What hours is Medicare open for calls?
1-800-MEDICARE (1-800-633-4227) is the official Medicare phone number that beneficiaries may call for help with their coverage, claims, payments and more. You may call 24 hours a day, 7 days per week, and help is available in both English and Spanish as well as for the hearing impaired (the TTY Medicare toll-free line is 1-877-486-2048).
Does Medicare call you at home?
You can relax because you were correct not to give your personal information over the phone due to the fact that Medicare or even Social Security does not randomly call your home or office and ask for your personal information. Medicare already has all of the information they need about you. Medicare or Social Security will never call you!
When does the 100 day Medicare period restart?
You must be released from the hospital to a facility or Medicaid will not pay. There must be 60 days between hospital cases for the 100 days to reset. A limited amount of days left for Medicare to pay and the facility anticipates the patient stay being longer than the dollars allow.
What is the phone number to contact Medicare?
What is the Medicare Phone Number?
- “Claim service” or press “1”
- “Coverage and benefits” or press “2”
- “Premium payments” or press “3”
- “Preventive exams” or press “4”
- “Deductible” or press “5”
- “Help me with something else” or press “6”
- “Agent” or press “0” (zero)
What is the 21 day rule for Medicare?
For days 21–100, Medicare pays all but a daily coinsurance for covered services. You pay a daily coinsurance. For days beyond 100, Medicare pays nothing. You pay the full cost for covered services.
How many days does Medicare pay for?
Medicare covers up to 100 days of care in a skilled nursing facility (SNF) each benefit period. If you need more than 100 days of SNF care in a benefit period, you will need to pay out of pocket. If your care is ending because you are running out of days, the facility is not required to provide written notice.
Can you call Medicare 24 hours a day?
Medicare.gov Live Chat is available 24 hours a day, 7 days a week, except some federal holidays.
Do Medicare days reset?
Does Medicare Run on a Calendar Year? Yes, Medicare's deductible resets every calendar year on January 1st. There's a possibility your Part A and/or Part B deductible will increase each year. The government determines if Medicare deductibles will either rise or stay the same annually.
What is the 3 day rule for Medicare?
The 3-day rule requires the patient have a medically necessary 3-consecutive-day inpatient hospital stay. The 3-consecutive-day count doesn't include the discharge day or pre-admission time spent in the Emergency Room (ER) or outpatient observation.
Does Medicare pay 100 of hospital bills?
According to the Centers for Medicare and Medicaid Services (CMS), more than 60 million people are covered by Medicare. Although Medicare covers most medically necessary inpatient and outpatient health expenses, Medicare reimbursement sometimes does not pay 100% of your medical costs.
How can I reach Medicare by phone?
(800) 633-4227Centers for Medicare & Medicaid Services / Customer service
What is the best way to contact Medicare?
1-800-MEDICARE (1-800-633-4227) For specific billing questions and questions about your claims, medical records, or expenses, log into your secure Medicare account, or call us at 1-800-MEDICARE.
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
Can you run out of Medicare?
In general, there's no upper dollar limit on Medicare benefits. As long as you're using medical services that Medicare covers—and provided that they're medically necessary—you can continue to use as many as you need, regardless of how much they cost, in any given year or over the rest of your lifetime.
How long can you stay in hospital with Medicare?
90 daysMedicare covers a hospital stay of up to 90 days, though a person may still need to pay coinsurance during this time. While Medicare does help fund longer stays, it may take the extra time from an individual's reserve days. Medicare provides 60 lifetime reserve days.
How many lifetime reserve days does Medicare cover?
60 daysOriginal Medicare covers up to 90 days of inpatient hospital care each benefit period. You also have an additional 60 days of coverage, called lifetime reserve days. These 60 days can be used only once, and you will pay a coinsurance for each one ($778 per day in 2022).
Will Medicare cover skilled nursing care?
Medicare will pay for what’s considered intermittent nursing services, meaning that care is provided either fewer than seven days a week, or daily...
Will Medicare cover physical, occupational, and speech therapy?
Medicare will pay for physical therapy when it’s required to help patients regain movement or strength following an injury or illness. Similarly, i...
Does Medicare cover durable medical equipment?
Medicare will cover the cost of medically necessary equipment prescribed by a doctor for in-home use. This includes items such as canes or walkers,...
Does Medicare cover medical social services?
