How Medicare Billing Works
- Medicare sets a value for everything it covers.. Every product and service covered by Medicare is given a value based...
- A health care provider must declare whether or not they accept Medicare assignment.. The overwhelming majority of...
- The provider sends a bill to Medicare that identifies the services rendered to the patient.. After...
What are the requirements for Medicare billing?
- The regular physician is unavailable to provide the service.
- The beneficiary has arranged or seeks to receive the services from the regular physician.
- The locum tenens is NOT an employee of the regular physician.
- The regular physician pays the locum tenens physician on a per diem or fee-for-service basis.
How do I become a Medicare Biller?
What Is an Insurance Biller?
- Get Trained. Formal training in insurance billing is available at vocational schools and community colleges in the form of diploma, certificate and associate's degree programs.
- Obtain Certification. Licensure is not required for insurance billers; however, obtaining professional certification is highly recommended.
- Acquire Work Experience. ...
Who do I call for Medicare billing questions?
- Home & Community Based Services Authorities
- HCBS Training
- Guidance
- Statewide Transition Plans
- Technical Assistance
How to bill Medicare as secondary payer?
What it means to pay primary/secondary
- The insurance that pays first (primary payer) pays up to the limits of its coverage.
- The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover.
- The secondary payer (which may be Medicare) may not pay all the uncovered costs.

Who processes Original Medicare claims?
Medicare Claims and Reimbursement If you have Original Medicare, Part A and/or Part B, your doctor and supplier are required to file Medicare claims for covered services and supplies you receive. If your doctor or the supplier doesn't file a claim, you can call Medicare at 1-800-MEDICARE (1-800-633-4227).
How is a Medicare claim submitted?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
How long does it take Medicare to pay a bill?
around 30 daysFor clean claims that are submitted electronically, they are generally paid within 14 calendar days by Medicare. The processing time for clean paper claims is a bit longer, usually around 30 days. These timelines are for initial claims.
How do doctors bill Medicare?
If you're on Medicare, your doctors will usually bill Medicare for any care you obtain. Medicare will then pay its rate directly to your doctor. Your doctor will only charge you for any copay, deductible, or coinsurance you owe.
What is the first step in submitting Medicare claims?
The first thing you'll need to do when filing your claim is to fill out the Patient's Request for Medical Payment form. ... The next step in filing your own claim is to get an itemized bill for your medical treatment.More items...•
How do providers get reimbursed by Medicare?
Traditional Medicare reimbursements When an individual has traditional Medicare, they will generally never see a bill from a healthcare provider. Instead, the law states that providers must send the claim directly to Medicare. Medicare then reimburses the medical costs directly to the service provider.
Can a patient bill Medicare directly?
If you have Original Medicare and a participating provider refuses to submit a claim, you can file a complaint with 1-800-MEDICARE. Regardless of whether or not the provider is required to file claims, you can submit the healthcare claims yourself.
How long does a Medicare rebate take to process?
As long as your details and bank account is registered with Medicare we should be able to process this for you immediately after taking payment for your consultation. Your rebate will usually be back in your bank account within one to two business days.
Confirm Financial Responsibility
Financial responsibility describes who owes what for a particular doctor’s visit. Once the biller has the pertinent info from the patient, that bil...
Patient Check-In and Check-Out
Patient check-in and check-out are relatively straight-forward front-of-house procedures. When the patient arrives, they will be asked to complete...
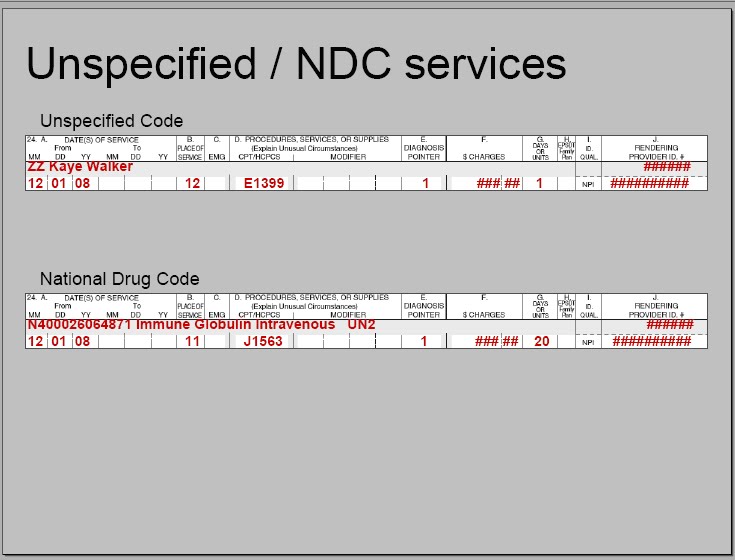
Prepare Claims/Check Compliance
The medical biller takes the superbill from the medical coder and puts it either into a paper claim form, or into the proper practice management or...
Generate Patient Statements
Once the biller has received the report from the payer, it’s time to make the statement for the patient. The statement is the bill for the procedur...
Follow Up on Patient Payments and Handle Collections
The final phase of the billing process is ensuring those bills get, well, paid. Billers are in charge of mailing out timely, accurate medical bills...
How does Medicare billing work?
1. Medicare sets a value for everything it covers. Every product and service covered by Medicare is given a value based on what Medicare decides it’s worth.
What does it mean when a provider accepts a Medicare assignment?
“Accepting assignment” means that a doctor or health care provider has agreed to accept the Medicare-approved amount as full payment for their services.
What percentage of Medicare is coinsurance?
For example, the patient is responsible for 20 percent of the Medicare-approved amount while Medicare covers the remaining 80 percent of the cost. A copayment is typically a flat-fee that is charged to the patient.
