How many chiropractor visits are paid by Medicare per year?
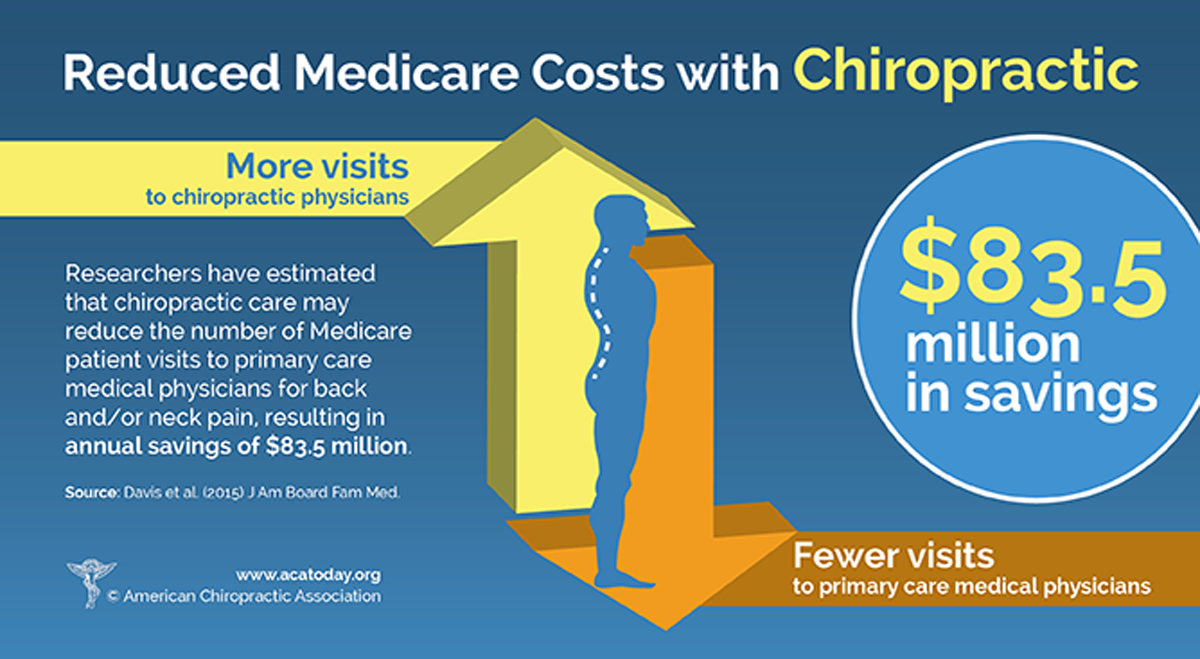
Chiropractic services. Medicare Part B (Medical Insurance) covers manual manipulation of the spine by a chiropractor or other qualified provider if. medically necessary. to correct a. subluxation. (when one or more of the bones of your spine move out of position). Medicare doesn't cover other services or tests a chiropractor orders, including X-rays, massage therapy, …
How much does Aflac pay for chiropractic visits?
Dec 24, 2021 · To date, there isnt a limit to the number of chiropractic visits Medicare allows. Youre able to receive treatment as long as its necessary to treat or correct your condition.
How many physical therapy visits are covered by Medicare?
Dec 27, 2021 · Medicare covers only a very limited selection of chiropractic services, of which are covered by Part B. As Part B is the part of Medicare that covers outpatient medical services, it makes sense that this coverage would apply to chiropractors. However, chiropractic services don’t qualify as medical care in the ordinary sense, so Part B won’t cover chiropractic services …
What are the Medicare guidelines for chiropractic?
If Medicare does pay for your treatment, it will cover 80% of the cost, while you will owe the remaining 20%. Medigap insurance may cover this remaining portion. Medicare Part B covers only Chiropractic care for subluxation, but if you have a Medicare Advantage Plan (Medicare Part C), your plan may cover a broader range of chiropractic services.
How long should you wait between chiropractic visits?
Common Chiropractic Treatment Plans In general, in the absence of progressive worsening of a condition during chiropractic care, a common chiropractic program is 3 times per week for 2 to 4 weeks, followed by a re-evaluation.
Does Medicare pay for a chiropractic exam?
Medicare covers chiropractic visits for medically necessary manual manipulation of the spine. “Medically necessary” means that the treatment is needed to diagnose or treat an illness, injury, condition or disease – or the related symptoms – and that it meets accepted standards of medicine.
