Full Answer
How long does it take to enroll in Medicare?
Medicare typically completes enrollment applications in 60 – 90 days. This varies widely by intermediary (by state). We see some applications turnaround in 15 days and others take as long as 3 months. Medicare will set the effective date as the date they receive the application.
How do I enroll in the Medicare fee-for-service provider program?
MDPP suppliers must use Form CMS-20134 to enroll in the Medicare Program. If you don’t see your provider type listed, contact your MAC’s provider enrollment center before submitting a Medicare enrollment application. For your state’s MAC contact information, refer to the Medicare Fee-For-Service Provider Enrollment Contact List.
How do I become a Medicare participating provider or supplier?
To participate as a Medicare Program provider or supplier, submit the Medicare Participating Physician or Supplier Agreement (Form CMS-460) upon initial enrollment. You’ve 90 days after your initial enrollment approval letter is sent to decide if you want to be a participating provider or supplier.
What is the Code of federal regulations for physician credentialing?
Credentialing of Providers is required under the Social Security Act, Section 1852. See also, Code of Federal Regulations-42 CFR 422.204, and the Medicare Managed Care Manual, Chapter 6. This presentation focuses mostly on Physician Credentialing by Medicare Advantage Organizations (MAO).
What does it mean to be credentialed with Medicare?
Credentialing is the process of approving a physician, agency or other medical provider as part of the Medicare supply chain.
How long does Medicare enrollment take Australia?
We'll process your application. It may take up to 6 weeks to process your application if you apply between July and November. This is because we get a lot of applications at that time. We'll write to you if we don't approve your application or need more information.
What is a Medicare entity?
According to the Centers for Medicare and Medicaid Services (CMS), a provider entity is a health care provider or supplier who bills Medicare or Medicaid for services rendered and has a National Provider Identifier (NPI) number.
Which of the following are steps to becoming a Medicare provider?
Applying to become a Medicare providerStep 1: Obtain an NPI. Psychologists seeking to become Medicare providers must obtain a National Provider Identifier (NPI) before attempting to enroll in Medicare. ... Step 2: Complete the Medicare Enrollment Application. ... Step 3: Select a Specialty Designation.
How long does Medicare Enrolment take?
Most Medicare provider number applications are taking up to 9 calendar days to process from the date we get your application. Some applications may take longer if they need to be assessed by the Department of Health. We assess your application to see if you're eligible to access Medicare benefits.
How long does a Medicare claim take?
Using the Medicare online account When you submit a claim online, you'll usually get your benefit within 7 days.
What is a qualified entity?
More Definitions of Qualified entity Qualified entity means a business or organization that provides care to children or the elderly or disabled, whether governmental, private, for profit, nonprofit or voluntary, except organizations exempt pursuant to subdivision A 10 of § 63.2-1715.
What is a first tier entity Medicare?
The term first tier entity means any party that enters into a written arrangement with an MA organization or contract applicant to provide administrative services or health care services for a Medicare eligible individual.
What is an entity provider?
Entity providers supply mapping services between representations and their associated Java types. There are two types of entity providers: MessageBodyReader and MessageBodyWriter . For HTTP requests, the MessageBodyReader is used to map an HTTP request entity body to method parameters.
Does Medicare require board certification?
Perhaps more convincingly, the CMS does not require board certification for provider enrollment in the Medicare program, which covers over 55 million elderly, disabled, and otherwise vulnerable Americans.
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
Why do I need Medicare Part C?
Medicare Part C provides more coverage for everyday healthcare including prescription drug coverage with some plans when combined with Part D. A Medicare Advantage prescription drug (MAPD) plan is when a Part C and Part D plan are combined. Medicare Part D only covers prescription drugs.
How long does it take to get a credential?
Most major carriers can complete the process in 90 – 120 days. Smaller regional or local plans may take even longer.
How long does it take for Medicare to process an application?
Medicare typically completes enrollment applications in 60 – 90 days. This varies widely by intermediary (by state). We see some applications turnaround in 15 days and others take as long as 3 months. Medicare will set the effective date as the date they receive the application.
How does a carrier credentialing work?
First is credentialing where the carrier verifies your credentials and presents your credentialing application to their committee for approval. After you are approved by the carrier’s credentialing committee, you then complete the contracting process to become a participating provider and receive an effective date.
What is the phone number for Medicare to replace a 147C?
Click here for an example of a CP575 To request a replacement letter 147C, you can call the IRS business center at (800) 829-4933. The hours of operation are 7:00 a.m. – 7:00 p.m. local time, Monday through Friday.
How long does it take for Medicare to bill?
Medicare will set the effective date as the date they receive the application. So, even if it takes 3 months for them to complete an application, you will be able to retroactively bill Medicare for services from the date your application was received.
