How Medicaid works with Medicare
- Medicaid can provide secondary insurance: For services covered by Medicare and Medicaid (such as doctors’ visits,...
- Medicaid can provide premium assistance: In many cases, if you have Medicare and Medicaid, you will automatically be...
- Medicaid can provide cost-sharing assistance: Depending on your income, you may qualify for the...
What services are covered by Medicaid?
- What financial aid options are available for parents in 2022?
- What is the medicare deductible for 2022?
- No, you shouldn't laminate your Social Security card
Who really pays for Medicaid?
Who Really Pays For Health Care Might Surprise You
- Before Obamacare we had a free-market health-care system. Government has been part of the business of medicine at least since the 1940s, when Washington began appropriating billions to build private ...
- I fully paid for Medicare through taxes deducted from my salary. ...
- Premiums from my paycheck fund my company health plan. Probably not entirely. ...
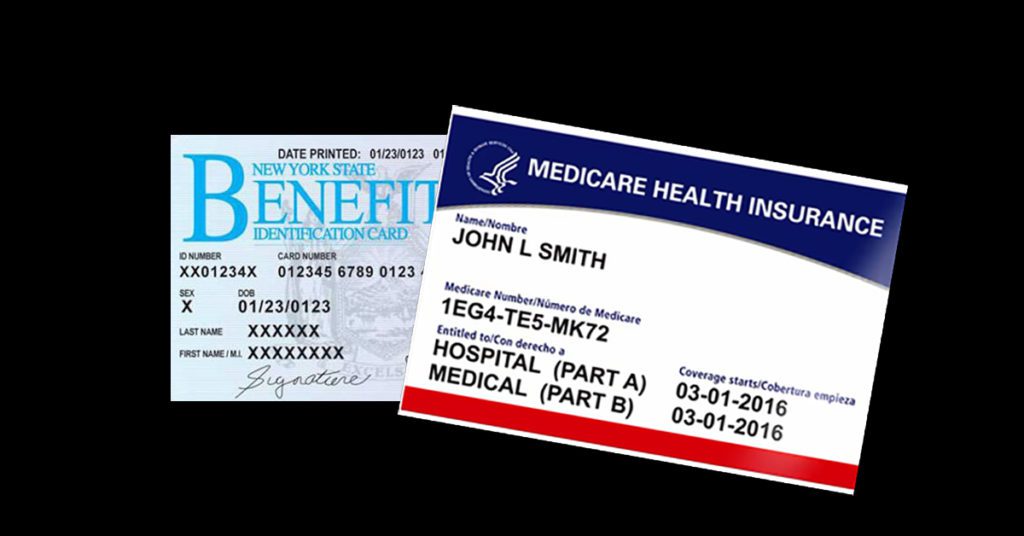
Do you know the difference between Medicaid and Medicare?
Medicare is the primary medical coverage provider for seniors and those with a disability. Medicaid is designed for people with limited income. Medicare has four parts that each cover different things—hospitalization, medically necessary services, supplemental coverage, and prescription drugs.
How to combine Medicare and Medicaid to save money?
You should have the following information ready when you apply:
- Full legal name, Date of Birth, Social Security Number, Citizenship or Immigration Status for you and anyone in your household who is applying for health care coverage.
- Most recent federal tax filing information (if available).
- Job and income information for members of your household for the month prior or the current month. ...

Do Medicaid and Medicare cover the same things?
Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid. pays second. Medicaid never pays first for services covered by Medicare. It only pays after Medicare, employer group health plans, and/or Medicare Supplement (Medigap) Insurance have paid.
When a patient is covered through Medicare and Medicaid which coverage is primary?
gov . Medicare pays first, and Medicaid pays second . If the employer has 20 or more employees, then the group health plan pays first, and Medicare pays second .
What is the highest income to qualify for Medicaid?
Federal Poverty Level thresholds to qualify for Medicaid The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.
What are the disadvantages of Medicaid?
Disadvantages of Medicaid They will have a decreased financial ability to opt for elective treatments, and they may not be able to pay for top brand drugs or other medical aids. Another financial concern is that medical practices cannot charge a fee when Medicaid patients miss appointments.
What’s the Difference Between Medicaid and Medicare?
Medicaid is an assistance program. For anyone that qualifies, Medicaid enrollment is open the entire year. Most Medicaid enrollees lack access to a...
