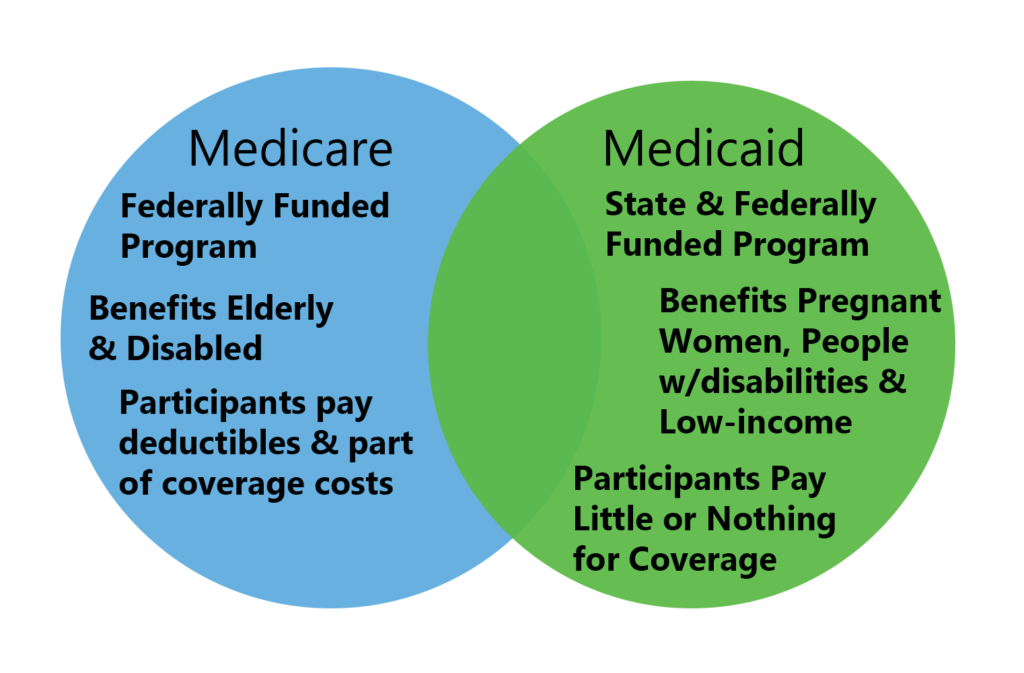
In effect, each state program combines federal funds and state resources to meet federal quality standards. Regardless of which state a person lives in, Medicare eligibility is based on U.S. citizenship, age, or disability status. On the other hand, Medicaid
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
Full Answer
How does Medicare work in my state?
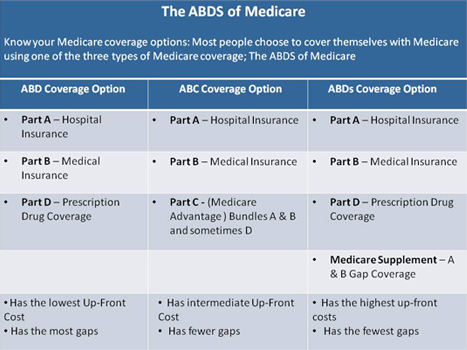
Medicare is the federal health services program for American seniors and those of any age with disabilities. Divided into several focused parts, Medicare provides preventive and diagnostic medical care, prescription drugs, and hospital stays. In short, Medicare provides the same nationwide coverage regardless of which state you live in.
Are Medicare plans different in each state?
But while these provisions apply nationwide, plan availability and prices are different from one state to another. Medicare uses a star rating system for Medicare Advantage and Part D plans, and the availability of high-quality plans is not the same in every state.
How are Medicare premiums determined?
Medicare premiums are based off how much you earned two years ago. Your modified adjusted gross income will determine what you pay for Medicare coverage.
What is the Medicare Coverage Determination process?
Medicare Coverage Determination Process. Medicare coverage is limited to items and services that are reasonable and necessary for the diagnosis or treatment of an illness or injury (and within the scope of a Medicare benefit category).
Is Medicare specific to each state?
