The expansion group covers 15 million people as of June 2019, about 12 million of whom were newly eligible for Medicaid under the ACA (the remainder had been covered under Section 1115 waivers and subsequently moved to expansion group).
How many Americans have gained coverage through the ACA’s Medicaid expansion?
52 rows · Jun 05, 2021 · The data shows those individuals currently enrolled in health coverage through the Health Insurance Marketplaces and Medicaid expansion under the ACA, including 11.3 million people enrolled in the ACA Marketplace plans as of February 2021 and 14.8 million newly-eligible people enrolled in Medicaid through the ACA’s expansion of eligibility to adults …
How many people are currently enrolled in the Affordable Care Act?
Oct 14, 2021 · Affordable Care Act Medicaid Expansion. Medicaid—a federal/state partnership with shared authority and financing—is a health insurance program for low-income individuals, …
Is Medicaid enrollment expansion happening in the expansion States?
Jun 09, 2021 · The ACA Medicaid expansion has significantly increased Medicaid enrollment and federal Medicaid expenditures. In FY2018, an estimated 12.2 million individuals were newly …
How many people are newly enrolled in Medicaid?
But the COVID pandemic drove the enrollment numbers significantly higher: As of 2021, there were about 14.8 million Medicaid enrollees who had gained eligibility due to Medicaid …
What is Medicaid expansion?
A provision in the Affordable Care Act (ACA) called for the expansion of Medicaid eligibility in order to cover more low-income Americans. Under th...