Can You Have Medicare and Medicaid?
The short answer is yes. If you receive coverage from both Medicaid and Medicare, you’re a “dually eligible beneficiary.” If you are dual eligible,...
What is Covered?
Your state determines Medicaid services. Original Medicare coverage includes Part A (hospital) and Part B (medical). It is important to know that y...
What are my Costs with dual eligibility?
Dual eligibility can limit individual costs for beneficiaries. For those with Medicare, state Medicaid programs will pay for many cost-sharing and...
Can I change plans if I’m dual eligible?
Yes. If you have Medicare and full Medicaid coverage, you can change plans once per calendar quarter for the first three quarters. The new plan wil...
Where do I apply for Medicaid?
You can apply through your state health department’s website, over the phone or even by mail.
What is the history of Medicaid, and how is it tied to Medicare?
Medicaid and Medicare share a birthday, both born on July 30, 1965, when President Lyndon B. Johnson signed legislation creating a pair of programs...
What is the difference between Medicare and Medicaid?
When you have dual enrollment, Medicare is your primary insurance that covers any costs first. Medicaid is your secondary payer. Every state has different benefits for people who qualify under dual eligibility, so it’s important that you check with your local Medicaid office.
Does Medicaid cover dental care?
Medicaid can cover a large variety of healthcare services like behavioral health for substance abuse and mental health or dental care. Medicaid also has a robust cost-sharing program that helps cover any out of pocket costs for economically disadvantaged participants.
Can seniors get medicaid?
Many seniors in the United States have dual eligibility for Medicare and Medicaid benefits. Generally, this means that you have enrolled in Medicare, but that you qualify for Medicaid as well due to your income.
Is Medicaid a secondary insurance?
Secondary Insurance. Medicaid can fill in the gap as a secondary insurance to Medicare. Any services you have that Medicare pays for like hospital care, doctor’s visits, skilled nursing facility care, or home care, Medicare will pay for as the primary payer.
Does Medicaid pay cost sharing?
Medicaid can pay any cost-sharing charges you have. This help will depend on your income level. If the level is low enough, you could qualify for the Qualified Medicare Beneficiary (QMB) Medicare Savings Program. If you enroll in QMB, you won’t have to pay Medicare cost-sharing fees.
Does Medicare help with prescription drugs?
Prescription drugs are some of the biggest expenses people on Medicare face, and Medicaid can help. People who meet the eligibility requirements for dual enrollment in Medicare and Medicaid automatically get enrolled in the Extra Help program.
How does Original Medicare work?
Original Medicare covers most, but not all of the costs for approved health care services and supplies. After you meet your deductible, you pay your share of costs for services and supplies as you get them.
How does Medicare Advantage work?
Medicare Advantage bundles your Part A, Part B, and usually Part D coverage into one plan. Plans may offer some extra benefits that Original Medicare doesn’t cover — like vision, hearing, and dental services.
What is Medicare and Medicaid?
Differentiating Medicare and Medicaid. Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. Since it can be easy to confuse the two terms, Medicare and Medicaid, it is important to differentiate between them. While Medicare is a federal health insurance program ...
How to apply for medicaid?
How to Apply. To apply for Medicare, contact your local Social Security Administration (SSA) office. To apply for Medicaid, contact your state’s Medicaid agency. Learn about the long-term care Medicaid application process. Prior to applying, one may wish to take a non-binding Medicaid eligibility test.
How much does Medicare Part B cost?
For Medicare Part B (medical insurance), enrollees pay a monthly premium of $148.50 in addition to an annual deductible of $203. In order to enroll in a Medicare Advantage (MA) plan, one must be enrolled in Medicare Parts A and B. The monthly premium varies by plan, but is approximately $33 / month.
What is the income limit for Medicaid in 2021?
In most cases, as of 2021, the individual income limit for institutional Medicaid (nursing home Medicaid) and Home and Community Based Services (HCBS) via a Medicaid Waiver is $2,382 / month. The asset limit is generally $2,000 for a single applicant.
How old do you have to be to qualify for medicare?
Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare. Applicants must also be at least 65 years old. For persons who are disabled or have been diagnosed with end-stage renal disease or Lou Gehrig’s disease (amyotrophic lateral sclerosis), there is no age requirement. Eligibility for Medicare is not income based. Therefore, there are no income and asset limits.
Does Medicare cover out-of-pocket expenses?
