Part A is primarily hospital coverage. It will pay for expenses related to inpatient hospital care, hospice
Hospice
Hospice care is a type of care and philosophy of care that focuses on the palliation of a chronically ill, terminally ill or seriously ill patient's pain and symptoms, and attending to their emotional and spiritual needs. In Western society, the concept of hospice has been evolving in Europe since the 11…
Full Answer
What is the difference between Medicare Part an and Part B?
Summary:
- Both Medicare Part A and B are federally funded plans that come with different coverages.
- Part A is free, and the patients need not pay a premium for the coverage. People have to pay some premium for availing themselves of the Part B coverage.
- Part A can be called hospital insurance whereas Part B can be termed as medical insurance.
How do I know if I have Medicare Part?
- You are 65 or older and meet the citizenship or residency requirements.
- You are under age 65, disabled, and your premium-free Medicare Part A coverage ended because you returned to work.
- You have not paid Medicare taxes through your employment or have not worked the required time to qualify for premium-free Part A.
Does Medicare Part A have a premium?
They differ not only in the Medicare benefits covered but also in how the premiums are determined. Most people eligible for Part A have premium-free coverage. The premium is based on credits earned by working and paying taxes. When you work in the U.S., a portion of the taxes automatically deducted are earmarked for the Medicare program.
What is the premium for Medicare Part A?
People who buy Part A will pay a premium of either $259 or $471 each month in 2021 depending on how long they or their spouse worked and paid Medicare taxes. If you choose NOT to buy Part A, you can still buy Part B.

Does Medicare Part A cover 100 percent?
Most medically necessary inpatient care is covered by Medicare Part A. If you have a covered hospital stay, hospice stay, or short-term stay in a skilled nursing facility, Medicare Part A pays 100% of allowable charges for the first 60 days after you meet your Part A deductible.
What is the main benefit of Medicare Part A?
Medicare Part A hospital insurance covers inpatient hospital care, skilled nursing facility, hospice, lab tests, surgery, home health care.
What is Medicare Part A and how does it work?
Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. coverage if you or your spouse paid Medicare taxes for a certain amount of time while working. This is sometimes called "premium-free Part A." Most people get premium-free Part A.
Do patients pay for Medicare Part A?
Most people don't pay a monthly premium for Part A (sometimes called "premium-free Part A"). If you buy Part A, you'll pay up to $499 each month in 2022. If you paid Medicare taxes for less than 30 quarters, the standard Part A premium is $499.
Is Medicare Part A free at age 65?
You are eligible for premium-free Part A if you are age 65 or older and you or your spouse worked and paid Medicare taxes for at least 10 years. You can get Part A at age 65 without having to pay premiums if: You are receiving retirement benefits from Social Security or the Railroad Retirement Board.
What is not covered by Medicare Part A?
Medicare Part A will not cover long-term care, non-skilled, daily living, or custodial activities. Certain hospitals and critical access hospitals have agreements with the Department of Health & Human Services that lets the hospital “swing” its beds into (and out of) SNF care as needed.
Does Medicare Part A cover emergency room visits?
Medicare Part A is sometimes called “hospital insurance,” but it only covers the costs of an emergency room (ER) visit if you're admitted to the hospital to treat the illness or injury that brought you to the ER.
Do I have to pay for Medicare Part B?
Part B premiums You pay a premium each month for Part B. Your Part B premium will be automatically deducted from your benefit payment if you get benefits from one of these: Social Security. Railroad Retirement Board.
Why do I need Medicare Part C?
Medicare Part C provides more coverage for everyday healthcare including prescription drug coverage with some plans when combined with Part D. A Medicare Advantage prescription drug (MAPD) plan is when a Part C and Part D plan are combined. Medicare Part D only covers prescription drugs.
How much is deducted from Social Security for Medicare?
In 2021, based on the average social security benefit of $1,514, a beneficiary paid around 9.8 percent of their income for the Part B premium. Next year, that figure will increase to 10.6 percent.
How much is the Part A deductible?
Part A Deductible: The deductible is an amount paid before Medicare begins to pay its share. The Part A deductible for an inpatient hospital stay is $1,556 in 2022. The Part A deductible is not an annual deductible; it applies for each benefit period.