What happens if a provider doesn't accept Medicare?
If a provider chooses not to accept assignment, they may still treat Medicare patients but will be allowed to charge up to 15 percent more for their product or service. These are known as “excess charges.”. 3.
Does Medicare cover out of pocket expenses?
Some of Medicare’s out-of-pocket expenses are covered partially or in full by Medicare Supplement Insurance. These are optional plans that may be purchased from private insurance companies to help cover some copayments, deductibles, coinsurance and other Medicare out-of-pocket costs.
Is Medicare covered by coinsurance?
Some services are covered in full by Medicare and the patient is left with no financial responsibility. But most products and services require some cost sharing between patient and provider.This cost sharing can come in the form of either coinsurance or copayments. Coinsurance is generally measured in a percentage.
How does Medicare receive claims?
Your Medigap (supplemental insurance) company or retiree plan receives claims for your services 1 of 3 ways: Directly from Medicare through electronic claims processing. This is done online. Directly from your provider, if he/she accepts Medicare assignment. This is done online, by fax or through the mail.
How to file a claim with Medicare?
Follow these steps: Fill out the claim form provided by your insurance company (if required). Attach copies of the bills you are submitting for payment (if required). Attach copies of the MSN related to those bills.
How much does Medicare pay for Part B?
If the provider accepts assignment (agrees to accept Medicare’s approved amount as full reimbursement), Medicare pays the Part B claim directly to him/her for 80% of the approved amount. You are responsible for the remaining 20% (this is your coinsurance ). If the provider does not accept assignment, he/she is required to submit your claim ...
Is MSN a bill?
How much Medicare approved and paid. How much you owe. Previously known as the Explanation of Medicare Benefits, the MSN is not a bill. You should not send money to Medicare after receiving an MSN. Your provider will bill you separately.
Does Medicare send a bill for MSN?
For more information, see Assignment for Original Fee-for-Service Medicare . Medicare will send you a Medicare Summary Notice (MSN) form each quarter. Previously known as the Explanation of Medicare Benefits, the MSN is not a bill. You should not send money to Medicare after receiving an MSN.
What is the final phase of billing?
The final phase of the billing process is ensuring those bills get, well, paid. Billers are in charge of mailing out timely, accurate medical bills, and then following up with patients whose bills are delinquent. Once a bill is paid, that information is stored with the patient’s file.
What is the process of a medical claim being accepted?
Once a claim reaches a payer, it undergoes a process called adjudication. In adjudication, a payer evaluates a medical claim and decides whether the claim is valid/compliant and, if so, how much of the claim the payer will reimburse the provider for. It’s at this stage that a claim may be accepted, denied, or rejected.
What does a medical biller do?
The medical biller takes the superbill from the medical coder and puts it either into a paper claim form, or into the proper practice management or billing software. Biller’s will also include the cost of the procedures in the claim. They won’t send the full cost to the payer, but rather the amount they expect the payer to pay, as laid out in the payer’s contract with the patient and the provider.
What is an EOB in a bill?
In certain cases, a biller may include an Explanation of Benefits (EOB) with the statement. An EOB describes what benefits, and therefore what kind of coverage, a patient receives under their plan. EOBs can be useful in explaining to patients why certain procedures were covered while others were not.
What is a statement in a bill?
The statement is the bill for the procedure or procedures the patient received from the provider. Once the payer has agreed to pay the provider for a portion of the services on the claim, the remaining amount is passed to the patient.
What happens if there are discrepancies in a biller's fees?
If there are any discrepancies, the biller/provider will enter into an appeal process with the payer.
What does "accepted" mean in medical billing?
Accepted does not necessarily mean that the payer will pay the entirety of the bill. Rather, they will process the claim within the rules of the arrangement they have with their subscriber (the patient). A rejected claim is one that the payer has found some error with.
How long does it take for Medicare to process a claim?
Medicare claims to providers take about 30 days to process. The provider usually gets direct payment from Medicare. What is the Medicare Reimbursement fee schedule? The fee schedule is a list of how Medicare is going to pay doctors. The list goes over Medicare’s fee maximums for doctors, ambulance, and more.
What happens if you see a doctor in your insurance network?
If you see a doctor in your plan’s network, your doctor will handle the claims process. Your doctor will only charge you for deductibles, copayments, or coinsurance. However, the situation is different if you see a doctor who is not in your plan’s network.
Does Medicare cover out of network doctors?
Coverage for out-of-network doctors depends on your Medicare Advantage plan. Many HMO plans do not cover non-emergency out-of-network care, while PPO plans might. If you obtain out of network care, you may have to pay for it up-front and then submit a claim to your insurance company.
Do participating doctors accept Medicare?
Most healthcare doctors are “participating providers” that accept Medicare assignment. They have agreed to accept Medicare’s rates as full payment for their services. If you see a participating doctor, they handle Medicare billing, and you don’t have to file any claim forms.
Do you have to pay for Medicare up front?
But in a few situations, you may have to pay for your care up-front and file a claim asking Medicare to reimburse you. The claims process is simple, but you will need an itemized receipt from your provider.
Do you have to ask for reimbursement from Medicare?
If you are in a Medicare Advantage plan, you will never have to ask for reimbursement from Medicare. Medicare pays Advantage companies to handle the claims. In some cases, you may need to ask the company to reimburse you. If you see a doctor in your plan’s network, your doctor will handle the claims process.
Can a doctor ask for a full bill?
In certain situations, your doctor may ask you to pay the full cost of your care–either up-front or in a bill; this might happen if your doctor doesn’t participate in Medicare. If your doctor doesn’t bill Medicare directly, you can file a claim asking Medicare to reimburse you for costs that you had to pay.