How many people in the United States have Medicare?
In 2020, 62.6 million people were enrolled in the Medicare program, which equates to 18.4 percent of all people in the United States. Around 54 million of them were beneficiaries for reasons of age, while the rest were beneficiaries due to various disabilities.
What is a Medicare payment amount?
In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference.
Do you have to pay monthly for Medicare?
Generally, you pay a monthly premium for Medicare coverage and part of the costs each time you get a covered service. There’s no yearly limit on what you pay out-of-pocket, unless you have supplemental coverage, like a Medicare Supplement Insurance (
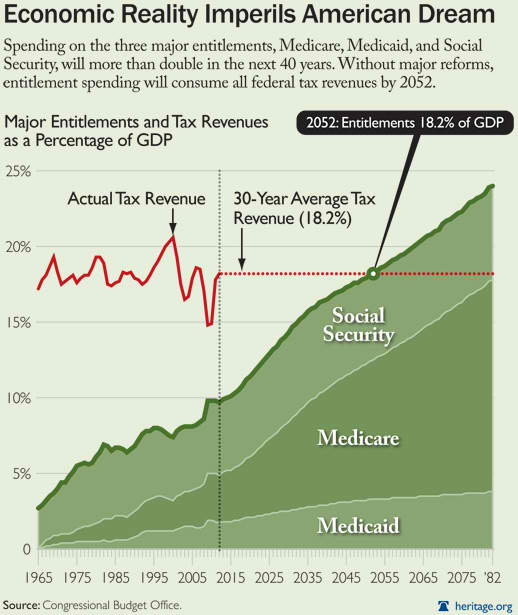
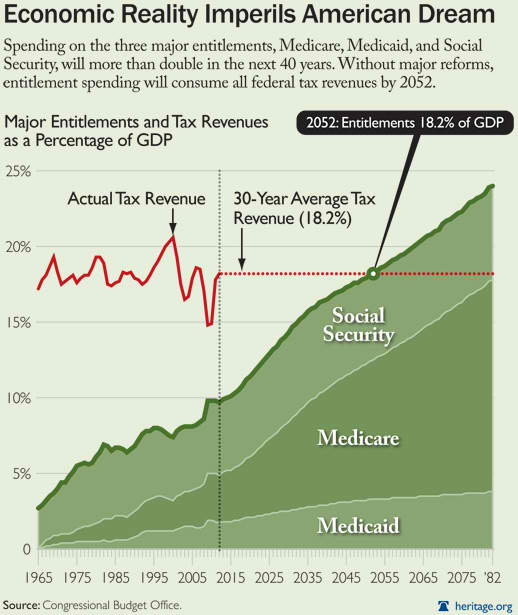
How much of the federal budget is spent on Medicare?
In 2018, Medicare spending (net of income from premiums and other offsetting receipts) totaled $605 billion, accounting for 15 percent of the federal budget (Figure 1). In 2018, Medicare benefit payments totaled $731 billion, up from $462 billion in 2008 (Figure 2) (these amounts do not net out premiums and other offsetting receipts).
How Much Does Medicare pay out each year?
In 2018, Medicare benefit payments totaled $731 billion, up from $462 billion in 2008.
How often are Medicare premiums paid?
All Medicare bills are due on the 25th of the month. In most cases, your premium is due the same month that you get the bill. Example of our billing timeline. For your payment to be on time, we must get your payment by the due date on your bill.
How much are Medicare premiums for 2021?
$148.50 forThe standard monthly premium for Medicare Part B enrollees will be $148.50 for 2021, an increase of $3.90 from $144.60 in 2020. The annual deductible for all Medicare Part B beneficiaries is $203 in 2021, an increase of $5 from the annual deductible of $198 in 2020.
Are Medicare premiums paid monthly or quarterly?
BILL TYPE Some people with Medicare are billed either monthly or quarterly. If you are billed for Part A or IRMAA Part D, you will be billed monthly. If this box says: • FIRST BILL, it means your last payment was received timely or this is your initial bill. SECOND BILL, it means a payment is late by at least 60 days.
What is the Medicare Part B premium for 2021?
$148.50Medicare Part B Premium and Deductible The standard monthly premium for Medicare Part B enrollees will be $170.10 for 2022, an increase of $21.60 from $148.50 in 2021. The annual deductible for all Medicare Part B beneficiaries is $233 in 2022, an increase of $30 from the annual deductible of $203 in 2021.