Original Medicare (Part A and Part B) is a federal program so your coverage, costs and benefits will not be different from state to state. Medicare Advantage, Medicare Part D and Medigap plans are available through private insurers. These optional Medicare plans are regulated by each state and tend to vary.
Is Medicare determined by where you live?
Since Original Medicare is a completely federal program, it's equally available to residents in all U.S. states. However, certain programs within Medicare vary from state to state in terms of rules, availability, and pricing.
Is Medicare based on state or federal?
Medicare is a federal program. It is basically the same everywhere in the United States and is run by the Centers for Medicare & Medicaid Services, an agency of the federal government.
Do Medicare rates differ by state?
The Medicare premium for Part B varies based on your income level, rather than your location. The standard monthly premium is $148.50 in 2021. Your Part B premium may be more if your income is above a certain level. As with Part A, the Part B premium doesn't change across the states.
What are the 3 requirements for Medicare?
Be age 65 or older; Be a U.S. resident; AND. Be either a U.S. citizen, OR. Be an alien who has been lawfully admitted for permanent residence and has been residing in the United States for 5 continuous years prior to the month of filing an application for Medicare.
What income is used to determine Medicare premiums?
modified adjusted gross incomeMedicare uses the modified adjusted gross income reported on your IRS tax return from 2 years ago. This is the most recent tax return information provided to Social Security by the IRS.
Who decides Medicare coverage?
Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
What is the highest income to qualify for Medicaid?
Federal Poverty Level thresholds to qualify for Medicaid The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.
How does the government pay for Medicare?
Medicare is funded primarily from general revenues (43 percent), payroll taxes (36 percent), and beneficiary premiums (15 percent) (Figure 7). Part A is financed primarily through a 2.9 percent tax on earnings paid by employers and employees (1.45 percent each) (accounting for 88 percent of Part A revenue).
Can you have Medicare in two states?
You can have Medicare while living in two states, but you'll choose one location as your primary residence. There will be some Medicare plans that benefit you more than others when you have multiple homes. Some retired people choose to reside in two different locations.
What states don't have Medicare?
Nonexpansion states include 12 states that have not expanded Medicaid: Alabama, Florida, Georgia, Kansas, Mississippi, North Carolina, South Carolina, South Dakota, Tennessee, Texas, Wisconsin, and Wyoming. Data: Urban Institute's Health Insurance Policy Simulation Model (HIPSM), 2021.
Does Medicare cover nationwide?
Original Medicare provides nationwide coverage, whereas Medicare Advantage plans have provider networks that can be limited to a local area.
How many people pay Medicare Part B?
States pay Medicare Part B premiums each month for over 10 million individuals and Part A premium for over 700,000 individuals.
When was the Medicare buy in manual released?
Manual for State Payment of Medicare Premiums (formerly called “State Buy-in Manual”) On September 8, 2020, the Centers for Medicare & Medicaid Services (CMS) released an updated version of the Manual for State Payment of Medicare Premiums (formerly called “State Buy-in Manual”). The manual updates information and instructions to states on federal ...
What states require community rating for Medigap?
As of 2018, eight states (Arkansas, Connecticut, Massachusetts, Maine, Minnesota, New York, Vermont, and Washington) required carriers to use community rating.
How many seniors will be covered by Medicare in 2021?
July 7, 2021. facebook2. twitter2. comment. Medicare is a federal program, covering more than 63 million seniors and disabled Americans throughout the country. Medicare beneficiaries in most areas have the option to get their coverage via private Medicare Advantage plans, and more than four out of ten do so.
How long does Medicare coverage last?
Medigap coverage is guaranteed issue for six months, starting when you’re at least 65 and enrolled in Medicare Parts A and B.
When is Medicare Part D open enrollment?
Federal guidelines call for an annual open enrollment period (October 15 to December 7) for Medicare Advantage and Medicare Part D coverage in every state. And as of 2019, there’s also a Medicare Advantage open enrollment period (January 1 through March 31) that allows people who already have Medicare Advantage to switch to a different Advantage plan or switch to Original Medicare. But while these provisions apply nationwide, plan availability and prices are different from one state to another.
