As long as the employer has more than 20 employees, then the coverage is considered creditable under Medicare. You’ll get a Special Enrollment Period when you drop employer coverage. This allows you to enroll in Part B without being penalized for not doing so when you were first eligible.
Full Answer
How many people are enrolled in Medicare?
Although Medicare eligibility has nothing to do with income levels, it can provide healthcare both for Americans with disabilities as well as people age 65 or older. About 19 million people enrolled when Medicare first started. By 2020, that number grew to nearly 63 million.
What is the number of employees for this employer for Medicare Secondary?
· CMS Fast Facts. CMS has developed a new quick reference statistical summary on annual CMS program and financial data. CMS Fast Facts includes summary information on total program enrollment, utilization, expenditures, as well as total number of Medicare providers including physicians by specialty area. The download below will be updated as data ...
How many employees do you need to have to qualify for Medicare?
Medicare Employer: 20+ employees: Employer: Medicare : Disabled job-based insurance: Fewer than 100 employees: Medicare: Employer: 100+ employees: Employer: Medicare : Liability …
How many Medicare Advantage enrollees are offered by employers and unions?
Number of People Receiving Medicare (2019): *. Total Medicare beneficiaries. • Aged. • Disabled. 61.2 million. • 52.6 million. • 8.7 million. Part A (Hospital Insurance, HI) beneficiaries. • Aged.
How many people are in Medicare system?
Medicare beneficiaries In 2020, 62.6 million people were enrolled in the Medicare program, which equates to 18.4 percent of all people in the United States. Around 54 million of them were beneficiaries for reasons of age, while the rest were beneficiaries due to various disabilities.
How big is the Medicare industry?
Historical NHE, 2020: NHE grew 9.7% to $4.1 trillion in 2020, or $12,530 per person, and accounted for 19.7% of Gross Domestic Product (GDP). Medicare spending grew 3.5% to $829.5 billion in 2020, or 20 percent of total NHE.
Who controls Medicare?
the Centers for Medicare & Medicaid ServicesMedicare is a federal program. It is basically the same everywhere in the United States and is run by the Centers for Medicare & Medicaid Services, an agency of the federal government.
How much does Medicare cost the government?
Medicare accounts for a significant portion of federal spending. In fiscal year 2020, the Medicare program cost $776 billion — about 12 percent of total federal government spending.
What percentage of the US population is on Medicare?
18.4%Medicare is a federal health insurance program that pays for covered health care services for most people aged 65 and older and for certain permanently disabled individuals under the age of 65. An estimated 60 million individuals (18.4% of the U.S. population) were enrolled in Medicare in 2020.
Is healthcare the largest industry in the US?
Healthcare takes more than 10% of the GDP of most developed countries. In fact, for the US this figure will be close to 18% by the end of 2019. This isn't surprising—the healthcare sector is the US's largest employer. Incidentally, the US spends considerably more than the world's average on healthcare.
Is Medicare funded by Social Security?
Medicare is funded by the Social Security Administration. Which means it's funded by taxpayers: We all pay 1.45% of our earnings into FICA - Federal Insurance Contributions Act, if you're into deciphering acronyms - which go toward Medicare.
Is Medicare federally funded?
As a federal program, Medicare relies on the federal government for nearly all of its funding. Medicaid is a joint state and federal program that provides health care coverage to beneficiaries with very low incomes.
How does Medicare get funded?
Funding for Medicare comes primarily from general revenues, payroll tax revenues, and premiums paid by beneficiaries (Figure 1). Other sources include taxes on Social Security benefits, payments from states, and interest.
Is Medicare underfunded?
Politicians promised you benefits, but never funded them.
Does Medicare lose money?
Medicare is not going bankrupt. It will have money to pay for health care. Instead, it is projected to become insolvent. Insolvency means that Medicare may not have the funds to pay 100% of its expenses.
Why does Medicare cost so much?
Medicare Part B covers doctor visits, and other outpatient services, such as lab tests and diagnostic screenings. CMS officials gave three reasons for the historically high premium increase: Rising prices to deliver health care to Medicare enrollees and increased use of the health care system.
How many people in Texas have Medicare?
