- Medicare Trust Funds. Medicare pays for Medicare Advantage out of two funds held in trust by the U.S. ...
- Affordable Care Act. The Affordable Care Act guarantees continuous funding of Medicare and Medicare Advantage at least until 2029, according to the Medicare.gov website.
- Premium Payments. ...
- Other Costs to Patients. ...
Full Answer
How is Medicare Advantage funded?
Medicare Advantage, or Part C, is a health insurance program. It is funded from two different sources. The monthly premiums of beneficiaries provide part of the funding. However, the main source is a federal agency called the Centers for Medicare & Medicaid Services, which runs the Medicare program.
Why are Medicare Advantage plans so expensive?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan; if you decide to switch to Medigap, there often are lifetime penalties.
What is a Medicare Advantage plan?
Medicare Advantage plans are all-in-one alternatives to original Medicare offered by private companies. They’re funded by Medicare and by the people signing up for the specific plan. Medicare pays the company offering the Medicare Advantage plan a monthly fixed amount for your care.
Is Medicare Advantage right for You?
It can be an affordable option for patients who are not currently sick or in need of intense medical care. If a patient's situation worsens, it might be difficult or expensive to switch plans. Can I Choose Any Doctor With Medicare Advantage?
What is Medicare Advantage?
What percentage of Medicare is on Advantage plans?
How does Medicare bidding work?
What determines the amount of Medicare payments?
What happens if Medicare bid is lower than benchmark?
What is benchmark Medicare?
What are the sources of Medicare funds?
See more
About this website
What are the sources of revenue for Medicare Advantage plans?
Three sources of revenue for Advantage plans include general revenues, Medicare premiums, and payroll taxes. The government sets a pre-determined amount every year to private insurers for each Advantage member. These funds come from both the HI and the SMI trust funds.
Do Medicare Advantage plans get paid by Medicare?
Rules for Medicare Advantage Plans Health or prescription drug costs that you must pay on your own because they aren't covered by Medicare or other insurance.
What is the biggest disadvantage of Medicare Advantage?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
How profitable is Medicare Advantage?
Medicare Advantage is the common thread. Big-name health insurers raked in $8.2 billion in profit for the fourth quarter of 2019 and $35.7 billion over the course of the year.
How can Medicare Advantage plans have no premiums?
$0 Medicare Advantage plans aren't totally free Medicare Advantage plans are provided by private insurance companies. These companies are in business to make a profit. To offer $0 premium plans, they must make up their costs in other ways. They do this through the deductibles, copays and coinsurance.
What is the biggest difference between Medicare and Medicare Advantage?
With Original Medicare, you can go to any doctor or facility that accepts Medicare. Medicare Advantage plans have fixed networks of doctors and hospitals. Your plan will have rules about whether or not you can get care outside your network. But with any plan, you'll pay more for care you get outside your network.
Can you switch back to Medicare from Medicare Advantage?
Yes, you can elect to switch to traditional Medicare from your Medicare Advantage plan during the Medicare Open Enrollment period, which runs from October 15 to December 7 each year. Your coverage under traditional Medicare will begin January 1 of the following year.
Who is the largest Medicare Advantage provider?
UnitedHealthcareUnitedHealthcare is the largest provider of Medicare Advantage plans and offers plans in nearly three-quarters of U.S. counties.
Do Medicare Advantage plan premiums increase with age?
The way they set the price affects how much you pay now and in the future. Generally the same monthly premium is charged to everyone who has the Medigap policy, regardless of age. Your premium isn't based on your age. Premiums may go up because of inflation and other factors, but not because of your age.
What percentage of Medicare is Medicare Advantage?
In 2021, more than 26 million people are enrolled in a Medicare Advantage plan, accounting for 42 percent of the total Medicare population, and $343 billion (or 46%) of total federal Medicare spending (net of premiums).
What is the most profitable insurance company?