How much does Social Security take out for Medicare each month?
In 2021, based on the average social security benefit of $1,514, a beneficiary paid around 9.8 percent of their income for the Part B premium. Next year, that figure will increase to 10.6 percent.
What is the Medicare Part B premium for 2022?
$170.102022. The standard Part B premium amount in 2022 is $170.10. Most people pay the standard Part B premium amount.
Is Medicare Part A free at age 65?
You are eligible for premium-free Part A if you are age 65 or older and you or your spouse worked and paid Medicare taxes for at least 10 years. You can get Part A at age 65 without having to pay premiums if: You are receiving retirement benefits from Social Security or the Railroad Retirement Board.
Is Medicare premium based on income?
Medicare premiums are based on your modified adjusted gross income, or MAGI. That's your total adjusted gross income plus tax-exempt interest, as gleaned from the most recent tax data Social Security has from the IRS.
Does Medicare come out of your Social Security check?
Medicare Part B (medical insurance) premiums are normally deducted from any Social Security or RRB benefits you receive. Your Part B premiums will be automatically deducted from your total benefit check in this case. You'll typically pay the standard Part B premium, which is $170.10 in 2022.
How is Medicare paid?
How is Medicare financed? Funding for Medicare comes primarily from general revenues, payroll tax revenues, and premiums paid by beneficiaries (Figure 1). Other sources include taxes on Social Security benefits, payments from states, and interest.
Can I pay Medicare Part B monthly instead of quarterly?
Part B: If you receive retirement benefits from Social Security, the Railroad Retirement Board or the civil service, your Part B premiums are automatically deducted from your monthly payments—there's no other option. But if you don't get any of those benefits, Medicare will send quarterly bills.
What is Medicare in the US?
Matej Mikulic. Medicare is a federal social insurance program and was introduced in 1965. Its aim is to provide health insurance to older and disabled people. In 2018, 17.8 percent of all people in the United States were covered by Medicare.
How many people are on Medicare in 2019?
In 2019, over 61 million people were enrolled in the Medicare program. Nearly 53 million of them were beneficiaries for reasons of age, while the rest were beneficiaries due to various disabilities.
Which state has the most Medicare beneficiaries?
With over 6.1 million, California was the state with the highest number of Medicare beneficiaries . The United States spent nearly 800 billion U.S. dollars on the Medicare program in 2019. Since Medicare is divided into several parts, Medicare Part A and Part B combined were responsible for the largest share of spending.
What is Medicare inpatient?
Hospital inpatient services – as included in Part A - are the service type which makes up the largest single part of total Medicare spending. Medicare, however, has also significant income, which amounted also to some 800 billion U.S. dollars in 2019.
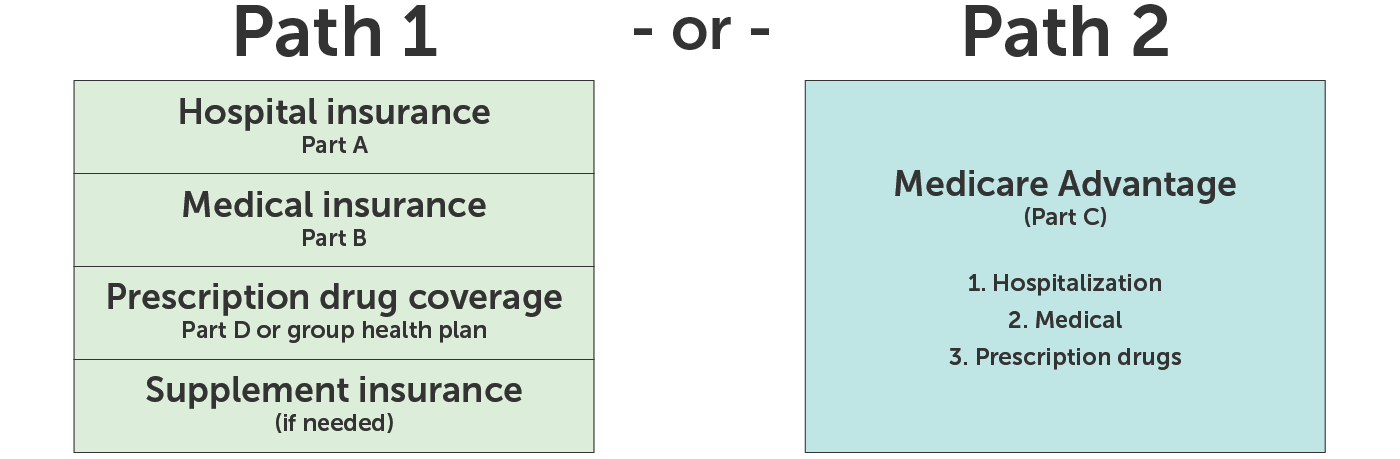
Medicare Advantage Plan (Part C)
Monthly premiums vary based on which plan you join. The amount can change each year.