Nonetheless, nearly 16% of its massive population of 39.5 million has Medicare, totaling about 6.3 million individuals. With Texas as the second most populous U.S. state, as of 2019, roughly 14% of Texas’ population has Medicare. By comparison, the state of Maine has over 25% of its population on Medicare.
Which states have the highest Medicare enrollment?
Overall, California, Florida and Texas have the highest number of people enrolled in Medicare. They are the only three states whose Medicare members exceed four million. Of course, California holding the title of most populous state translates to a higher Medicare population.
How to find Medicare population by state?
In order to see a complete list of Medicare populations by state, visit the website of the Centers for Medicare and Medicaid Services (CMS).
What is Medicare Supplement?
Medicare Supplement (Medigap) – Supplements help pay expenses for hospital and medical services left by Original Medicare, with each Medigap plan standardized to cover specific expenses like deductibles, co-pays, and co-insurance.
What is Medicare count?
Counting Medicare enrollees per year and per month. Generally meant by the term Medicare health plan are Medicare-approved health insurance products that works in addition to having Original Medicare. As a means of getting benefits that can exceed Medicare, you can choose from Medicare health plans: Medicare Advantage (Part C) ...
What is Medicare health plan?
As often as monthly, the Centers for Medicare and Medicaid Services keep tabs on trends in the Medicare population by: Generally meant by the term Medicare health plan are Medicare-approved health insurance products that works in addition to having Original Medicare.
How many Medicare Advantage subscribers are there in 2019?
Whereas in 2014, Medicare Advantage had about 16.2 million subscribers, by 2019 that number rose to nearly 23 million . As a whole, Medicare appears to be growing as the competition for benefits progresses.
What is the difference between Medicare and Medicaid?
Eligible for Medicare. Medicare. Medicaid ( payer of last resort) 1 Liability insurance only pays on liability-related medical claims. 2 VA benefits and Medicare do not work together. Medicare does not pay for any care provided at a VA facility, and VA benefits typically do not work outside VA facilities.
Is Medicare a secondary insurance?
When you have Medicare and another type of insurance, Medicare is either your primary or secondary insurer. Use the table below to learn how Medicare coordinates with other insurances. Go Back. Type of Insurance. Conditions.
How much is Medicare Part A deductible?
– Initial deductible: $1,408.
What is Medicare Advantage?
Medicare Advantage (MA): Eligibility to choose a MA plan: People who are enrolled in both Medicare A and B, pay the Part B monthly premium, do not have end-stage renal disease, and live in the service area of the plan. Formerly known as Medicare+Choice or Medicare Health Plans.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
What is a Medicare company?
The company that acts on behalf of Medicare to collect and manage information on other types of insurance or coverage that a person with Medicare may have, and determine whether the coverage pays before or after Medicare. This company also acts on behalf of Medicare to obtain repayment when Medicare makes a conditional payment, and the other payer is determined to be primary.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
Which insurance pays first, Medicare or No Fault?
No-fault insurance or liability insurance pays first and Medicare pays second.
Which pays first, Medicare or group health insurance?
If you have group health plan coverage through an employer who has 20 or more employees, the group health plan pays first, and Medicare pays second.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
How many employees are eligible for Medicare?
When an employer participates in a multi-employer/multiple employer plan and at least one participating employer has at least 20 full and/or part-time employees, the Working Aged MSP rules apply to all individuals entitled to Medicare on the basis of age, including those associated with the employer having fewer than 20 employees.
When did Medicare become secondary?
Medicare would be the primary payer for the first 19 calendar weeks of 2009. Starting week 20 of 2009, Medicare would become secondary and remain secondary for the remainder of 2009.
When did Medicare become the primary payer for GHP?
Since there is no “20 week rule” for employers that get smaller, Medicare will not become the primary payer over GHP coverage until January 1, 2010.
Which payer would be the secondary payer to GHP coverage during all of the calendar year 2007?
Medicare would be the secondary payer to GHP coverage during all of the calendar year 2007 because there were 20 or more employees during the preceding year, 2006.
Can a GHP be a small employer?
However, the law provides that a multi-employer GHP (or its authorized insurer) may be granted a Small Employer Exception (SEE) to the Working Aged provisions for specifically identified employees and specifically identified spouses entitled to Medicare on the basis of age and who are covered as a named insured or spouse (covered individual) of an employer with fewer than 20 full and/or part-time employees.