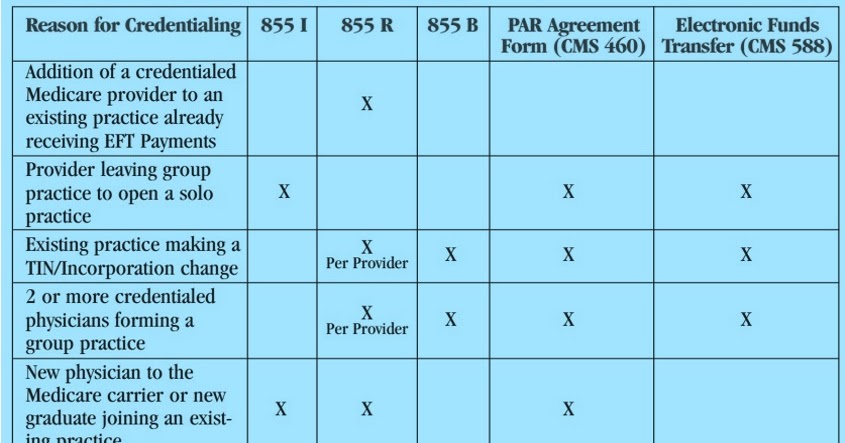
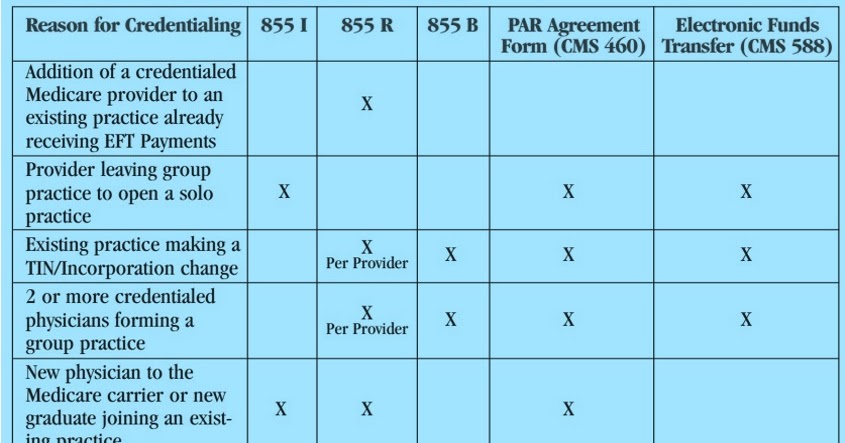
What is a CMS 855I?
The CMS 855I is used for individual provider enrollment in the Medicare plan. The 855I can be used by physician and non-physician providers. Supporting documents and details required by the application vary by provider types.
What is AO in Medicare?
Section 1865 (a) (1) of the Social Security Act (the Act) permits providers and suppliers "accredited" by an approved national accreditation organization (AO) to be exempt from routine surveys by State survey agencies to determine compliance with Medicare conditions.
Is AO required for Medicare?
Accreditation by an AO is voluntary and is not required for Medicare certification or participation in the Medicare Program. A provider’s or supplier’s ability to bill Medicare for covered services is not impacted if it chooses to discontinue accreditation from a CMS-approved AO or change AOs.
Provider Credentialing for Medicare and Medicaid
Provider credentialing is the process of gathering and verifying a doctor’s credentials. Credentialing ensures that providers have the required licenses, certifications, and skills to care for patients properly.
What is Provider Enrollment?
Provider enrollment is the process of enrolling a provider with commercial or government health insurance plans to which the provider can be reimbursed for the services rendered to patients.
Critical Steps for Credentialing a Provider
Make a list and collect all information you need for provider credentialing applications like professional licenses, work history, certifications, bank statements, and more.
How long does it take to become a Medicare provider?
You’ve 90 days after your initial enrollment approval letter is sent to decide if you want to be a participating provider or supplier.
How to change Medicare enrollment after getting an NPI?
Before applying, be sure you have the necessary enrollment information. Complete the actions using PECOS or the paper enrollment form.
How to get an NPI for Medicare?
Step 1: Get a National Provider Identifier (NPI) You must get an NPI before enrolling in the Medicare Program. Apply for an NPI in 1 of 3 ways: Online Application: Get an I&A System user account. Then apply in the National Plan and Provider Enumeration System (NPPES) for an NPI.
How to request hardship exception for Medicare?
You may request a hardship exception when submitting your Medicare enrollment application via either PECOS or CMS paper form. You must submit a written request with supporting documentation with your enrollment that describes the hardship and justifies an exception instead of paying the application fee.
What is Medicare Part B?
Medicare Part B claims use the term “ordering/certifying provider” (previously “ordering/referring provider”) to identify the professional who orders or certifies an item or service reported in a claim. The following are technically correct terms:
What is Medicare revocation?
A Medicare-imposed revocation of Medicare billing privileges. A suspension, termination, or revocation of a license to provide health care by a state licensing authority or the Medicaid Program. A conviction of a federal or state felony within the 10 years preceding enrollment, revalidation, or re-enrollment.
How much is the Medicare application fee for 2021?
Application Fee Amount. The enrollment application fee sent January 1, 2021, through December 31, 2021, is $599. For more information, refer to the Medicare Application Fee webpage. How to Pay the Application Fee ⤵. Whether you apply for Medicare enrollment online or use the paper application, you must pay the application fee online:
What is incident to rule in Medicare?
Using the Medicare rule of incident-to rule; this provides an exception and permits reporting of services performed by personnel under the name of a credentialed physician, if requirements are met. This rule is most commonly used to report the services of NPPs under the name of a licensed and credentialed physician. 1.
Do you have to go through credentialing boards before getting approved?
However most carriers have credentialing boards or committees that the application will need to go before to receive final approval before being made active. This may affect how quickly the carrier is able to process the newest application depending on their schedule for meeting and the volume they have to review.
Is NPP credentialing carrier dependent?
In 2018 we saw a increase in the requirements needed for credentialing NPP, but as noted this is carrier dependent.
How long can a locum tenens be on Medicare?
Medicare beneficiaries must seek to receive services from the regular physician, and services may not be provided by the locum tenens over a continuous period of more than 60 days (with the exception of a locum tenens filling in for a physician who is a member of the armed forces called to active duty).
Do locum tenens have to be enrolled in Medicare?
The locum tenens physician does not have to be enrolled in the Medicare program or be in the same specialty as the physician for whom he or she is filling in, but the locum tenens must have a National Provider Identifier (NPI) and possess an unrestricted license in the state in which he or she is practicing.