Is Medicare taken out of your Social Security check?
Yes. In fact, if you are signed up for both Social Security and Medicare Part B — the portion of Medicare that provides standard health insurance — the Social Security Administration will automatically deduct the premium from your monthly benefit.
How does Original Medicare work?
Original Medicare covers most, but not all of the costs for approved health care services and supplies. After you meet your deductible, you pay your share of costs for services and supplies as you get them. There’s no limit on what you’ll pay out-of-pocket in a year unless you have other coverage (like Medigap, Medicaid, or employee or union coverage). Get details on cost saving programs.
What is Medicare Advantage?
Medicare Advantage bundles your Part A, Part B, and usually Part D coverage into one plan. Plans may offer some extra benefits that Original Medicare doesn’t cover — like vision, hearing, and dental services.
Why buy Medicare Supplement Insurance?
Buy a Medicare Supplement Insurance (Medigap) policy to help lower your share of costs for services you get.
Is Medicare a private insurance?
Medicare is different from private insurance — it doesn’t offer plans for couples or families. You don’t have to make the same choice as your spouse.
Does Medicare cover urgent care?
Plans must cover all emergency and urgent care, and almost all medically necessary services Original Medicare covers. Some plans tailor their benefit packages to offer additional benefits to treat specific conditions.
How to know if Medicare will cover you?
Talk to your doctor or other health care provider about why you need certain services or supplies. Ask if Medicare will cover them. You may need something that's usually covered but your provider thinks that Medicare won't cover it in your situation. If so, you'll have to read and sign a notice. The notice says that you may have to pay for the item, service, or supply.
What is national coverage?
National coverage decisions made by Medicare about whether something is covered. Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
Is Medicare Advantage the same as Original Medicare?
What's covered? Note. If you're in a Medicare Advantage Plan or other Medicare plan, your plan may have different rules. But, your plan must give you at least the same coverage as Original Medicare. Some services may only be covered in certain settings or for patients with certain conditions.
How to learn more about Medicare?
You can learn more about the Original Medicare Plan and the Medicare program by reading “Medicare & You”, the official government handbook about Medicare. You will need the free Adobe® Reader® software to download the files.
When does the enrollment period start for a new Medicare plan?
General Enrollment Period —Between January 1 – March 31 each year. Your coverage will begin July 1. You may have to pay a higher premium for late enrollment. See below.
What is inpatient care?
Inpatient care in a skilled nursing facility (not custodial or long-term care) Hospice care services. Home health care services. Inpatient care in a religious non-medical health care institution (RNHCI). You usually don’t pay a monthly premium for Part A coverage if you or your spouse paid Medicare taxes while working.
How long does Medicare enrollment last?
Initial Enrollment Period —When you are first eligible for Medicare. (This is a 7-month period that begins three months before the month you turn age 65, includes the month you turn age 65, and ends three months after the month you turn age 65.)
What to call if you are disabled and your Part A coverage ends?
You are disabled and your premium-free Part A coverage ended because you returned to work. Call Social Security at 1-800-772-1213 for more information about the Part A premium. TTY users should call 1-800-325-0778. In most cases, if you choose to buy Part A, you must also have Part B and pay monthly premiums for both.
How long do you have to pay higher insurance premiums?
You will have to pay the higher premium for twice the number of years you could have had Part A, but didn’t join. For example, if you were eligible for Part A, but didn’t join for two years, you will have to pay the higher premium for four years.
When do you get Medicare if you are 65?
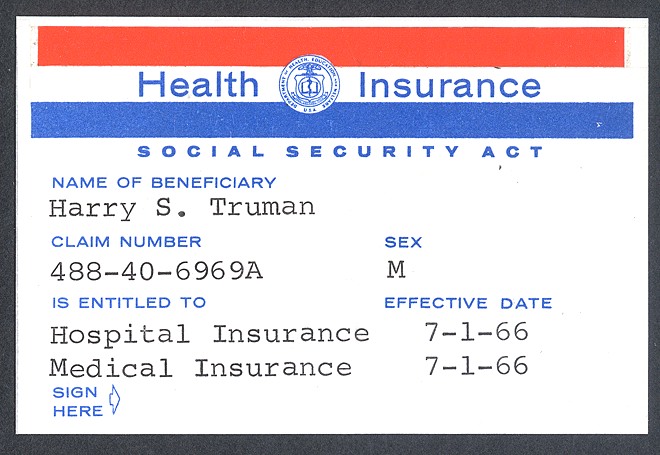
You will get your Medicare card in the mail three months before your 65th birthday or your 25th month of disability.