Why are there some states that haven't implemented Medicaid expansion?
The ACA called for Medicaid expansion nationwide. But in June 2012, the Supreme Court ruled that states could not be forced to expand their Medicai...
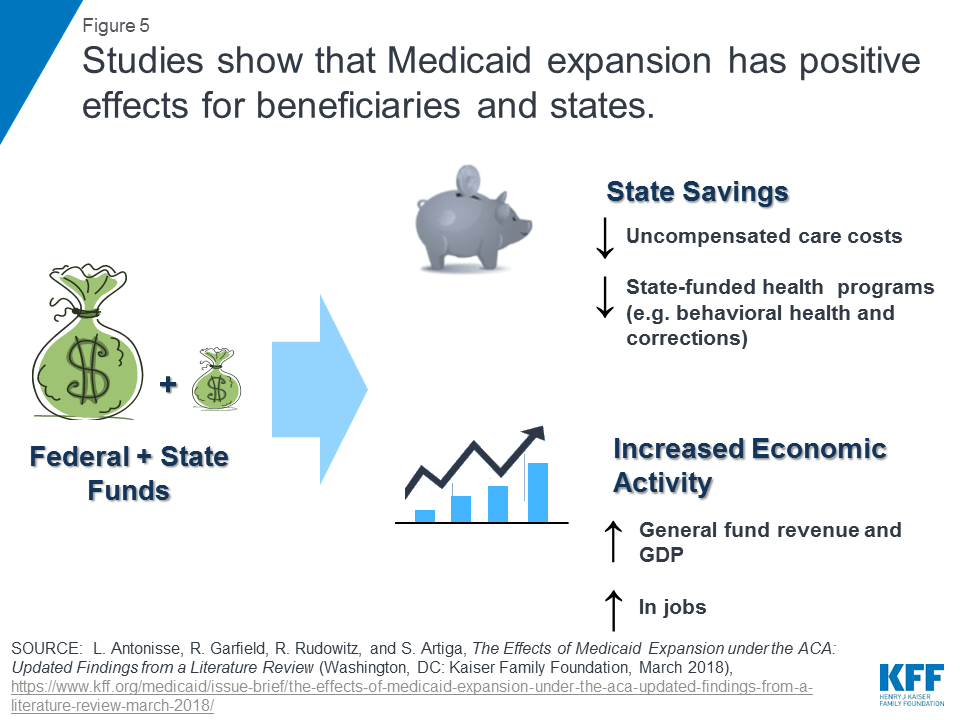
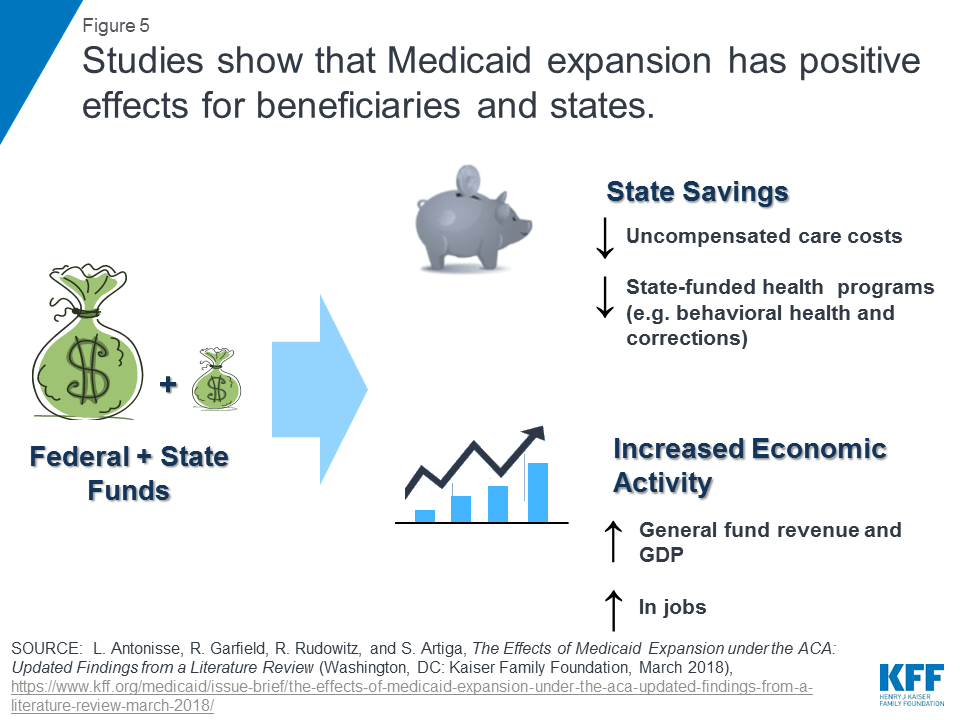
How is Medicaid expansion funded?
The federal government is financing most of the cost of expanding Medicaid, and a small portion is being paid by participating states. The costs fo...
How many people are enrolled in coverage due to Medicaid expansion?
As of 2019, there were about 10 million people who had become newly eligible for Medicaid due to the ACA’s expanded eligibility guidelines. But the...
What is the Medicaid coverage gap?
In the states that have not expanded Medicaid, there’s a coverage gap that leaves about 2.2 million people ineligible for any sort of affordable co...
Which states have expanded Medicaid?
As of 2021, Medicaid has been expanded in 38 states and DC (you can click on a state on this map for more information about each state): Alaska Ari...
Which states have refused to expand Medicaid?
As of 2021, the following states have not yet accepted federal funding to expand Medicaid: Alabama Florida Georgia Kansas Mississippi North Carolin...
What is the Affordable Care Act?
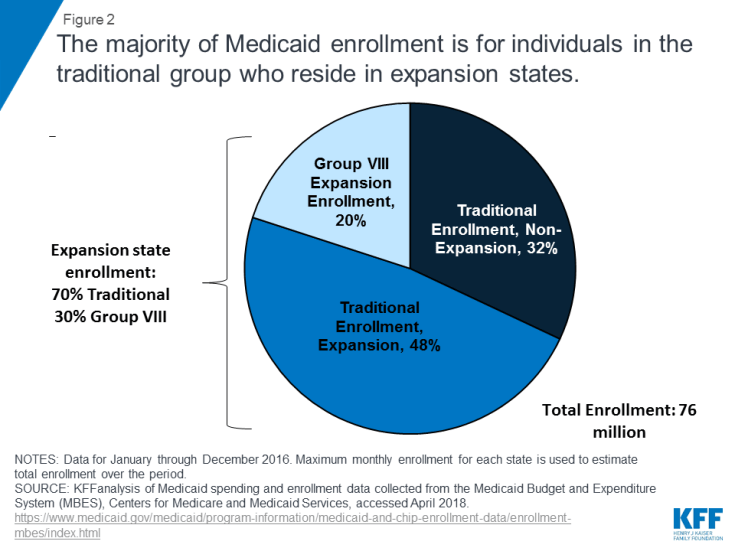
Medicaid—a federal/state partnership with shared authority and financing—is a health insurance program for low-income individuals, children, their parents, the elderly and people with disabilities. Medicaid pays for health care for more than 74.5 million people nationally.