Top 10 Most Profitable Insurance Companies in 2020Berkshire Hathaway. $81.4B.MetLife. $5.9B.State Farm. $5.6B.Allstate. $4.8B.Prudential. $4.2B.USAA. $4B.Progressive. $4B.MassMutual. $3.7B.More items...•
What is the difference between Medicare Advantage and Medigap?
Medigap is supplemental and helps to fill gaps by paying out-of-pocket costs associated with Original Medicare while Medicare Advantage plans stand in place of Original Medicare and generally provide additional coverage.
What is Medicare Advantage?
Medicare Advantage, a health plan provided by private insurance companies, is paid for by federal funding, subscriber premiums and co-payments. It includes the same coverage as the federal government’s Original Medicare program as well as additional supplemental benefits.
How is health insurance funded?
Treasury. The Hospital Insurance Trust Fund is funded by federal payroll taxes and income taxes from Social Security benefits.
What is Supplementary Medical Insurance Fund?
The Supplementary Medical Insurance Fund is composed of funds approved by Congress and Part B and Part D premiums paid by subscribers.
Is Medicare Advantage financed by monthly premiums?
Each insurance company is approved and contracted by Medicare and must fulfill guidelines for coverage as established by the government. Medicare Advantage plans are also financed by monthly premiums paid by subscribers. The premium amounts vary by company and plan.
How many people did Medicare cover in 2017?
programs offered by each state. In 2017, Medicare covered over 58 million people. Total expenditures in 2017 were $705.9 billion. This money comes from the Medicare Trust Funds.
What is Medicare Part B?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. and. Medicare Drug Coverage (Part D) Optional benefits for prescription drugs available to all people with Medicare for an additional charge.
What is the CMS?
The Centers for Medicare & Medicaid Services ( CMS) is the federal agency that runs the Medicare Program. CMS is a branch of the. Department Of Health And Human Services (Hhs) The federal agency that oversees CMS, which administers programs for protecting the health of all Americans, including Medicare, the Marketplace, Medicaid, ...
Does Medicare cover home health?
Medicare only covers home health care on a limited basis as ordered by your doctor. , and. hospice. A special way of caring for people who are terminally ill. Hospice care involves a team-oriented approach that addresses the medical, physical, social, emotional, and spiritual needs of the patient.
What are the sources of revenue for Advantage Plans?
Three sources of revenue for Advantage plans include general revenues, Medicare premiums, and payroll taxes. The government sets a pre-determined amount every year to private insurers for each Advantage member. These funds come from both the H.I. and the SMI trust funds.
What is benchmark amount for Medicare?
Benchmark amounts vary depending on the region. Benchmark amounts can range from 95% to 115% of Medicare costs. If bids come in higher than benchmark amounts, the enrollees must pay the cost difference in a monthly premium. If bids are lower than benchmark amounts, Medicare and the health plan provide a rebate to enrollees after splitting ...
What is supplementary medical insurance?
The supplementary medical insurance trust fund is what’s responsible for funding Part B, as well as operating the Medicare program itself. Part B helps to cover beneficiaries’ doctors’ visits, routine labs, and preventative care.
Will Medicare stop paying hospital bills?
Of course, this isn’t saying Medicare will halt payments on hospital benefits; more likely, Congress will raise the national debt. Medicare already borrows most of the money it needs to pay for the program. The Medicare program’s spending came to over $600 billion, 15% of the federal budget.
Does Medicare Supplement pay for premiums?
Many times, seniors who are retired may have their premiums paid by their former employers. The federal government doesn’t contribute financially to Medigap premiums.
How much does Medicare cost?
In 2018, Medicare spending (net of income from premiums and other offsetting receipts) totaled $605 billion, accounting for 15 percent of the federal budget (Figure 1).
Why is Medicare spending so high?
Over the longer term (that is, beyond the next 10 years), both CBO and OACT expect Medicare spending to rise more rapidly than GDP due to a number of factors, including the aging of the population and faster growth in health care costs than growth in the economy on a per capita basis.
How is Medicare Part D funded?