Persons who are enrolled in both Medicaid and Medicare may receive greater healthcare coverage and have lower out-of-pocket costs. For Medicare covered expenses, such as medical and hospitalization, Medicare is always the first payer (primary payer). If Medicare does not cover the full cost, Medicaid (the secondary payer) will cover the remaining cost, given they are Medicaid covered expenses. Medicaid does cover some expenses that Medicare does not, such as personal care assistance in the home and community and long-term skilled nursing home care (Medicare limits nursing home care to 100 days). The one exception, as mentioned above, is that some Medicare Advantage plans cover the cost of some long term care services and supports. Medicaid, via Medicare Savings Programs, also helps to cover the costs of Medicare premiums, deductibles, and co-payments.
Does Medicaid cover nursing home care?
Medicaid also pays for nursing home care, and often limited personal care assistance in one’s home. While some states offer long-term care and supports in the home and community thorough their state Medicaid program, many states offer these supports via 1915 (c) Medicaid waivers.
How does Medicare and Medicaid work together?
Medicare and Medicaid work together to cover costs, including long-term services. If you do not have full Medicaid benefits, Medicare Savings Programs (MSP) may help cover some of those costs: Qualified Medicare Beneficiary (QMB) Program. Specified Low-Income Medicare Beneficiary (SLMB) program.
What are the benefits of Medicare Part A?
Dual-eligible beneficiaries can have: 1 Medicare Part A#N#Medicare Part A, also called "hospital insurance," covers the care you receive while admitted to the hospital, skilled nursing facility, or other inpatient services. Medicare Part A is part of Original Medicare. 2 Medicare Part B#N#Medicare Part B is the portion of Medicare that covers your medical expenses. Sometimes called "medical insurance," Part B helps pay for the Medicare-approved services you receive. 3 Both Part A and Part B 4 Full Medicaid benefits 5 State Medicare Savings Programs
What is partial coverage?
Partial coverage may include Medicaid coverage for expenses like Medicare premiums. A premium is a fee you pay to your insurance company for health plan coverage. This is usually a monthly cost. A deductible is an amount you pay out of pocket before your insurance company covers its portion of your medical bills.
How long does it take to get medicaid after a disability?
An individual under 65 receiving Social Security Disability Insurance can have Medicaid and later enroll in Medicare after 24 months of receiving Social Security Disability benefits, or upon reaching the age of 65.
What is dual eligibility for medicaid?
Medicaid is a state-based health insurance program for individuals that qualify. Unlike Medicare, Medicaid does not have age restrictions for members. , you are dual-eligible. Dual-eligibility allows beneficiaries to combine Medicare and Medicaid benefits to expand coverage ...
What is full coverage Medicare?
. Full coverage consists of the same benefits as partial coverage and may include services not covered by Medicare like long-term care.
What is Medicare Part A?
Dual-eligible beneficiaries can have: Medicare Part A. Medicare Part A, also called "hospital insurance, " covers the care you receive while admitted to the hospital, skilled nursing facility, or other inpatient services. Medicare Part A is part of Original Medicare. Medicare Part B.
What is integrated care?
When care is provided to Medicare-Medicaid beneficiaries through an “integrated” care model, the beneficiary can get the full array of Medicaid and Medicare benefits through a single delivery system. This approach can improve care coordination and quality, and reduce administrative burdens. One such model is the Program for All-Inclusive Care ...
Can Medicare beneficiaries get help with out of pocket medical expenses?
Medicare beneficiaries who have limited income and resources may get help paying for their Medicare premiums and out-of-pocket medical expenses from Medicaid.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
Eligibility
In addition to low-income Americans, other eligible groups include people with serious illness and unmet health care needs; this includes women with breast cancer or cervical cancer, as well as adults who need treatment for tuberculosis.
Enrollment and Expansion
As part of health care reform, Medicaid application and enrollment became consolidated through the Health Insurance Marketplace.
Costs: Who pays what?
Medicaid’s funding has long been a hot-button political issue. In this 1995 photo, an elderly woman protests cuts to Medicare and Medicaid at a health care march and rally in New York City.
Lots More Information
One fact I learned while discovering the ins and outs of our public health care system is this: Every year, 45,000 Americans die because they couldn't afford the care they needed to get well -- and to put that number into perspective, that's as many as 5 people dying every hour from something that could have been prevented or treated.