Medicare Supplement Insurance (Medigap)
Monthly premiums vary based on which policy you buy, where you live, and other factors. The amount can change each year.
How much does Medicare pay for outpatient therapy?
After your deductible is met, you typically pay 20% of the Medicare-approved amount for most doctor services (including most doctor services while you're a hospital inpatient), outpatient therapy, and Durable Medical Equipment (DME) Part C premium. The Part C monthly Premium varies by plan.
What happens if you don't buy Medicare?
If you don't buy it when you're first eligible, your monthly premium may go up 10%. (You'll have to pay the higher premium for twice the number of years you could have had Part A, but didn't sign up.) Part A costs if you have Original Medicare. Note.
What is Medicare Advantage Plan?
A Medicare Advantage Plan (Part C) (like an HMO or PPO) or another Medicare health plan that offers Medicare prescription drug coverage. Creditable prescription drug coverage. In general, you'll have to pay this penalty for as long as you have a Medicare drug plan.
How much is coinsurance for days 91 and beyond?
Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime). Beyond Lifetime reserve days : All costs. Note. You pay for private-duty nursing, a television, or a phone in your room.
How much is coinsurance for 61-90?
Days 61-90: $371 coinsurance per day of each benefit period. Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime) Beyond lifetime reserve days: all costs. Part B premium.
Do you pay more for outpatient services in a hospital?
For services that can also be provided in a doctor’s office, you may pay more for outpatient services you get in a hospital than you’ll pay for the same care in a doctor’s office . However, the hospital outpatient Copayment for the service is capped at the inpatient deductible amount.
Does Medicare cover room and board?
Medicare doesn't cover room and board when you get hospice care in your home or another facility where you live (like a nursing home). $1,484 Deductible for each Benefit period . Days 1–60: $0 Coinsurance for each benefit period. Days 61–90: $371 coinsurance per day of each benefit period.
How much does Medicare pay for therapy?
Starting in 2019, Medicare no longer limits how much it will pay for medically necessary therapy services. You will typically pay 20% of the Medicare-approved amount for your therapy services, once you have met your Part B deductible for the year.
What is Medicare Part A?
Medicare Part A (Hospital Insurance) and Part B (Medical Insurance) cover inpatient hospital and outpatient health care services that are deemed medically necessary. " Medically necessary " can be defined as “services and supplies that are needed to prevent, diagnose, or treat illness, injury, disease, health conditions, ...
How long does Medicare cover psychiatric care?
Medicare only covers 190 days of inpatient care in a psychiatric hospital throughout your lifetime. If you require more than the Medicare-approved stay length at a psychiatric hospital, there’s no lifetime limit for mental health treatment you receive as an inpatient at a general hospital.
What is a Medigap policy?
Medicare Supplement Insurance (Medigap) policies are private health care plans designed to supplement your Original Medicare benefits and help pay for some of the out-of-pocket costs that Original Medicare doesn’t cover.
How long can you stay in a hospital with Medicare?
Medicare Part A covers hospital stays for any single illness or injury up to a benefit period of 90 days. If you need to stay in the hospital more than 90 days, you have the option of using your lifetime reserve days, of which the Medicare lifetime limit is 60 days.
What are the services that are beyond the annual limit?
Extended hospitalization. Psychiatric hospital stays. Skilled nursing facility care. Therapy services. If you require any of these services beyond the annual limits, and don't qualify for an exception, you may be responsible for the full cost of those services for the rest of the year.
Does Medicare cover hospital costs?
Medicare covers many of your hospital and medical care costs, but it doesn't cover 100% of them . Here's what you can do to help bridge the gaps left by Medicare limits and offset some of your healthcare costs.
How much did Medicare spend?
Medicare spending increased 6.4% to $750.2 billion, which is 21% of the total national health expenditure. The rise in Medicaid spending was 3% to $597.4 billion, which equates to 16% of total national health expenditure.
What is the agency that administers Medicare?