Do all states have to meet the federal minimum requirements for Medicaid?
However, eligibility for Medicaid benefits varies widely among the states - all states must meet federal minimum requirements, but they have options for expanding Medicaid beyond the minimum federal guidelines, the details are outlined here.
How many states have expanded Medicaid?
Thirty-six states and DC have either already expanded Medicaid under the ACA or are in the process of doing so. Fourteen states continue to refuse to adopt Medicaid expansion, despite the fact that the federal government will always pay 90% of the cost.
Is the uninsured rate lower in Medicaid?
The uninsured rate, particularly among low-income residents, is considerably lower in Medicaid expansion states. A provision in the Affordable Care Act ( ACA) called for expansion of Medicaid eligibility in order to cover more low-income Americans. Under the expansion, Medicaid eligibility would be extended to adults up to age 64 ...
What is the ACA expansion?
A provision in the Affordable Care Act ( ACA) called for expansion of Medicaid eligibility in order to cover more low-income Americans. Under the expansion, Medicaid eligibility would be extended to adults up to age 64 with incomes up to 138 percent of the federal poverty level (133 percent plus a 5 percent income disregard).
Is Medicaid funded by the federal government?
The federal government is financing most of the cost of expanding Medicaid, and a small portion is being paid by participating states. The costs for enrollees who are newly eligible under the expanded guidelines was covered 100 percent by the federal government until 2016.
How much is Medicaid coverage in 2020?
That will gradually decrease to 90 percent by 2020, but will not go below that amount. As of 2019, official Medicaid data put the total newly-eligible enrollment at about 10 million.
How many people are on medicaid in 2019?
As of 2019, official Medicaid data put the total newly-eligible enrollment at about 10 million . Total enrollment in Medicaid/CHIP has increased by 26 percent since 2013, although enrollment growth is much higher than that average (34.4 percent) if we only consider states that have expanded Medicaid.
Which states have Medicaid expansion?
Five states — Texas, North Carolina, Florida, Georgia, and Tennessee — account for the lion’s share of the coverage gap population, and they are among the 14 states where expansion is still a contentious issue and the legislature and/or governor are still strongly opposed to accepting federal funding to expand Medicaid.
How many states have Medicaid expansion?
To date, 39 states (including DC) have adopted the Medicaid expansion and 12 states have not adopted the expansion. Current status for each state is based on KFF tracking and analysis of state expansion activity.
Which states have Section 1115 waivers?
Arizona, Arkansas, Indiana, Iowa, Michigan, Montana, Nebraska, New Hampshire, New Mexico, Ohio, and Utah have approved Section 1115 waivers to operate their Medicaid expansion programs in ways not otherwise allowed under federal law. Some of these Section 1115 waivers include work requirements, which the Biden Administration has recently begun ...
What is the name of the state that will replace the state's Medicaid expansion?
Arkansas. In April 2021, Governor Asa Hutchinson signed a bill passed by the Arkansas Legislature that would replace the state’s current Medicaid expansion program, Arkansas Works, with the Arkansas Health and Opportunity for Me (HOME) program, contingent on federal approval.
Does Arkansas Home have Medicaid?