Does Medicare apply to a single employer?
If an employer, having fewer than 20 full and/or part-time employees, sponsors or contributes to a single-employer GHP, the MSP rules applicable to individuals entitled to Medicare on the basis of age do not apply to such individuals. Medicare is the primary payer.
Is Medicare a GHP?
Medicare is the secondary payer to GHPs for the working aged where either a single employer of 20 or more full and/or part-time employees is the sponsor of the GHP or contributor to the GHP, or two or more employers are sponsors or contributors to a multi-employer/multiple employer plan, and a least one of the employers has 20 or more full and/or part -time employees.
Who can provide information for Medicare?
Vendors, especially those involved in administering health plans and HSAs, can also provide helpful information for Medicare-eligible employees.
How long does it take to get Medicare?
Generally, individuals can enroll in Medicare within a seven-month window around the time they turn age 65. There are several parts to Medicare, with varying premiums, that employees should keep in mind:
How long is the Cobra enrollment period?
Employees should beware that if after ending employment they elect to use COBRA for their insurance for more than eight months (and COBRA coverage is generally available for up to 18 months), then the penalties for missing the special enrollment period and enrolling late are significant and, in the form of higher premiums, continuous.
How long does an employer's plan remain primary?
At firms with 20 or more employees, "emphasize that the employer's plan will generally remain primary as long as the employee is actively employed ," Buckey said. "That means employees—and their providers—should continue to submit claims first to the employer's plan and then to Medicare, as appropriate. Remind employees to alert their providers to this secondary coverage."
Do you have to have Medicare if you have fewer than 20 employees?
If they work for an employer with fewer than 20 employees, they will need to enroll in Medicare to have primary insurance, because health care coverage from employers with fewer than 20 employees pays secondary to Medicare. Failing to enroll will trigger higher-premium penalties.
How much does Part B premium go up?
For instance, "If employees lack employer coverage and don't sign up for Part B when they're first eligible, their monthly premium for Part B may go up 10 percent for each full 12-month period that they delayed enrollment," said Kim Buckey, vice president of client services at Burlington, Mass.-based DirectPath, a benefits education, enrollment and health care transparency firm.
What age can you take Medicare?
Centers for Medicare & Medicaid Services (CMS) can provide such information as how income from employment may impact Medicare premiums and specific actions Medicare-eligible employees may take when they reach age 65 . YOU'VE READ 3 of 3 FREE ARTICLES THIS MONTH.
How many counties are covered by Medicare?
In 117 counties, accounting for 5 percent of the Medicare population, more than 60% of all Medicare beneficiaries are enrolled in Medicare Advantage plans or cost plans. Many of these counties are centered around large, urban areas, such as Monroe County, NY (69%), which includes Rochester, and Allegheny County, PA (63%), which includes Pittsburgh.
What are the companies that are part of Medicare Advantage?
Medicare Advantage enrollment is highly concentrated among a small number of firms. UnitedHealthcare and Humana together account for 44 percent of all Medicare Advantage enrollees nationwide, and the BCBS affiliates (including Anthem BCBS plans) account for another 15 percent of enrollment in 2020. Another four firms (CVS Health, Kaiser Permanente, Centene, and Cigna) account for another 23 percent of enrollment in 2020. For the fourth year in a row, enrollment in UnitedHealthcare’s plans grew more than any other firm, increasing by more than 500,000 beneficiaries between March 2019 and March 2020. This is also the first year that Humana’s increase in plan year enrollment was close to UnitedHealthcare’s, with an increase of about 494,000 beneficiaries between March 2019 and March 2020. CVS Health purchased Aetna in 2018 and had the third largest growth in Medicare Advantage enrollment in 2020, increasing by about 396,000 beneficiaries between March 2019 and March 2020.
How many Medicare Advantage enrollees are in a plan that requires higher cost sharing than the Part A hospital
Nearly two-thirds (64%) of Medicare Advantage enrollees are in a plan that requires higher cost sharing than the Part A hospital deductible in traditional Medicare for a 7-day inpatient stay, and more than 7 in 10 (72%) are in a plan that requires higher cost sharing for a 10-day inpatient stay.