To grasp the magnitude of the government expenditure for Medicare benefits, following are 2018 statistics from the Centers for Medicare & Medicaid Services (CMS), which is the agency that administers Medicare:
What is the largest share of health spending?
The biggest share of total health spending was sponsored by the federal government (28.3%) and households (28.4%) while state and local governments accounted for 16.5%. For 2018 to 2027, the average yearly spending growth in Medicare (7.4%) is projected to exceed that of Medicaid and private health insurance.
Does Medicare pay payroll taxes?
Additionally, Medicare recipients have seen their share of payroll taxes for Medicare deducted from their paychecks throughout their working years.
How long does Medicare cover hospital care?
Depending on how long your inpatient stay lasts, there is a limit to how long Medicare Part A will cover your hospital costs. For the first 60 days of ...
How many reserve days do you get with Medicare?
Medicare limits you to only 60 of these days to use over the course of your lifetime, and they require a coinsurance payment of $742 per day in 2021. You only get 60 lifetime reserve days, and they do not reset after a benefit period or a calendar year.
What is the Medicare donut hole?
Medicare Part D prescription drug plans feature a temporary coverage gap, or “ donut hole .”. During the Part D donut hole, your drug plan limits how much it will pay for your prescription drug costs. Once you and your plan combine to spend $4,130 on covered drugs in 2021, you will enter the donut hole. Once you enter the donut hole in 2021, you ...
How much is Medicare Part A deductible in 2021?
You are responsible for paying your Part A deductible, however. In 2021, the Medicare Part A deductible is $1,484 per benefit period. During days 61-90, you must pay a $371 per day coinsurance cost (in 2021) after you meet your Part A deductible.
What happens if you spend $6,550 out of pocket in 2021?
After you spend $6,550 out-of-pocket on covered drugs in 2021, you leave the donut hole coverage gap and enter the catastrophic coverage stage. Once you reach this stage, you only pay a small coinsurance or copayment for your covered drugs for the rest of the year.
What is Medicare Part B and Part D?
Medicare Part B (medical insurance) and Part D have income limits that can affect how much you pay for your monthly Part B and/or Part D premium. Higher income earners pay an additional amount, called an IRMAA, or the Income-Related Monthly Adjusted Amount.
What is Medicare Advantage Plan?
When you enroll in a Medicare Advantage plan, it replaces your Original Medicare coverage and offers the same benefits that you get from Medicare Part A and Part B.
What is Medicare benefit period?
Medicare benefit periods mostly pertain to Part A , which is the part of original Medicare that covers hospital and skilled nursing facility care. Medicare defines benefit periods to help you identify your portion of the costs. This amount is based on the length of your stay.
What facilities does Medicare Part A cover?
Some of the facilities that Medicare Part A benefits apply to include: hospital. acute care or inpatient rehabilitation facility. skilled nursing facility. hospice. If you have Medicare Advantage (Part C) instead of original Medicare, your benefit periods may differ from those in Medicare Part A.
How much coinsurance do you pay for inpatient care?
Days 1 through 60. For the first 60 days that you’re an inpatient, you’ll pay $0 coinsurance during this benefit period. Days 61 through 90. During this period, you’ll pay a $371 daily coinsurance cost for your care. Day 91 and up. After 90 days, you’ll start to use your lifetime reserve days.
How long does Medicare benefit last after discharge?
Then, when you haven’t been in the hospital or a skilled nursing facility for at least 60 days after being discharged, the benefit period ends. Keep reading to learn more about Medicare benefit periods and how they affect the amount you’ll pay for inpatient care. Share on Pinterest.
How much is Medicare deductible for 2021?
Here’s what you’ll pay in 2021: Initial deductible. Your deductible during each benefit period is $1,484. After you pay this amount, Medicare starts covering the costs. Days 1 through 60.
How long does Medicare Advantage last?
Takeaway. Medicare benefit periods usually involve Part A (hospital care). A period begins with an inpatient stay and ends after you’ve been out of the facility for at least 60 days.
How long can you be out of an inpatient facility?
When you’ve been out of an inpatient facility for at least 60 days , you’ll start a new benefit period. An unlimited number of benefit periods can occur within a year and within your lifetime. Medicare Advantage policies have different rules entirely for their benefit periods and costs.
How many types of Medicare savings programs are there?
Medicare savings programs. There are four types of Medicare savings programs, which are discussed in more detail in the following sections. As of November 9, 2020, Medicare has not announced the new income and resource thresholds to qualify for the following Medicare savings programs.