Part D is financed by general revenues (71 percent), beneficiary premiums (17 percent), and state payments for beneficiaries dually eligible for Medicare and Medicaid (12 percent). Higher-income enrollees pay a larger share of the cost of Part D coverage, as they do for Part B.
How fast will Medicare spending grow?
On a per capita basis, Medicare spending is also projected to grow at a faster rate between 2018 and 2028 (5.1 percent) than between 2010 and 2018 (1.7 percent), and slightly faster than the average annual growth in per capita private health insurance spending over the next 10 years (4.6 percent).
What has changed in Medicare spending in the past 10 years?
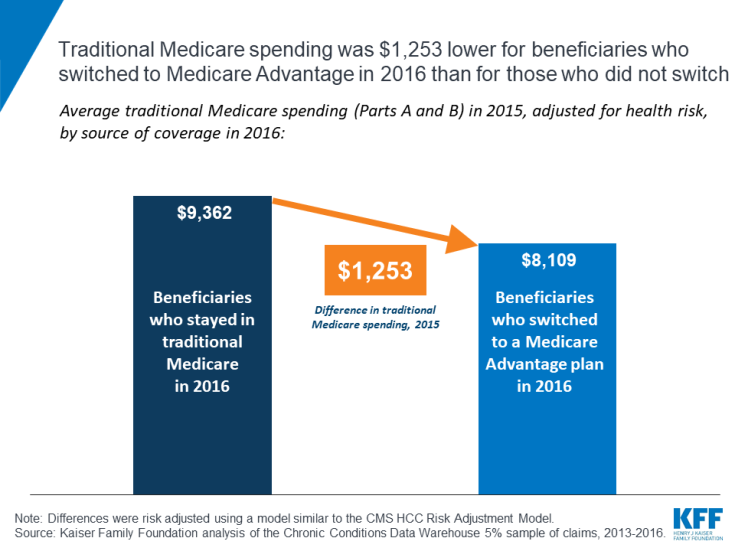
Another notable change in Medicare spending in the past 10 years is the increase in payments to Medicare Advantage plans , which are private health plans that cover all Part A and Part B benefits, and typically also Part D benefits.
How is Medicare's solvency measured?
The solvency of Medicare in this context is measured by the level of assets in the Part A trust fund. In years when annual income to the trust fund exceeds benefits spending, the asset level increases, and when annual spending exceeds income, the asset level decreases.
How much will Medicare per capita increase in 2028?
Medicare per capita spending is projected to grow at an average annual rate of 5.1 percent over the next 10 years (2018 to 2028), due to growing Medicare enrollment, increased use of services and intensity of care, and rising health care prices.
How much of the federal budget is Medicare?
Medicare spending often plays a major role in federal health policy and budget discussions, since it accounts for 21% of national health care spending and 12% of the federal budget. Recent attention has focused on one specific measure of Medicare’s financial condition – the solvency of the Medicare Hospital Insurance (HI) trust fund, ...
Where does Medicare get its money from?
Funding for Medicare comes primarily from general revenues, payroll tax revenues, and premiums paid by beneficiaries (Figure 1). Other sources include taxes on Social Security benefits, payments from states, and interest. The different parts of Medicare are funded in varying ways.
How is Medicare solvency measured?
Medicare solvency is measured by the level of assets in the Part A trust fund. In years when annual income to the trust fund exceeds benefits spending, the asset level increases, and when annual spending exceeds income, the asset level decreases. This matters because when spending exceeds income and the assets are fully depleted, ...
How much would Medicare increase over 75 years?
Over a longer 75-year timeframe, the Medicare Trustees estimated that it would take an increase of 0.76% of taxable payroll over the 75-year period, or a 16% reduction in benefits each year over the next 75 years, to bring the HI trust fund into balance.
How many people are covered by Medicare?
Medicare, the federal health insurance program for more than 60 million people ages 65 and over and younger people with long-term disabilities, helps to pay for hospital and physician visits, prescription drugs, and other acute and post-acute care services. Medicare spending often plays a major role in federal health policy and budget discussions, ...