Medicare will pay for medically prescribed services that allow patients to cope with the emotional aftermath of an injury or illness. These may inc...
Who’s eligible for in-home care through Medicare?
Medicare enrollees are eligible for in-home care under Medicare Parts A and B provided the following conditions are met: The patient is under the c...
Will Medicaid pay for long-term care services?
Many Medicare enrollees are qualify for Medicaid due to their limited incomes and assets. Unlike Medicare, Medicaid covers both nursing home care a...
How many hours a week does Medicare cover home health?
Medicare’s home health benefit covers skilled nursing care and home health aide services provided up to seven days per week for no more than eight hours per day and 28 hours per week. If you need additional care, Medicare provides up to 35 hours per week on a case-by-case basis.
How often do you have to recertify your home health plan?
You can continue to receive home health care for as long as you qualify. However, your plan of care must be recertified every 60 days by your doctor. Your doctor may make changes to the hours you are receiving or other services, depending on whether the level of care you are receiving is still reasonable and necessary.
What is a medical social service?
Medical social services. Part-time or intermittent home health aide services (personal hands-on care) Injectible osteoporosis drugs for women. Usually, a home health care agency coordinates the services your doctor orders for you. Medicare doesn't pay for: 24-hour-a-day care at home. Meals delivered to your home.
What is the eligibility for a maintenance therapist?
To be eligible, either: 1) your condition must be expected to improve in a reasonable and generally predictable period of time, or 2) you need a skilled therapist to safely and effectively make a maintenance program for your condition , or 3) you need a skilled therapist to safely and effectively do maintenance therapy for your condition. ...
What is intermittent skilled nursing?
Intermittent skilled nursing care (other than drawing blood) Physical therapy, speech-language pathology, or continued occupational therapy services. These services are covered only when the services are specific, safe and an effective treatment for your condition.
Does Medicare cover home health services?
Your Medicare home health services benefits aren't changing and your access to home health services shouldn’t be delayed by the pre-claim review process.
Can you get home health care if you attend daycare?
You can still get home health care if you attend adult day care. Home health services may also include medical supplies for use at home, durable medical equipment, or injectable osteoporosis drugs.
How many hours does Medicare pay for a week?
The maximum amount of weekly care Medicare will pay for is usually 28 hours, though in some circumstances, it will pay for up to 35. But it won’t cover 24-hour-a-day care.
How long does Medicare pay for intermittent nursing?
Medicare will pay for what’s considered intermittent nursing services, meaning that care is provided either fewer than seven days a week, or daily for less than eight hours a day, for up to 21 days. Sometimes, Medicare will extend this window if a doctor can provide a precise estimate on when that care will end.
How long does Medicare pay for custodial care?
Medicare will sometimes pay for short-term custodial care (100 days or less) if it’s needed in conjunction with actual in-home medical care prescribed by a doctor.
What is a long term care policy?
A long-term care policy can help defray the cost of home health aides whose services are strictly custodial in nature. It can also help pay for assisted living facilities, which offer seniors the ability to live independently, albeit with help.
Does Medicare cover social services?
Does Medicare cover medical social services? Medicare will pay for medically prescribed services that allow patients to cope with the emotional aftermath of an injury or illness. These may include in-home counseling from a licensed therapist or social worker.
Does Medicaid have a higher income limit?
Due to the high cost of long-term care, many states have higher Medicaid income limits for long-term care benefits than for other Medicaid coverage. However, Medicaid’s asset limits usually require you to “spend-down” resources before becoming eligible.
Is skilled nursing part time?
The need for skilled nursing is only part-time or intermittent. The home health agency used to provide care is approved by Medicare. Additionally, other than durable medical care, patients usually don’t pay anything for in-home care.
How long does Medicare cover hospital care?
Depending on how long your inpatient stay lasts, there is a limit to how long Medicare Part A will cover your hospital costs. For the first 60 days of ...
How many reserve days do you get with Medicare?
Medicare limits you to only 60 of these days to use over the course of your lifetime, and they require a coinsurance payment of $742 per day in 2021. You only get 60 lifetime reserve days, and they do not reset after a benefit period or a calendar year.
