How are Medicare Advantage plans combined when calculating quality ratings?
All plans that are part of a single Medicare Advantage contract are combined when calculating the quality rating (most contracts include several plans).
What is a star rating for Medicare Advantage plans?
Medicare Advantage plans receive a star rating based on performance measures that are intended to help potential enrollees compare plans available in their area as well as encourage plans to compete based on quality.
How are quality ratings calculated?
Typically, quality ratings are calculated annually based on data from the previous year. However, due to the COVID-19 pandemic and disruptions to data collection, as well as “to avoid inadvertently creating incentives to place cost considerations above patient safety ”, CMS modified the calculation of 2021 star ratings.
What is the benchmark for Medicare Advantage Medicare Advantage plans?
The benchmark for plans that receive at least 4 stars is increased by 5 percent in most counties, and by 10 percent in double bonus counties (urban counties with low traditional Medicare spending and historically high Medicare Advantage enrollment).

How are Medicare Advantage plans evaluated?
Medicare uses information from member satisfaction surveys, plans, and health care providers to give overall performance star ratings to plans. A plan can get a rating between 1 and 5 stars. A 5-star rating is considered excellent. These ratings help you compare plans based on quality and performance.
What is CMS star rating based on?
The Centers for Medicare & Medicaid Services (CMS) uses a five-star quality rating system to measure the experiences Medicare beneficiaries have with their health plan and health care system — the Star Rating Program. Health plans are rated on a scale of 1 to 5 stars, with 5 being the highest.
How are CMS stars calculated?
For the Overall Star Rating, Z-scores were produced by subtracting the national mean score from each hospital's measure score and dividing that by the standard deviation across hospitals. Standard deviation is a number that measures how far data values are from their average.
Which Medicare Advantage plan has the highest rating?
What Does a Five Star Medicare Advantage Plan Mean? Medicare Advantage plans are rated from 1 to 5 stars, with five stars being an “excellent” rating. This means a five-star plan has the highest overall score for how well it offers members access to healthcare and a positive customer service experience.
How are star ratings determined?
Summary star ratings are an average of a provider's question level star ratings. Patient star ratings are calculated by dividing the patient's aggregate mean score by 20. For clients using only one question in the patient star rating, the star rating would simply be the individual question score, divided by 20.
What is star quality rating?
The star quality rating indicates the quality or confidence in the results of the study producing the CMF. While the reviewers applied an objective as possible set of criteria, the star quality rating still results from an exercise in judgment and a degree of subjectivity.
What are the CMS quality measures?
These goals include: effective, safe, efficient, patient-centered, equitable, and timely care.
What does a CMS 5 Star rating mean?
Nursing homes with 5 stars are considered to have much above average quality and nursing homes with 1 star are considered to have quality much below average.
What is the 5 star rating system?
The Five-Star Quality Rating System is a tool to help consumers select and compare skilled nursing care centers. Created by the Centers for Medicare & Medicaid Services (CMS) in 2008, the rating system uses information from Health Care Surveys (both standard and complaint), Quality Measures, and Staffing.
What is the biggest disadvantage of Medicare Advantage?
The takeaway There are some disadvantages as well, including provider limitations, additional costs, and lack of coverage while traveling. Whether you choose original Medicare or Medicare Advantage, it's important to review healthcare needs and Medicare options before choosing your coverage.
What are the top 3 most popular Medicare supplement plans in 2021?
Three plans — Plan F, Plan G, and Plan N — are the most popular (accounting for over 80 percent of all plans sold). Here's an in-depth look at this trio of Medicare Supplement plans, and the reasons so many people choose them.
What are 4 types of Medicare Advantage plans?
Below are the most common types of Medicare Advantage Plans.Health Maintenance Organization (HMO) Plans.Preferred Provider Organization (PPO) Plans.Private Fee-for-Service (PFFS) Plans.Special Needs Plans (SNPs)
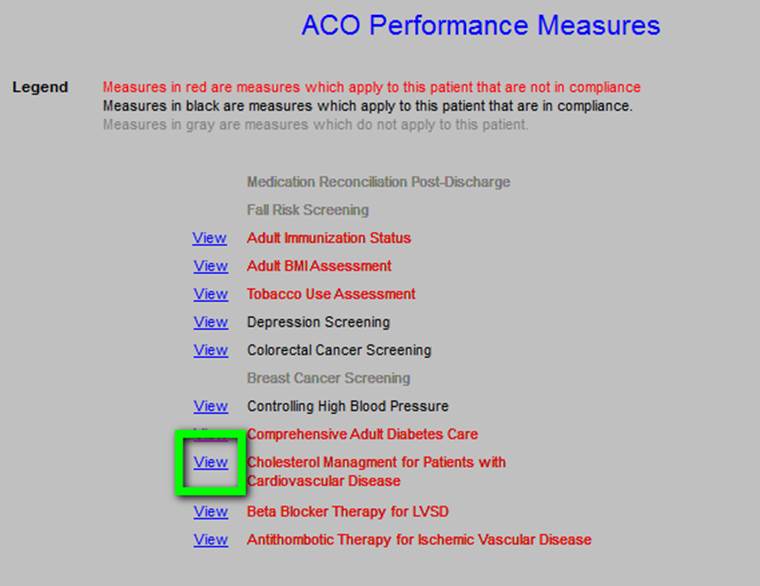
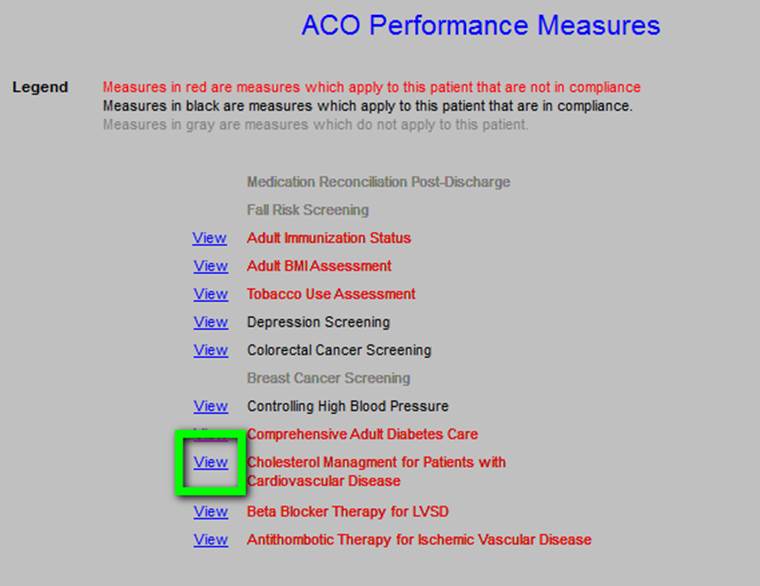
Measures, domains for star ratings
CMS assesses a Medicare Advantage plan’s quality of care according to the plan’s performance on a list of quality measures. Each measure falls under one of nine domains. The domains include maintaining health, chronic disease management, member experience, member complaints, and customer service as well as four domains for scoring drug plans.
