How long does Medicare cover SNF?
After day 100 of an inpatient SNF stay, you are responsible for all costs. Medicare Part A will also cover 90 days of inpatient hospital rehab with some coinsurance costs after you meet your Part A deductible. Beginning on day 91, you will begin to tap into your “lifetime reserve days.".
How long does rehab last in a skilled nursing facility?
When you enter a skilled nursing facility, your stay (including any rehab services) will typically be covered in full for the first 20 days of each benefit period (after you meet your Medicare Part A deductible). Days 21 to 100 of your stay will require a coinsurance ...
How much is Medicare Part A deductible for 2021?
In 2021, the Medicare Part A deductible is $1,484 per benefit period. A benefit period begins the day you are admitted to the hospital. Once you have reached the deductible, Medicare will then cover your stay in full for the first 60 days. You could potentially experience more than one benefit period in a year.
How much is coinsurance for inpatient care in 2021?
If you continue receiving inpatient care after 60 days, you will be responsible for a coinsurance payment of $371 per day (in 2021) until day 90. Beginning on day 91, you will begin to tap into your “lifetime reserve days,” for which a daily coinsurance of $742 is required in 2021. You have a total of 60 lifetime reserve days.
What day do you get your lifetime reserve days?
Beginning on day 91 , you will begin to tap into your “lifetime reserve days.". You may have to undergo some rehab in a hospital after a surgery, injury, stroke or other medical event. The rehab may take place in a designated section of a hospital or in a stand-alone rehabilitation facility. Medicare Part A provides coverage for inpatient care ...
How long do you have to be out of the hospital to get a deductible?
When you have been out of the hospital for 60 days in a row, your benefit period ends and your Part A deductible will reset the next time you are admitted.
Does Medicare cover rehab?
Learn how inpatient and outpatient rehab and therapy can be covered by Medicare. Medicare Part A (inpatient hospital insurance) and Part B (medical insurance) may both cover certain rehabilitation services in different ways.
What are the requirements for Medicare rehab?
In addition to the benefit period rules above, a beneficiary must meet all the following requirements: The beneficiary has Medicare Part A (hospital insurance) and days left in their benefit period available to use. The beneficiary has a qualifying hospital stay.
How much is Medicare coinsurance for 2021?
In 2021, the coinsurance is $185.50 per day. Days 101 and beyond: Medicare provides no rehab coverage after 100 days. Beneficiaries must pay for any additional days completely out of pocket, apply for Medicaid coverage, explore other payment options or risk discharge from the facility.
What is Medicare benefit period?
Medicare measures the use and coverage of skilled nursing care in “ benefit periods.”. This is a complicated concept that often trips up seniors and family caregivers. Each benefit period begins on the day that a Medicare beneficiary is admitted to the hospital on an inpatient basis. Time spent at the hospital on an outpatient or observation basis ...
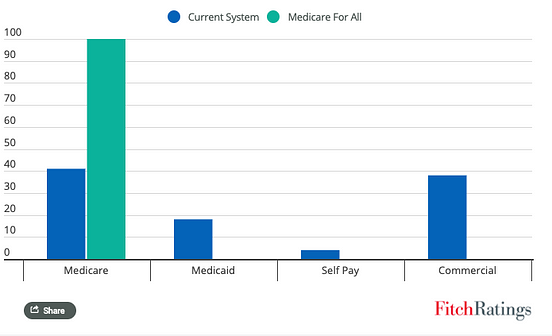
What is Medicaid dually eligible?
Medicaid provides assistance with paying for skilled and/or custodial care, medications, and other medical expenses. If they qualify for both Medicare and Medicaid, then they are considered a “ dually eligible beneficiary ” and most of their health care costs are typically covered.
How long does a SNF benefit last?
A benefit period ends when the beneficiary has not received inpatient hospital or SNF care for 60 consecutive days . Once a benefit period ends, a new one can begin the next time the beneficiary is admitted to the hospital. There is no limit to the number of benefit periods a beneficiary can have.
How long does a beneficiary have to stay in hospital for SNF?
For example, if a beneficiary leaves the SNF for less than 30 days and then needs to return for the same medical condition (or a related one), they will not need another qualifying three-day hospital stay to be eligible for additional SNF coverage left in their benefit period.
How long does it take to get into a skilled nursing facility?
Following a qualifying hospital stay, a beneficiary must enter the skilled nursing facility within a short period of time (generally 30 days) of being discharged. The beneficiary’s doctor must order skilled nursing care, which requires the skills and oversight of professional personnel (e.g., registered nurses, licensed practical nurses, ...
How long does it take to get into an inpatient rehab facility?
You’re admitted to an inpatient rehabilitation facility within 60 days of being discharged from a hospital.
What is part A in rehabilitation?
Inpatient rehabilitation care. Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine.
What is the benefit period for Medicare?
benefit period. The way that Original Medicare measures your use of hospital and skilled nursing facility (SNF) services. A benefit period begins the day you're admitted as an inpatient in a hospital or SNF. The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row.
Does Medicare cover outpatient care?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
Does Medicare cover private duty nursing?
Medicare doesn’t cover: Private duty nursing. A phone or television in your room. Personal items, like toothpaste, socks, or razors (except when a hospital provides them as part of your hospital admission pack). A private room, unless medically necessary.
How long does Medicare cover inpatient rehab?
Medicare covers inpatient rehab in a skilled nursing facility – also known as an SNF – for up to 100 days. Rehab in an SNF may be needed after an injury or procedure, like a hip or knee replacement.
What is Medicare Part A?
Published by: Medicare Made Clear. Medicare Part A covers medically necessary inpatient rehab (rehabilitation) care , which can help when you’re recovering from serious injuries, surgery or an illness. Inpatient rehab care may be provided in of the following facilities: A skilled nursing facility.
How long does it take to get Medicare to cover rehab?
The 3-day rule for Medicare requires that you are admitted to the hospital as an inpatient for at least 3 days for rehab in a skilled nursing facility to be covered. You must be officially admitted to the hospital by a doctor’s order to even be considered an inpatient, so watch out for this rule. In cases where the 3-day rule is not met, Medicare ...
What is an inpatient rehab facility?
An inpatient rehabilitation facility (inpatient “rehab” facility or IRF) Acute care rehabilitation center. Rehabilitation hospital. For inpatient rehab care to be covered, your doctor needs to affirm the following are true for your medical condition: 1. It requires intensive rehab.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
How much does Medicare pay for day 150?
You pay 100 percent of the cost for day 150 and beyond in a benefit period. Your inpatient rehab coverage and costs may be different with a Medicare Advantage plan, and some costs may be covered if you have a Medicare supplement plan. Check with your plan provider for details.
What is the medical condition that requires rehab?
To qualify for care in an inpatient rehabilitation facility, your doctor must state that your medical condition requires the following: Intensive rehabilitation. Continued medical supervision.