What is Medicare premium?
premium. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage. for. Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
What does Part B cover?
In most cases, if you choose to buy Part A, you must also: Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. Contact Social Security for more information about the Part A premium. Learn how and when you can sign up for Part A. Find out what Part A covers.
How much will Medicare premiums be in 2021?
People who buy Part A will pay a premium of either $259 or $471 each month in 2021 depending on how long they or their spouse worked and paid Medicare taxes. If you choose NOT to buy Part A, you can still buy Part B. In most cases, if you choose to buy Part A, you must also: Have. Medicare Part B (Medical Insurance)
What is premium free Part A?
Most people get premium-free Part A. You can get premium-free Part A at 65 if: The health care items or services covered under a health insurance plan. Covered benefits and excluded services are defined in the health insurance plan's coverage documents.
What is covered benefits and excluded services?
Covered benefits and excluded services are defined in the health insurance plan's coverage documents. from Social Security or the Railroad Retirement Board. You're eligible to get Social Security or Railroad benefits but haven't filed for them yet. You or your spouse had Medicare-covered government employment.
What Is Medicare Part A?
Part A is the hospital insurance portion of Medicare. Most people become eligible for Medicare once they turn 65, and they may be automatically enrolled if they receive Social Security benefits. Otherwise, you have a limited window of time during which to sign up for Part A without having to pay a penalty. This is referred to as the initial enrollment period. It lasts for a total of seven months (three months before you become eligible for Medicare and three months after).
What is Part A in nursing?
Part A covers a percentage of hospital or skilled nursing facilities based on benefit periods. A benefit period begins when you're admitted and ends 60 days after you are no longer receiving care. There is no limit on benefit periods. Part A also covers 100% of hospice care and skilled intermittent home health care.
How long does Medicare enrollment last?
This is referred to as the initial enrollment period, which lasts for a total of seven months (three months before you become eligible for Medicare and three months after). 2. If you already get Social Security retirement benefits (or are eligible for them), you won’t pay a premium for part A.
How many people are covered by Medicare?
Introduced in 1965, Medicare covered 61 million people in 2019, almost 19% of the population. 1. The original Medicare program had two parts: hospital insurance (Part A) and medical insurance (Part B). But it has expanded over the years to include optional drug coverage (Part D). Medicare can also refer to comprehensive plans offered by private ...
What is respite care in Medicare?
Aide and homemaker services. Inpatient respite care received in a Medicare-certified facility to provide rest to the usual caregiver, such as a family member. Services can be provided in the home, or at a Medicare-certified facility.
When it pays, does it depend on the plan you enroll in?
When it pays: It depends on the specific plan you enroll in, but benefits eligibility will be similar to other Medicare plans.
Do you have to pay for Medicare Advantage?
What you pay: If you select Medicare Advantage, you have to enroll and pay for the Part B premium. However, some Medicare Advantage plans will pay the Part B premium for you, and others will charge an additional premium. Each Medicare advantage plan has its own deductibles and copays.
When do you get Part A?
An individual who is receiving monthly Social Security or RRB benefits at least 4 months prior to turning age 65 does not need to file a separate application to become entitled to premium-free Part A. In this case, the individual will get Part A automatically at age 65.
How long does Medicare take to pay for disability?
A person who is entitled to monthly Social Security or Railroad Retirement Board (RRB) benefits on the basis of disability is automatically entitled to Part A after receiving disability benefits for 24 months.
How to qualify for Medicare premium free?
