Who is paying for Medicaid expanded programs?
The federal government is financing most of the cost of expanding Medicaid, and a small portion is being paid by participating states. The costs for enrollees who are newly eligible under the expanded guidelines were covered 100% by the federal government until the end of 2016.
How many states have expanded Medicaid under the ACA?
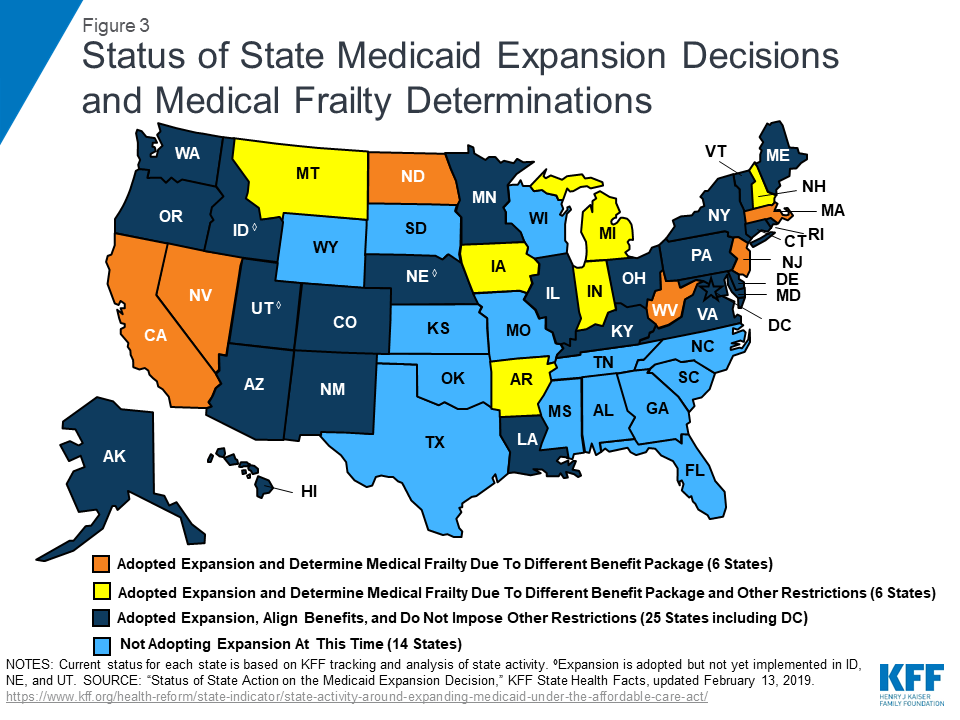
Thirty-eight states and DC have expanded Medicaid under the ACA. Twelve states continue to refuse to adopt Medicaid expansion, despite the fact that the federal government will always pay 90% of the cost. Nearly 19 million Americans had gained coverage as of 2021 through the ACA’s Medicaid expansion.
How do States pay for Medicaid?
States finance the nonfederal share of their Medicaid expenditures in large part through general revenues, which consist of revenue from sources including personal and corporate income taxes and sales taxes.
When will enrollment in Medicaid coverage under expansion begin?
Enrollment in Medicaid coverage under expansion began on November 1, 2019, and coverage for these enrollees began on January 1, 2020.
Do states contribute to Medicare?
Medicare is federally administered and covers older or disabled Americans, while Medicaid operates at the state level and covers low-income families and some single adults. Funding for Medicare is done through payroll taxes and premiums paid by recipients. Medicaid is funded by the federal government and each state.
How many states in the US subscribe to the Medicaid expansion?
Medicaid expansion states: Key takeaways. 38 states and DC have accepted federal funding to expand Medicaid under the ACA.
What states do not have the Affordable Care Act?
Nonexpansion states include 12 states that have not expanded Medicaid: Alabama, Florida, Georgia, Kansas, Mississippi, North Carolina, South Carolina, South Dakota, Tennessee, Texas, Wisconsin, and Wyoming. Data: Urban Institute's Health Insurance Policy Simulation Model (HIPSM), 2021.
How much would Medicaid expansion cost North Carolina?
In North Carolina, where about 2.7 million residents are enrolled in Medicaid, that additional funding would give the state $1.5 billion over two years if it adopts expansion, according to the AP report.
Why has Florida not expanded Medicaid?
Florida has set below-average limits for the mandatory coverage groups, and since the state has not accepted federal funding to expand Medicaid, the eligibility rules have not changed with the implementation of the ACA.
Why did NC not expand Medicaid?
North Carolina has an unprecedented opportunity to provide health care to those currently without insurance through Medicaid expansion. The NC General Assembly has rejected federal dollars to expand Medicaid for the last five years, repeatedly choosing politics over the health and well-being of North Carolinians.
Why is Medicaid expansion unconstitutional?
2 The most complex part of the Court's decision concerned the ACA's Medicaid expansion: a majority of the Court found the ACA's Medicaid expansion unconstitutionally coercive of states because states did not have adequate notice to voluntarily consent to this change in the Medicaid program, and all of a state's ...
Is Obamacare the same in every state?