How many adjustments do you need chiropractor?
Common Chiropractic Adjustment Frequencies To achieve maximum benefits, most injury and pain types will need somewhere between four and twelve sessions. Ongoing maintenance is used to prevent pain from coming back and to prevent additional injuries from forming due to a misalignment of the spine.Jun 1, 2020
Does Medicare cover spinal decompression?
Medicare covers chiropractic manipulation of the spine to help a person manage back pain, provided they have active back pain. The program only funds chiropractic care that corrects an existing problem and does not cover spinal manipulations as maintenance or preventive services.Mar 3, 2020
Does Medicare pay for massages?
Original Medicare (parts A and B) doesn't cover massage therapy, but it can cover other therapies like physical therapy and acupuncture. If you use massage therapy without Medicare coverage, you'll be responsible for 100 percent of the costs. Medicare Advantage (Part C) may offer some coverage for massage therapy.Oct 2, 2020
Is it necessary to go to a chiropractor 3 times a week?
Depending on the severity of the underlying condition which is causing your pain, it is typical for a patient to need chiropractic care or adjustments 2-3 times per week for 4-12 weeks.
Why do chiropractors want you to keep coming back?
Changing your posture, changing your spine's ability to move, changing your muscle health and structure take time. Months in fact. All muscles have memory and your body wants to go back to its old patterns instead of creating new healthy ones. That is why adjustments need to be repeated again and again.Jun 20, 2021
How often should you have your neck adjusted?
If your main priority of getting chiropractic adjustments is to maintain a healthy body, you should visit your chiropractor several times a month. You might benefit from getting adjustments as often as every week.
What should a treatment plan include?
A treatment plan should include a recommendation for the duration and frequency of visits. Also, the program should consist of specific treatment goals, objective measures to evaluate treatment effectiveness, and the date of initial treatment.
Who is Lindsay Malzone?
Lindsay Malzone is the Medicare expert for MedicareFAQ. She has been working in the Medicare industry since 2017. She is featured in many publications as well as writes regularly for other expert columns regarding Medicare.
Does Medicare pay for massage therapy?
A participating provider will bill Medicare and charge you only for the amount Medicare doesn’t pay. A non-participating provider must bill Medicare but may ask you to pay the bill, and you’ll get a reimbursement. Does Medicare cover massage therapy? Your chiropractor may advise massage therapy to help ease the pain.
Do you need a referral for chiropractic care?
For the most part, if you have Medicare, you won’t need a referral. But, with an Advantage plan, a referral could be a requirement. How many chiropractic visits does Medicare allow? For Chiropractic care, there is no cap on the number of visits Medicare will cover to correct a subluxation.
Does Medicare cover Medigap?
Now, on services Medicare does cover, Medigap can help eliminate some or all of the deductibles and coinsurances. Our agents can help you learn more about the benefits of Medigap, give us a call at the number above. Or, fill out an online rate form to discover your rates now!
Does Medicare cover chiropractors?
Medicare doesn’t cover a visit to the chiropractor for other reasons. If you see a chiropractor for spine manipulation, you should be aware that Medicare won’t pay for it. For example, Medicare won’t cover x-rays or acupuncture with a chiropractor’s orders. But, you’ll have coverage for the actual chiropractic treatment ...
What is subluxation in chiropractic?
Subluxation is a condition where one or more of the bones of your spine are out of position.
What is medically necessary?
Under Medicare Part B, medically necessary has a very particular meaning: “health care services and supplies needed to diagnose to treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine.”.
Does Medicare cover chiropractic?
Medicare will only cover the actual chiropractic treatments, not any X-rays, massage therapy, and acupuncture recommended by your chiropractor. Medicare will only cover a limited number of treatments, which may be less than your doctor and/or chiropractor recommend.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
What is subluxation of the spine?
Subluxation of the spine is when the vertebra – the bones in the spine – are separated or out of position. Symptoms may include pain, headache or stiffness, though these may have other causes as well. Chiropractic treatment involves adjusting the spine manually (with the hands) to help realign the vertebra and relieve the symptoms.
Does Medicare cover chiropractors?
Medicare covers a chiropractor specifically for manual manipulation of the spine to correct a subluxation. Original Medicare (Parts A & B) does not cover other services or tests ordered by a chiropractor, such as X-rays, massage therapy or acupuncture. Some Medicare Advantage plans (Part C) may provide additional chiropractic coverage.