How many Part D prescriptions will be available in 2021?
Part D prescription drug plan availability differs from state to state as well, with the number of plans for sale in 2021 varying from 25 to 35, depending on the region. The number of available premium-free (“benchmark”) prescription plans for low-income enrollees varies from five to ten, depending on the state.
Does Alaska have Medicare Advantage?
Not surprisingly, the popularity of Medicare Advantage plans varies significantly from one state to another, with only one percent of the Medicare population enrolled in Advantage plans in A laska. (There are no individual Medicare Advantage plans available at all in Alaska.
Can you switch to a different Medigap plan in Maine?
In Maine, Medigap enrollees can switch to a different Medigap plan with the same or lesser benefits at any time during the year, and all carriers must designate one month each year when Medigap Plan A is available on a guaranteed issue basis to all enrollees.
How much will Medicare premiums be in 2021?
There are six income tiers for Medicare premiums in 2021. As stated earlier, the standard Part B premium amount that most people are expected to pay is $148.50 month. But, if your MAGI exceeds an income bracket — even by just $1 — you are moved to the next tier and will have to pay the higher premium.
How much of Medicare Part B is paid?
But the remaining 25% of Medicare Part B expenses are paid through your premium, which is determined by your income level. Medicare prices are quoted under the assumption you have an average income. If your income level exceeds a certain threshold, you will have to pay more.
Why did Medicare Part B premiums increase in 2021?
That’s because 2021 Medicare Part B premiums increased across the board due to rising healthcare costs. Exactly how much your premiums increased though, isn’t based on your current health or Medicare plan or your income. Rather, it’s the soaring prices of overall healthcare.
What is Medicare Advantage?
Essentially: Medicare Advantage – Private plans that replace your Parts A, B, and in most cases, D. Also known as Part C. Medicare Part D – Prescription drug coverage plans, introduced in 2006. Generally, if you’re on Medicare, you aren’t charged a premium for Part A.
Why are Social Security beneficiaries paying less than the full amount?
In 2016, 2017, and 2018, the Social Security COLA amount for most beneficiaries wasn’t enough to cover the full cost of the Part B premium increases, so most enrollees were paying less than the full amount, because they were protected by the hold harmless rule.
Is Medicare Part D tax deductible?
Also known as Part C. Medicare Part D – Prescription drug coverage plans, introduced in 2006. Generally, if you’re on Medicare, you aren’t charged a premium for Part A. However, you are charged monthly premiums for Part B and Part D, and can also be charged for Part C, depending on the plan you select. These premiums are tax-deductible but very few ...
Does Medicare Part B get deducted from Social Security?
Medicare Part B premiums are deducted from Social Security checks, and Social Security benefit amounts are adjusted annually by the cost-of-living adjustment (COLA).
What is the federal government's role in Medicaid?
The federal government watches the quality of care that states use when providing Medicaid assistance. In effect, each state program is a combination of federal funds, federal quality standards, and state resources.
What is Medicare for older people?
Medicare is the national health services program for older Americans. It has several parts designed to make a comprehensive healthcare system. It provides medical care, prescription drugs, and hospital care. The federal government has a strong legal responsibility when carrying out Medicare. It must keep a rule of medical necessity.
What does Medicare Supplement require?
States require a combination of comprehensive plans along with any limited option plans. The insurance companies can use medical underwriting to determine process, discriminate against applicants and reject applications.
What is Medicare Advantage?
The private insurance plans in Medicare Advantage offer a wide variety of choices for consumers. There is another level of choice, and that is the managed care organizations. The balancing of resources, prices, and consumer costs require trade-offs. High premiums go along with low deductibles and out-of-pocket costs.
What is the massive undertaking to insure a national and diverse population?
The massive undertaking to insure a national and diverse population requires technical expertise and consistency. The Centers for Medicare and Medicaid use several networks of private contractors to process claims and maintain records.
Why did states turn down federal funds?
States turned down federal funds to expand coverage to their vulnerable residents. They declined although expansion would have reduced the numbers of uninsured residents and avoided the weight of unpaid bills that plague local hospitals and clinics.