The availability and cost of health plans also vary by state. This is because each state has their own exchange, as well as different regional populations and demographics, varying the state's providers and number of plans.
What is the highest income to qualify for Medicaid?
Federal Poverty Level thresholds to qualify for Medicaid The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.
Did NC adopt Medicaid expansion?
North Carolina has thus far failed to expand Medicaid, and is one of 11 states where a “coverage gap” still exists. New state budget calls for a legislative committee to study Medicaid expansion in 2022. North Carolina's Medicaid program transitioned to a managed care model in July 2021 after several delays.
Who could Medicaid reach with expansion in North Carolina?
The ACA expanded Medicaid coverage to nearly all adults with incomes up to 138% of the Federal Poverty Level ($17,609 for an individual in 2020).
Is Tennessee expanding Medicaid?
Tennessee has not expanded Medicaid coverage (which is called TennCare) as allowed under the Affordable Care Act, which means that there are an estimated 118,000 residents in the coverage gap — ineligible for Medicaid and also ineligible for premium subsidies in the exchange.
What is the name of the state that will replace the state's Medicaid expansion?
Arkansas. In April 2021, Governor Asa Hutchinson signed a bill passed by the Arkansas Legislature that would replace the state’s current Medicaid expansion program, Arkansas Works, with the Arkansas Health and Opportunity for Me (HOME) program, contingent on federal approval.
What are the effects of Medicaid expansion?
Effects of the ACA Medicaid Expansion on Racial Disparities in Health and Health Care. The Coverage Gap: Uninsured Poor Adults in States that Do Not Expand Medicaid.
Why did Governor Cooper veto the SFY 2020-2021 budget?
In 2019, Governor Cooper vetoed the SFY 2020-2021 budget passed by the Republican-controlled legislature due to omission of Medicaid expansion, and the 2019 legislative session resulted in a budget impasse.
How many states have Medicaid in 2021?
Published: Jul 09, 2021. To date, 39 states (including DC) have adopted the Medicaid expansion and 12 states have not adopted the expansion. Current status for each state is based on KFF tracking and analysis of state expansion activity. These data are available in a table format. The map may be downloaded as a PowerPoint slide.
Why is Medicaid not expanding in 2021?
On June 23, 2021, the judge ruled in favor of DSS, finding that the state’s refusal to expand Medicaid is not unlawful because the initiated amendment violated the state constitution by failing to provide a funding source.
When will the FPL waiver be effective?
On December 23, 2019, CMS approved certain provisions in the state’s “Fallback Plan” waiver request to amend its Primary Care Network Waiver to expand Medicaid eligibility to 138% FPL, effective January 1, 2020; the approval also included work requirements for the newly expanded adult Medicaid population. Virginia.
When will Medicaid be available in Oklahoma?
Oklahoma. Enrollment in Medicaid coverage under expansion in Oklahoma began on June 1, 2021, with coverage for these enrollees beginning on July 1, 2021. Oklahoma voters approved a ballot measure on June 30, 2020 which added Medicaid expansion to the state’s Constitution. Language in the approved measure prohibits the imposition ...
When will the FMAP increase be extended?
That FMAP increase will remain in effect until March 31, 2021, though the Administration has indicated that it is likely to extend the deadline. As a result, much of the increased Medicaid spending resulting from the pandemic will fall to the federal government.
What is Medicaid 2021?
Feb 22, 2021. Medicaid is a joint federal-state program that provides health insurance targeted to lower-income recipients. The program plays a significant role in the U.S. health system, providing medical care for about 22 percent of the population. As a key part of the safety net, Medicaid is designed to be countercyclical, ...
How is Medicaid matched?
Each state’s Medicaid expenditures for healthcare services are matched by federal funds according to various formulas. The formula that governs the majority of government funding takes into account differences in per capita income among the states and is called the federal medical assistance percentages (FMAP). The FMAP ranges from a minimum of 50 percent in wealthier states such as California to 78 percent in Mississippi. The matching structure provides states with resources that automatically adjust for demographic and economic shifts, healthcare costs, public health emergencies, and natural disasters.
How much did the 2020 stimulus cost?
According to the National Association of State Budget Officers, in fiscal year 2020 (which for most states is July 1–June 30) the program cost a total of $647 billion, about $241 billion of which was the nonfederal share. TWEET THIS.
What is the most prominent example of the Affordable Care Act?
The most prominent example stems from the Affordable Care Act (ACA), which expanded the Medicaid program to cover individuals with incomes up to 138 percent of the poverty level ; the federal government covers nearly all the cost of coverage for the expansion population.
How many people did Medicare cover in 2017?
programs offered by each state. In 2017, Medicare covered over 58 million people. Total expenditures in 2017 were $705.9 billion. This money comes from the Medicare Trust Funds.
What is Medicare Part B?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. and. Medicare Drug Coverage (Part D) Optional benefits for prescription drugs available to all people with Medicare for an additional charge.
What is the CMS?
The Centers for Medicare & Medicaid Services ( CMS) is the federal agency that runs the Medicare Program. CMS is a branch of the. Department Of Health And Human Services (Hhs) The federal agency that oversees CMS, which administers programs for protecting the health of all Americans, including Medicare, the Marketplace, Medicaid, ...