What is Medicare Part B?
Medicare Part B. This is medical insurance and covers visits to doctors and specialists, as well as ambulance rides, vaccines, medical supplies, and other necessities.
What is the Medicare Part D premium for 2021?
Part D plans have their own separate premiums. The national base beneficiary premium amount for Medicare Part D in 2021 is $33.06, but costs vary. Your Part D Premium will depend on the plan you choose.
How much is Medicare Part B 2021?
For Part B coverage, you’ll pay a premium each year. Most people will pay the standard premium amount. In 2021, the standard premium is $148.50. However, if you make more than the preset income limits, you’ll pay more for your premium.
How does Social Security determine IRMAA?
The Social Security Administration (SSA) determines your IRMAA based on the gross income on your tax return. Medicare uses your tax return from 2 years ago. For example, when you apply for Medicare coverage for 2021, the IRS will provide Medicare with your income from your 2019 tax return. You may pay more depending on your income.
Does Medicare change if you make a higher income?
If you make a higher income, you’ll pay more for your premiums, even though your Medicare benefits won’t change.
Can I qualify for QI if I have medicaid?
You can’t qualify for the QI program if you have Medicaid. If you have a monthly income of less than $1,456 or a joint monthly income of less than $1,960, you are eligible to apply for the QI program. You’ll need to have less than $7,860 in resources. Married couples need to have less than $11,800 in resources.
Summary
- Medicare, the federal health insurance program for nearly 60 million people ages 65 and over and younger people with permanent disabilities, helps to pay for hospital and physician visits, prescription drugs, and other acute and post-acute care services. This issue brief includes the m…
Health
- In 2017, Medicare spending accounted for 15 percent of the federal budget (Figure 1). Medicare plays a major role in the health care system, accounting for 20 percent of total national health spending in 2016, 29 percent of spending on retail sales of prescription drugs, 25 percent of spending on hospital care, and 23 percent of spending on physician services.
Causes
- Slower growth in Medicare spending in recent years can be attributed in part to policy changes adopted as part of the Affordable Care Act (ACA) and the Budget Control Act of 2011 (BCA). The ACA included reductions in Medicare payments to plans and providers, increased revenues, and introduced delivery system reforms that aimed to improve efficiency and quality of patient care …
Effects
- In addition, although Medicare enrollment has been growing around 3 percent annually with the aging of the baby boom generation, the influx of younger, healthier beneficiaries has contributed to lower per capita spending and a slower rate of growth in overall program spending. In general, Part A trust fund solvency is also affected by the level of growth in the economy, which affects …
Impact
- Prior to 2010, per enrollee spending growth rates were comparable for Medicare and private health insurance. With the recent slowdown in the growth of Medicare spending and the recent expansion of private health insurance through the ACA, however, the difference in growth rates between Medicare and private health insurance spending per enrollee has widened.
Future
- While Medicare spending is expected to continue to grow more slowly in the future compared to long-term historical trends, Medicares actuaries project that future spending growth will increase at a faster rate than in recent years, in part due to growing enrollment in Medicare related to the aging of the population, increased use of services and intensity of care, and rising health care pri…
Funding
- Medicare is funded primarily from general revenues (41 percent), payroll taxes (37 percent), and beneficiary premiums (14 percent) (Figure 7). Part B and Part D do not have financing challenges similar to Part A, because both are funded by beneficiary premiums and general revenues that are set annually to match expected outlays. Expected future increases in spending under Part B and …
Assessment
- Medicares financial condition can be assessed in different ways, including comparing various measures of Medicare spendingoverall or per capitato other spending measures, such as Medicare spending as a share of the federal budget or as a share of GDP, as discussed above, and estimating the solvency of the Medicare Hospital Insurance (Part A) trust fund.
Purpose
- The solvency of the Medicare Hospital Insurance trust fund, out of which Part A benefits are paid, is one way of measuring Medicares financial status, though because it only focuses on the status of Part A, it does not present a complete picture of total program spending. The solvency of Medicare in this context is measured by the level of assets in the Part A trust fund. In years whe…
Benefits
- A number of changes to Medicare have been proposed that could help to address the health care spending challenges posed by the aging of the population, including: restructuring Medicare benefits and cost sharing; further increasing Medicare premiums for beneficiaries with relatively high incomes; raising the Medicare eligibility age; and shifting Medicare from a defined benefit s…