Categorical adjustment index
The fact that stars are assigned to contracts and not individual plans could pose a problem for contracts that cover a diverse set of Medicare Advantage health plans.
Adjustments for stable, high performance
Additionally, CMS has incorporated an improvement measure for plans that receive high scores multiple years in a row. Consistently high-scoring plans would receive a lower star score in successive years because they have less room for improvement.
Quality bonus payments
As a result of the data collection and calculations involved in this methodology, the Medicare Advantage Star Rating system helps consumers compare Medicare Advantage plans. It also informs CMS how much to reimburse payers with Medicare Advantage contracts.
What is a quality rating?
Quality ratings are assigned at the contract level, rather than for each individual plan, meaning that each plan covered under the same contract receives the same quality rating. Most contracts cover multiple plans, and can include individual plans, as well as employer-sponsored and special needs plans (SNPs).
Why do Medicare Advantage plans get stars?
Medicare Advantage plans receive a star rating based on performance measures that are intended to help potential enrollees compare plans available in their area as well as encourage plans to compete based on quality. All plans that are part of a single Medicare Advantage contract are combined when calculating the quality rating ...
How much is the bonus for Medicare 2021?
UnitedHealthcare and Humana, which together account for 46% of Medicare Advantage enrollment, have bonus payments of $5.3 billion (46% of total bonus payments) in 2021. BCBS affiliates (including Anthem BCBS) and CVS Health each have $1.6 billion in bonus spending, followed by Kaiser Permanente ($1.1 billion), Cigna and Centene ($0.2 billion each).
What percentage of Medicare Advantage plans will receive bonus payments in 2021?
In 2021, 81 percent of all Medicare Advantage enrollees are in plans that receive a bonus payment from Medicare based on star quality ratings (or because they are new), substantially higher than the share in 2015 (55 percent). Annual bonus payments from the federal government to Medicare Advantage insurers have increased correspondingly, ...
How much is Medicare Advantage rebate in 2021?
Additionally, as more enrollees are in plans that are in bonus status, the average rebate per Medicare Advantage enrollee has more than doubled, rising from $184 per year in 2015 to $446 per year in 2021.
How much is the average bonus for 2021?
The average bonus per enrollee in an employer plan is $886 in 2021, more than 2.5 times higher than for enrollees in either individual plans ($351) or SNPs ($309). While average bonuses in employer plans have consistently been higher than for other plans, the gap has increased substantially in recent years, driven by a rapid rise in the average bonuses for employer plans. Both the high share of enrollees in group plans that receive bonus payments (98% in 2021), as well as changes to the payment methodology for group plans implemented starting in 2017 contribute to this trend.
What is Medicare Advantage 2021?
Medicare Advantage in 2021: Star Ratings and Bonuses. Medicare Advantage plans receive a star rating based on performance measures that are intended to help potential enrollees compare plans available in their area as well as encourage plans to compete based on quality. All plans that are part of a single Medicare Advantage contract are combined ...
Measures, Domains For Star Ratings
Categorical Adjustment Index
- READ MORE: Surveys, Advanced Analytics Key for Member Experience, Star Ratings The fact that stars are assigned to contracts and not individual plans could pose a problem for contracts that cover a diverse set of Medicare Advantage health plans. For example, one employer-sponsored Medicare Advantage plan in a contract could serve a healthier demographic with lower social de…
Adjustments For Stable, High Performance
- Additionally, CMS has incorporated an improvement measure for plans that receive high scores multiple years in a row. Consistently high-scoring plans would receive a lower star score in successive years because they have less room for improvement. Calculating the improvement measure involves assessing the net improvement for process measures, patient experience an…
Quality Bonus Payments
- As a result of the data collection and calculations involved in this methodology, the Medicare Advantage Star Rating system helps consumers compare Medicare Advantage plans. It also informs CMS how much to reimburse payers with Medicare Advantage contracts. The additional quality bonus payment for high-performing health plans is directly linked to ...