How much is the deductible for Medicare Advantage 2020?
In contrast, under traditional Medicare, when beneficiaries require an inpatient hospital stay, there is a deductible of $1,408 in 2020 (for one spell of illness) with no copayments until day 60 of an inpatient stay.
Which cities have low Medicare enrollment?
Some urban areas, such as Baltimore City (20%) and Cook County, IL (Chicago, 28%) have low Medicare Advantage enrollment, compared to the national average (39%). 4. Most Medicare Advantage enrollees are in plans operated by UnitedHealthcare, Humana, or BlueCross BlueShield (BCBS) affiliates in 2020.
What percentage of Medicare beneficiaries are in Miami-Dade County?
Within states, Medicare Advantage penetration varies widely across counties. For example, in Florida, 71 percent of all beneficiaries living in Miami-Dade County are enrolled in Medicare Advantage plans compared to only 14 percent of beneficiaries living in Monroe County (Key West).
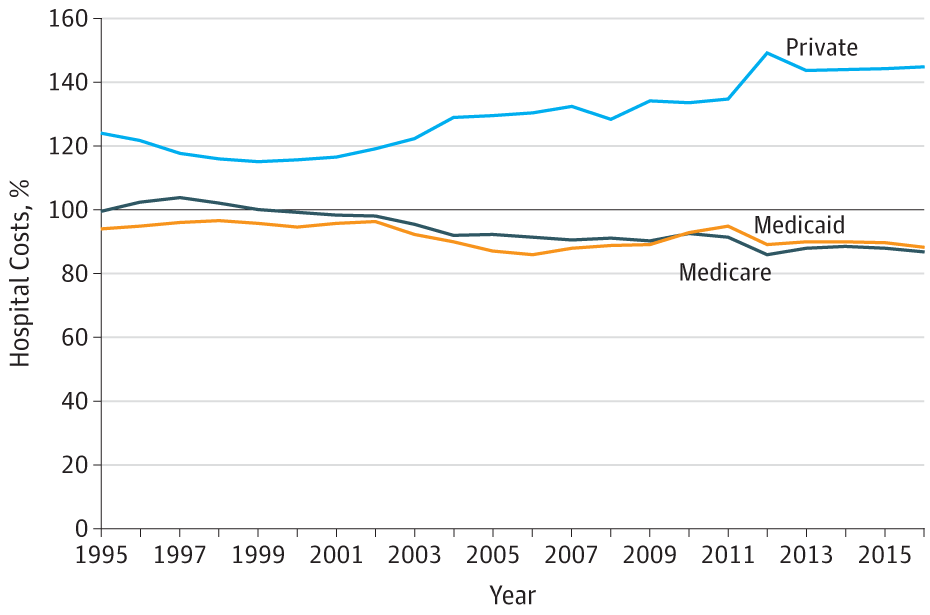
Does Medicare Advantage have lower FFS?
Hospitals in states with higher shares of Medicare Advantage enrollees may have lower FFS reimbursement overall. As a result, some hospitals and other health care entities may be reimbursed less that they would if the allocation of funds took into account payments received on behalf of Medicare Advantage enrollees. 3.
How many employees can you have with Medicare?
There are two sets of compliance, one for employers with less than 20 employees and one for those over 20 employees. Not understanding the difference could be very expensive for both the employee and the employer.
Who can subsidize Medicare Part B?
The Employer or the Agent? The liability came down on the employer . In companies with less than 20 employees, the employer can subsidize the cost of an employee’s Medicare Part B and Medicare subsidy. This has always proven to be less expensive than the insurance companies individual group health rate.
Who was misinformed by the group health insurance agent?
The employer had been misinformed by the group health insurance agent who was not aware of the Medicare Part B requirement for companies with less than 20 employees. The liability of these expenses became a topic for the lawyers. Was the employee responsible for the uncovered expenses? The Employer or the Agent? The liability came down on the employer.
Is group health insurance less expensive than individual health insurance?
This has always proven to be less expensive than the insurance companies individual group health rate. However, when the employer pays a significant portion of the employee’s individual health insurance premium, the employee usually elects to remain on the company’s policy.