Is Medicare a private or government program?
The Congress later added the Prescription Drug benefit and the private sector style of health insurance in Medicare Advantage. The Original Medicare is a government run program for medical services and hospital care. Users are free to select among doctors and hospitals that agree to accept the Medicare assignment of fees and payments.
Medicare Advantage Plan (Part C)
Monthly premiums vary based on which plan you join. The amount can change each year.
Medicare Supplement Insurance (Medigap)
Monthly premiums vary based on which policy you buy, where you live, and other factors. The amount can change each year.
Which states have the lowest Medicare premiums?
Florida, South Carolina, Nevada, Georgia and Arizona had the lowest weighted average monthly premiums, with all five states having weighted average plan premiums of $17 or less per month. The highest average monthly premiums were for Medicare Advantage plans in Massachusetts, North Dakota and South Dakota. *Medicare Advantage plans are not sold in ...
What is the second most popular Medicare plan?
Medigap Plan G is, in fact, the second-most popular Medigap plan. 17 percent of all Medigap beneficiaries are enrolled in Plan G. 2. The chart below shows the average monthly premium for Medicare Supplement Insurance Plan G for each state in 2018. 3.
How to contact Medicare Advantage 2021?
New to Medicare? Compare Medicare plan costs in your area. Compare Plans. Or call. 1-800-557-6059. 1-800-557-6059 TTY Users: 711 to speak with a licensed insurance agent.
How is medicaid funded?
Medicaid is funded through both federal and state funds. While states are required to provide health insurance coverage to specific groups, each state can determine its own income requirements and eligibility guidelines. You do not get Medicaid automatically; you must apply to know if you’re eligible.
How to apply for medicaid in Wyoming?
How to apply: To apply online, visit the Wyoming Eligibility System, request an application over the phone by calling 1-855-294-2127 or apply through the Health Insurance Marketplace. For more information, visit the Wyoming Medicaid website.
What is Medicaid for low income?
Medicaid is a public assistance program funded by both federal and state governments that covers the medical costs for low-income children, pregnant women, people with disabilities and adults over the age of 65. In some states, low-income adults are also covered.
Does each state have its own medicaid website?
Medicaid plans. Each state has its own Medicaid website that includes coverage information like which providers are available and covered, as well as other benefits. If you have a particular doctor you would like to use, make sure to choose a plan that includes that doctor.
Is Medicare a magi or magi?
And some groups, including those who have a disability and those on Medicare, may also have a choice between MAGI and non-MAGI Medicaid, with non-MAGI Medicaid having slightly different income and resource guidelines for eligibility and services.
Is Medicaid income based?
Medicaid, on the other hand, is income-based and provides coverage for anyone of any age as long as they meet the income requirements and other eligibility requirements for their respective group. Some people may qualify for both government programs; this is called dual-eligibility.
Does Missouri have Medicaid?
Missouri. Eligibility: Missouri Medicaid covers children, pregnant women, parents/caretakers, people with disabilities and adults over 65. The state did not vote to expand coverage to include all low-income adults, although the state may offer coverage to some adults with limitations and an enrollment cap.
How many credits can you earn on Medicare?
Workers are able to earn up to four credits per year. Earning 40 credits qualifies Medicare recipients for Part A with a zero premium.
What is Medicare's look back period?
How Medicare defines income. There is a two-year look-back period, meaning that the income range referenced is based on the IRS tax return filed two years ago. In other words, what you pay in 2020 is based on what your yearly income was in 2018. The income that Medicare uses to establish your premium is modified adjusted gross income (MAGI).
How does Medicare affect late enrollment?
If you do owe a premium for Part A but delay purchasing the insurance beyond your eligibility date, Medicare can charge up to 10% more for every 12-month cycle you could have been enrolled in Part A had you signed up. This higher premium is imposed for twice the number of years that you failed to register. Part B late enrollment has an even greater impact. The 10% increase for every 12-month period is the same, but the duration in most cases is for as long as you are enrolled in Part B.