What is covered by Part A?
Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. The health care items or services covered under a health insurance plan. Covered benefits and excluded services are defined in the health insurance plan's coverage documents.
Who pays payroll taxes?
Payroll taxes paid by most employees, employers, and people who are self-employed. Other sources, like these: Income taxes paid on Social Security benefits. Interest earned on the trust fund investments. Medicare Part A premiums from people who aren't eligible for premium-free Part A.
Does Medicare cover home health?
Medicare only covers home health care on a limited basis as ordered by your doctor. , and. hospice. A special way of caring for people who are terminally ill. Hospice care involves a team-oriented approach that addresses the medical, physical, social, emotional, and spiritual needs of the patient.
How many states have expanded Medicaid?
36 states and the District of Columbia have expanded Medicaid as of early 2021, and two more — Oklahoma and Missouri — will expand Medicaid in mid-2021. Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006.
How does Medicaid expansion affect the state?
The cost of Medicaid expansion can sometimes be offset by increased revenues for the state, including revenue from taxes/fees assessed on hospitals, medical providers, and insurers, increased tax revenue due to economic growth linked to Medicaid expansion, and premiums that some states require some Medicaid expansion enrollees to pay.
Why is Medicaid expansion important?
There are a few reasons for that: Medicaid expansion allows some states to shift certain populations from traditional Medicaid eligibility to the Medicaid expansion category, where the federal government pays a much larger portion of the cost.
How much does Medicaid pay in 2020?
The federal government’s portion gradually dropped to 90 percent by 2020, and it now stays there permanently (for perspective, under traditional Medicaid, states can pay up to 50 percent of the cost ).
When did the federal government pay for the expansion?
The federal government paid the full cost of expansion from 2014 through 2016. The federal government's portion gradually dropped to 90 percent by 2020, and will stay there permanently. Q.
Does Medicaid cover 10 percent of the cost?
For states that expand Medicaid, the federal funding they receive will always dwarf the amount that the state has to spend. And although states have to cover 10 percent of the cost of Medicaid expansion, their net spending can be much less than that — even negative in some cases. There are a few reasons for that:
How much will the Senate bill increase Medicaid?
Calculations of state costs, derived from the coverage and federal cost estimates prepared by the Centers for Medicare and Medicaid Services (CMS), show that the Senate bill would increase state Medicaid spending—for both benefits and administration—by $32.6 billion for FY 2014 to FY 2019, while the increased Medicaid costs to states under the House bill would be $60 billion for FY 2013 to FY 2019. [3]
How does the House and Senate health care bill increase health insurance coverage?
Both the House and Senate health care bills would increase health insurance coverage principally by expanding the federal–state Medicaid program. In fact, depending on the version enacted, the Medicaid expansion would account for between three-fifths and four-fifths of the projected reduction in the uninsured population under the legislation.
What is the last minute inclusion in the Senate bill of provisions?
The last-minute inclusion in the Senate bill of provisions giving three states special Medicaid funding deals has generated considerable attention and controversy. [4] Table 3 projects the savings to the three states from their special Medicaid funding deals.
How much is Medicaid spending?
In fiscal year (FY) 2018, total Medicaid spending was estimated at $616.1 billion, with spending on the newly eligible adults ( CMS 2020 ). [1]
How much will the US government spend on adult expansion in 2027?
Over the next decade (2018 to 2027), spending on the adult expansion population is expected to grow from $74.2 billion in 2018 to $124.3 billion in 2027. Due to the higher federal matching rate, the vast majority (91 percent) of this spending will be paid for by the federal government ( CMS 2020 ).
What was the impact of Medicaid in 2014?
In 2014, high Medicaid spending growth rates nationally reflected the combined effects of increased enrollment as well as increased spending per enrollee. Along with new high-cost drugs and a required increase in primary care payments, expanded coverage for adults was a key driver of spending growth rates. However, spending growth rates were lower for 2015–2017 and are projected to be even lower for 2018 ( CMS 2020 ). This is due, in part, to the initial 2014 surge in enrollment continuing to diminish ( Keehan et al. 2016 ).
Is Medicaid expansion good for the state budget?
Although the share of Medicaid spending borne by states has increased as states take on a larger share of the costs for the newly eligible, there is some evidence to indicate that Medicaid expansion has been beneficial for state budgets.
Who is eligible for 100 percent matching?
Individuals eligible to receive the 100 percent matching rate included those who would not have been eligible for Medicaid in the state as of December 1, 2009, or who were eligible under a waiver but not enrolled because of limits or caps on waiver enrollment. As of June 2019, there were 14.8 million enrollees in the new group in ...
Is enrollment slowing in 2019?
States have reported that spending and enrollment growth continued to slow in 2018 and 2019. A strong economy, resumption of redeterminations in states that had previously delayed them due to eligibility system upgrades, and improved data matching capabilities, contributed to enrollment declines in FY 2019 ( MACPAC 2019 ).
Is the traditional matching rate increased?
Specifically, the traditional matching rate was increased by a transition factor so that in 2020 it is equal to the federal matching rate for newly eligible adults (see table below).