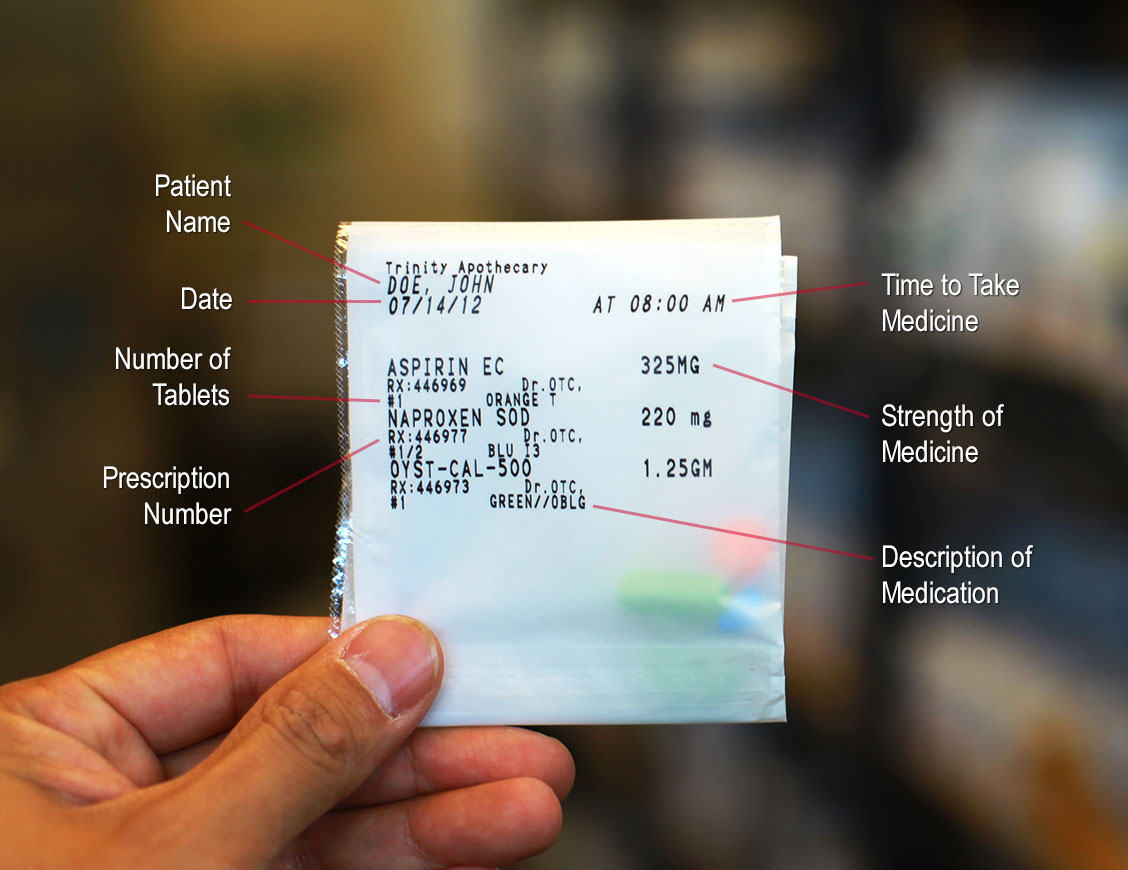
What is the Medicare donut hole?
Medicare Part D prescription drug plans feature a temporary coverage gap, or “ donut hole .”. During the Part D donut hole, your drug plan limits how much it will pay for your prescription drug costs. Once you and your plan combine to spend $4,130 on covered drugs in 2021, you will enter the donut hole. Once you enter the donut hole in 2021, you ...
How much is Medicare Part A deductible in 2021?
You are responsible for paying your Part A deductible, however. In 2021, the Medicare Part A deductible is $1,484 per benefit period. During days 61-90, you must pay a $371 per day coinsurance cost (in 2021) after you meet your Part A deductible.
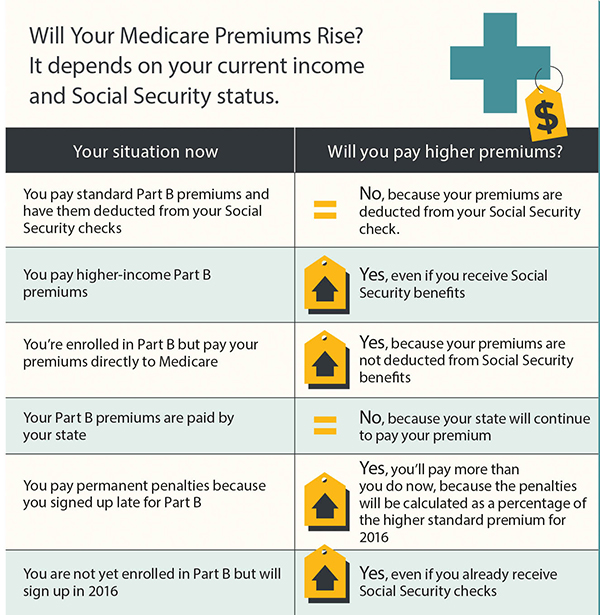
What is Medicare Part B and Part D?