To be eligible for premium-free Part A, an individual must be entitled to receive Medicare based on their own earnings or those of a spouse, parent, or child. To receive premium-free Part A, the worker must have a specified number of quarters of coverage (QCs) and file an application for Social Security or Railroad Retirement Board (RRB) benefits. The exact number of QCs required is dependent on whether the person is filing for Part A on the basis of age, disability, or End Stage Renal Disease (ESRD). QCs are earned through payment of payroll taxes under the Federal Insurance Contributions Act (FICA) during the person's working years. Most individuals pay the full FICA tax so the QCs they earn can be used to meet the requirements for both monthly Social Security benefits and premium-free Part A.
How long do you have to be on Medicare if you are disabled?
Disabled individuals are automatically enrolled in Medicare Part A and Part B after they have received disability benefits from Social Security for 24 months. NOTE: In most cases, if someone does not enroll in Part B or premium Part A when first eligible, they will have to pay a late enrollment penalty.
How long does it take to get Medicare if you are 65?
For someone under age 65 who becomes entitled to Medicare based on disability, entitlement begins with the 25 th month of disability benefit entitlement.
What is the income related monthly adjustment amount for Medicare?
Individuals with income greater than $85,000 and married couples with income greater than $170,000 must pay a higher premium for Part B and an extra amount for Part D coverage in addition to their Part D plan premium. This additional amount is called income-related monthly adjustment amount. Less than 5 percent of people with Medicare are affected, so most people will not pay a higher premium.
When do you have to apply for Medicare if you are already on Social Security?
Individuals already receiving Social Security or RRB benefits at least 4 months before being eligible for Medicare and residing in the United States (except residents of Puerto Rico) are automatically enrolled in both premium-free Part A and Part B. People living in Puerto Rico who are eligible for automatic enrollment are only enrolled in premium-free Part A.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
Which pays first, Medicare or group health insurance?
If you have group health plan coverage through an employer who has 20 or more employees, the group health plan pays first, and Medicare pays second.
What is a Medicare company?
The company that acts on behalf of Medicare to collect and manage information on other types of insurance or coverage that a person with Medicare may have, and determine whether the coverage pays before or after Medicare. This company also acts on behalf of Medicare to obtain repayment when Medicare makes a conditional payment, and the other payer is determined to be primary.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
What do I need to know about Medicare?
What else do I need to know about Original Medicare? 1 You generally pay a set amount for your health care (#N#deductible#N#The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay.#N#) before Medicare pays its share. Then, Medicare pays its share, and you pay your share (#N#coinsurance#N#An amount you may be required to pay as your share of the cost for services after you pay any deductibles. Coinsurance is usually a percentage (for example, 20%).#N#/#N#copayment#N#An amount you may be required to pay as your share of the cost for a medical service or supply, like a doctor's visit, hospital outpatient visit, or prescription drug. A copayment is usually a set amount, rather than a percentage. For example, you might pay $10 or $20 for a doctor's visit or prescription drug.#N#) for covered services and supplies. There's no yearly limit for what you pay out-of-pocket. 2 You usually pay a monthly premium for Part B. 3 You generally don't need to file Medicare claims. The law requires providers and suppliers to file your claims for the covered services and supplies you get. Providers include doctors, hospitals, skilled nursing facilities, and home health agencies.
What is Part A (Hospital Insurance)?
Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
Can I get my health care from any doctor, other health care provider, or hospital?
In most cases, yes. You can go to any doctor, health care provider, hospital, or facility that is enrolled in Medicare and accepting new Medicare patients.
What is Medicare Advantage?
Medicare Advantage Plans may also offer prescription drug coverage that follows the same rules as Medicare drug plans. .
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. ) before Medicare pays its share. Then, Medicare pays its share, and you pay your share (. coinsurance.
What factors affect Medicare out of pocket costs?
Whether you have Part A and/or Part B. Most people have both. Whether your doctor, other health care provider, or supplier accepts assignment. The type of health care you need and how often you need it.
Do you have to choose a primary care doctor for Medicare?
No, in Original Medicare you don't need to choose a. primary care doctor. The doctor you see first for most health problems. He or she makes sure you get the care you need to keep you healthy. He or she also may talk with other doctors and health care providers about your care and refer you to them.