How much of Medicare will be covered in 2026?
Based on data from Medicare’s actuaries, in 2026, Medicare will be able to cover 94% of Part A benefits spending with revenues plus the small amount of assets remaining at the beginning of the year, and just under 90% with revenues alone in 2027 through 2029.
What is Medicare Advantage Plan?
A Medicare Advantage Plan is intended to be an all-in-one alternative to Original Medicare. These plans are offered by private insurance companies that contract with Medicare to provide Part A and Part B benefits, and sometimes Part D (prescriptions). Most plans cover benefits that Original Medicare doesn't offer, such as vision, hearing, ...
What is Medicare Part A?
Original Medicare. Original Medicare includes Part A (hospital insurance) and Part B (medical insurance). To help pay for things that aren't covered by Medicare, you can opt to buy supplemental insurance known as Medigap (or Medicare Supplement Insurance). These policies are offered by private insurers and cover things that Medicare doesn't, ...
Can you sell a Medigap plan to a new beneficiary?
But as of Jan. 2, 2020, the two plans that cover deductibles—plans C and F— cannot be sold to new Medigap beneficiaries.
Do I have to sign up for Medicare if I am 65?
Coverage Choices for Medicare. If you're older than 65 (or turning 65 in the next three months) and not already getting benefits from Social Security, you have to sign up for Medicare Part A and Part B. It doesn't happen automatically.
Does Medicare cover vision?
Most plans cover benefits that Original Medicare doesn't offer, such as vision, hearing, and dental. You have to sign up for Medicare Part A and Part B before you can enroll in Medicare Advantage Plan.
Does Medicare automatically apply to Social Security?
It doesn't happen automatically. However, if you already get Social Security benefits, you'll get Medicare Part A and Part B automatically when you first become eligible (you don't need to sign up). 4. There are two main ways to get Medicare coverage: Original Medicare. A Medicare Advantage Plan.
Do I need Part D if I don't have Medicare?
Be aware that with Original Medicare and Medigap, you will still need Part D prescription drug coverage, and that if you don't buy it when you first become eligible for it—and are not covered by a drug plan through work or a spouse—you will be charged a lifetime penalty if you try to buy it later. 5.
What is Medicare Advantage?
Medicare spending. Summary. Medicare Advantage, or Part C, is a health insurance program. It is funded from two different sources. The monthly premiums of beneficiaries provide part of the funding. However, the main source is a federal agency called the Centers for Medicare & Medicaid Services, which runs the Medicare program.
What percentage of Medicare is on Advantage plans?
In 2019, Medicare payments to Advantage plans to fund Part A and Part B benefits were $250 billion, according to the Kaiser Family Foundation. This represents 33% of Medicare’s total spending.
How does Medicare bidding work?
First, each plan submits a bid to Medicare, based on the estimated cost of Part A and Part B benefits per person. Next, Medicare compares the amount of the bid against the benchmark.
What determines the amount of Medicare payments?
The amount of the monthly payments depends on two main factors: the healthcare practices in the county where each beneficiary lives, which influences a procedure called the bidding process. the health of each beneficiary, which governs how Medicare raises or lowers the rates, in a system known as risk adjustment.
What happens if Medicare bid is lower than benchmark?
If the bid is lower than the benchmark, the plan gets a rebate from Medicare that is a percentage of the difference between the bid and the benchmark. Plans that receive rebates should use a portion of the rebates to fund supplemental benefits or to reduce premiums.
What is benchmark Medicare?
The benchmark is a percentage of costs of average Medicare spending per individual. Each county in the United States has its own benchmark. It reflects the practice patterns of resident healthcare providers that bill Medicare. Practice patterns differ among counties, so their benchmarks also differ.
What are the sources of Medicare funds?
Two trust funds held by the United States Department of the Treasury supply the money for Medicare payments. The funds are the Hospital Insurance Trust Fund and the Supplemental Medical Insurance Trust fund.