Medicare Part B (medical insurance) and Part D have income limits that can affect how much you pay for your monthly Part B and/or Part D premium. Higher income earners pay an additional amount, called an IRMAA, or the Income-Related Monthly Adjusted Amount.
What is Medicare Advantage Plan?
When you enroll in a Medicare Advantage plan, it replaces your Original Medicare coverage and offers the same benefits that you get from Medicare Part A and Part B.
What is the Medicare Advantage spending limit?
Medicare Advantage (Medicare Part C) plans, however, do feature an annual out-of-pocket spending limit for covered Medicare expenses. While each Medicare Advantage plan carrier is free to set their own out-of-pocket spending limit, by law it must be no greater than $7,550 in 2021. Some plans may set lower maximum out-of-pocket (MOOP) limits.
How many hours of DSMT is covered by Medicare?
Medicare may cover up to 10 hours of initial DSMT – 1 hour of individual training and 9 hours of group training.
What is original Medicare?
Your costs in Original Medicare. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference.
How does hospital status affect Medicare?
Inpatient or outpatient hospital status affects your costs. Your hospital status—whether you're an inpatient or an outpatient—affects how much you pay for hospital services (like X-rays, drugs, and lab tests ). Your hospital status may also affect whether Medicare will cover care you get in a skilled nursing facility ...
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. , coinsurance. An amount you may be required to pay as your share of the cost for services after you pay any deductibles.
How long does an inpatient stay in the hospital?
Inpatient after your admission. Your inpatient hospital stay and all related outpatient services provided during the 3 days before your admission date. Your doctor services. You come to the ED with chest pain, and the hospital keeps you for 2 nights.
Does Medicare cover skilled nursing?
Your hospital status may also affect whether Medicare will cover care you get in a skilled nursing facility (SNF) following your hospital stay. You're an inpatient starting when you're formally admitted to the hospital with a doctor's order. The day before you're discharged is your last inpatient day. You're an outpatient if you're getting ...
How long do you have to live to qualify for Medicare?
You qualify for full Medicare benefits if: You are a U.S. citizen or a permanent legal resident who has lived in the United States for at least five years and. You are receiving Social Security or railroad retirement benefits or have worked long enough to be eligible for those benefits but are not yet collecting them.
How old do you have to be to get Medicare?
citizen or have been a legal resident for at least five years, you can get full Medicare benefits at age 65 or older. You just have to buy into them by: Paying premiums for Part A, the hospital insurance.
How much will Medicare premiums be in 2021?
If you have 30 to 39 credits, you pay less — $259 a month in 2021. If you continue working until you gain 40 credits, you will no longer pay these premiums. Paying the same monthly premiums for Part B, which covers doctor visits and other outpatient services, as other enrollees pay.
How long do you have to be on disability to receive Social Security?
You have been entitled to Social Security disability benefits for at least 24 months (that need not be consecutive); or. You receive a disability pension from the Railroad Retirement Board and meet certain conditions; or.
Medicare Covers Medically Necessary Home Health Services
Medicare does not usually cover the cost of non-medical home care aides if that is the only type of assistance that a senior needs.
Medicare Advantage May Offer More Comprehensive Coverage
Private insurance companies run Medicare Advantage. Those companies are regulated by Medicare and must provide the same basic level of coverage as Original Medicare. However, they also offer additional coverage known as “supplemental health care benefits.”
note
Medicare law no longer limits how much it pays for your medically necessary outpatient therapy services in one calendar year.
note
To find out how much your test, item, or service will cost, talk to your doctor or health care provider. The specific amount you’ll owe may depend on several things, like:
note
Your doctor or other health care provider may recommend you get services more often than Medicare covers. Or, they may recommend services that Medicare doesn’t cover. If this happens, you may have to pay some or all of the costs. Ask questions so you understand why your doctor is recommending certain services and whether Medicare will pay for them.