD Connect to Care Advisors may be able to help.
How to enroll in Medicare Advantage?
To enroll in a Medicare Advantage plan, you must: 1 Be entitled to Part A and enrolled in Part B. 2 Maintain a permanent residence for at least 6 months out of the year in your chosen plan's service area. 3 After you enroll, continue to pay your Part B premium as well as any Medicare Advantage plan premium.
How to contact Kaiser Permanente about Medicare?
If you are becoming eligible for Medicare and your employer offers a group retiree Medicare Advantage health plan through Kaiser Permanente Washington, call us at 1-800-581-8252 or TTY 711 from 8 a.m. to 5 p.m., Monday through Friday.
What is a PPO plan?
PPO. A PPO (preferred provider organization) plan has a network of providers , but members can also use out-of-network providers for covered services. Typically in-network services cost the member less out of pocket than out-of-network services. Providers must accept Medicare to ensure care is covered. SNP.
How long do you have to be in a Medicare Advantage plan?
To enroll in a Medicare Advantage plan, you must: Be entitled to Part A and enrolled in Part B. Maintain a permanent residence for at least 6 months out of the year in your chosen plan's service area. After you enroll, continue to pay your Part B premium as well as any Medicare Advantage plan premium.
What is an HMO?
HMO#N#HMO (health maintenance organization ) plan members generally see doctors, specialists, or hospitals that are part of the plan's network, except for an emergency, out-of-area urgent care, or out-of-area dialysis.
Is MSA covered by Medicare?
Prescription drugs are not covered in an MSA plan, although enrollment in a prescription drug plan is permitted. A PFFS (private fee-for-service) plan is a type of Medicare Advantage plan in which a beneficiary is not limited to a specific network of providers.
Does Medicare Part C cover hospice?
Medicare Advantage plans usually feature: Medicare Part C must cover all of the services that Parts A and B cover except hospice care (still provided by Original Medicare).
How many parts does Medicare have?
Unlike traditional health insurance plans, Medicare is divided into four parts that each cover different services. If you’re already claiming Social Security benefits, then you will be automatically enrolled in Medicare Part A and Medicare Part B once you turn 65. These two parts are known as Original Medicare .
What is the maximum out of pocket amount for Medicare Part C?
If you have Medicare Part C, for services that Medicare Parts A and B cover, the maximum out-of pocket limit is $7,550 per year in 2021 if you go to in-network care providers. The limit is $11,300 per year for combined in-network and out-of-network costs.
What are the benefits of a Medicare plan?
Plans often cover more benefits than traditional Medicare plans, including vision, dental, hearing, and prescription drug coverage. Plans put an annual cap on out-of-pocket expenses, unlike standard Medicare. Plans restrict you to a much smaller, local network of available doctors and health care providers.
How much is Medicare Part B in 2021?
The Medicare Part B premium is typically $148.50 a month in 2021, but it may be higher if you earn a higher income. Beyond that, prices can vary greatly by plan. Medicare Advantage premiums average $33 in 2020, according to data from the CMS compiled by Policygenius. At the same time, premiums can reach up to $481.
What is Medicare for older people?
Medicare is a federal health insurance program that primarily serves Americans age 65 and older. It’s also available to younger individuals with certain disabilities or health conditions. Medicare consists of multiple parts, which each cover different types of health services.
What is a copay?
A copay is a flat fee that you pay whenever you receive certain services. For example, a hospital stay for a surgery could come with a copay of $100 per day. If you stay three days, you will end up paying $300 in copays plus other costs the visit incurs.
What is MSA in Medicare?
MSAs are a bit different from the types of plans above. An MSA works very similarly to a high-deductible health plan (HDHP) paired with a health savings account (HSA). With an MSA plan, Medicare will deposit money into an account that you can then use to pay for your health care services. Your insurance will not start to pay for your medical expenses until you spend enough to hit your deductible.
What is Medicare Supplement?
Medicare supplement insurance policies help fill in the gaps left by Original Medicare health care insurance. For many people, Medicare Supplement, also known as Medigap, insurance helps them economically by paying some of the out-of-pocket costs associated with Original Medicare.
What percentage of Medicare supplement is paid?
After this is paid, your supplement policy pays your portion of the remaining cost. This is generally 20 percent. Some policies pay your deductibles The deductible is a set amount which you must pay before Medicare begins covering your health care costs.
How many people does Medicare Supplement cover?
Keep in mind that, just like Medicare, Medicare Supplement plans are individual insurance policies. They only cover one person per plan. If you want coverage for your spouse, you must purchase a separate plan.
How long does it take to get a Medigap plan?
When you turn 65 and enroll in Part B, you will have a 6-month Initial Enrollment Period to purchase any Medigap plan sold in your state. During this time, you have a “guaranteed issue right” to buy any plan available. They are required to accept you and cannot charge you more due to any pre-existing conditions.
How long does Medicare cover travel?
Each plan varies in what it covers, but all plans pay for Medicare Part A (hospital insurance) coinsurances for up to 365 days beyond the coverage that Medicare offers. Some of the plans cover a percentage of the cost for emergency health care while traveling abroad.
How old do you have to be to qualify for medicare?
To be eligible for Medicare, you must be at least 65 years old, a citizen of the United States or permanent legal resident for at least five consecutive years. Also, you, or your spouse, must have worked and paid federal taxes for at least ten years (or 40 quarters).
Does Medicare cover long term care?
Most plans do not cover long-term care, vision, dental, hearing care, or private nursing care. All Medicare Supplement insurance coverage comes with a monthly premium which you pay directly to your provider. How much you pay depends on which plan you have.
What happens if you get a health care provider out of network?
If you get health care outside the plan’s network, you may have to pay the full cost. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed. In most cases, you need to choose a primary care doctor. Certain services, like yearly screening mammograms, don’t require a referral. If your doctor or other health care provider leaves the plan’s network, your plan will notify you. You may choose another doctor in the plan’s network. HMO Point-of-Service (HMOPOS) plans are HMO plans that may allow you to get some services out-of-network for a higher copayment or coinsurance. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed.
What is an HMO plan?
Health Maintenance Organization (HMO) plan is a type of Medicare Advantage Plan that generally provides health care coverage from doctors, other health care providers, or hospitals in the plan’s network (except emergency care, out-of-area urgent care, or out-of-area dialysis). A network is a group of doctors, hospitals, and medical facilities that contract with a plan to provide services. Most HMOs also require you to get a referral from your primary care doctor for specialist care, so that your care is coordinated.
What is a special needs plan?
Special Needs Plan (SNP) provides benefits and services to people with specific diseases, certain health care needs, or limited incomes. SNPs tailor their benefits, provider choices, and list of covered drugs (formularies) to best meet the specific needs of the groups they serve.
Do providers have to follow the terms and conditions of a health insurance plan?
The provider must follow the plan’s terms and conditions for payment, and bill the plan for the services they provide for you. However, the provider can decide at every visit whether to accept the plan and agree to treat you.
Can a provider bill you for PFFS?
The provider shouldn’t provide services to you except in emergencies, and you’ll need to find another provider that will accept the PFFS plan .However, if the provider chooses to treat you, then they can only bill you for plan-allowed cost sharing. They must bill the plan for your covered services. You’re only required to pay the copayment or coinsurance the plan allows for the types of services you get at the time of the service. You may have to pay an additional amount (up to 15% more) if the plan allows providers to “balance bill” (when a provider bills you for the difference between the provider’s charge and the allowed amount).