Arkansas Home would allow expansion enrollees who comply with work requirements and monthly premiums to enroll in private marketplace plans while enrollees who opt out of these requirements would receive traditional fee-for-service Medicaid coverage.
When will Montana expand?
Montana. On April 18, 2019, the Montana Legislature passed a bill (which was signed by Governor Bullock on May 9, 2019) to continue the state’s expansion program with significant changes until 2025.
When will Medicaid be available in Oklahoma?
Oklahoma. Enrollment in Medicaid coverage under expansion in Oklahoma began on June 1, 2021, with coverage for these enrollees beginning on July 1, 2021. Oklahoma voters approved a ballot measure on June 30, 2020 which added Medicaid expansion to the state’s Constitution. Language in the approved measure prohibits the imposition ...
When did Oklahoma add Medicaid expansion?
Oklahoma voters approved a ballot measure on June 30, 2020 which added Medicaid expansion to the state’s Constitution. Language in the approved measure prohibits the imposition of any additional burdens or restrictions on eligibility or enrollment for the expansion population. Utah.
How long did it take to get Medicaid expansion in Michigan?
Michigan Medicaid expansion. It took nearly eight months to authorize the Healthy Michigan plan. Republican Gov. Rick Snyder announced his support in February 2013, saying it was a good move for public health and state finances. Snyder had support from numerous health care and advocacy groups, but was opposed by some Republicans in ...
Is Michigan a Medicaid expansion state?
Michigan proposed a Medicaid work requirement for the Medicaid expansion population that received federal approval in late 2018. The work requirement waiver is based on legislation the state enacted in 2018 (details below), and it took effect as of January 2020; non-exempt Medicaid expansion enrollees had to complete at least 80 hours per month of activities that could include work, school, job training, etc., and begin reporting their work hours as of February 2020.
When did Michigan expand Medicaid?
Michigan expanded Medicaid as of April 2014. The expanded Medicaid program is called Healthy Michigan, and it includes premiums for people with income above the poverty level. Nearly 750,000 Michiganders are enrolled in expanded Medicaid as of mid-2020, up from about 650,000 before the COVID-19 pandemic began.
What percentage of income is eligible for Medicaid in Michigan?
Residents are eligible for Michigan Medicaid with incomes up to 138 percent of the poverty level (as called for in the ACA), but the state obtained approval from the Obama administration to charge premiums equal to 2 percent of income for people with income above the poverty level.
How much money did Michigan save in 2016?
The researchers also determined that Michigan saved $235 million in 2016 as a result of Medicaid expansion, thanks to federal Medicaid funds covering some prison health care costs that were previously covered by the state.
When did Michigan's Medicaid work requirement take effect?
Michigan’s Medicaid work requirement proposal took effect January 1, 2020, but was soon overturned by a judge. Michigan proposed a Medicaid work requirement for the Medicaid expansion population that received federal approval in late 2018. The work requirement waiver is based on legislation the state enacted in 2018 (details below), ...
Who is the governor of Michigan who has opposed the Medicaid Work Requirement?
Gov. Gretchen Whitmer — who has long opposed the Medicaid work requirement but who took office after it had been enshrined in statute and approved by CMS — had asked Michigan lawmakers to delay implementation of the Medicaid work requirement until the lawsuit was resolved, in order to avoid wasting taxpayer dollars.
Is Medicaid expanding in New York?
Medicaid expansion in New York. New York has long been a healthcare reform front-runner, creating a guaranteed issue individual health insurance market decades ahead of the Affordable Care Act (ACA), and also expanding Medicaid to cover many low-income parents and childless adults long before the ACA reformed the nation’s health insurance system.
Is New York a healthcare reform state?
New York has long been a healthcare reform front-runner, creating a guaranteed issue individual health insurance market decades ahead of the Affordable Care Act (ACA), and also expanding Medicaid to cover many low-income parents and childless adults long before the ACA reformed the nation’s health insurance system.
When did New York expand Medicaid?
The state accepted the ACA’s provision to use federal funding to expand Medicaid in New York as of January 1, 2014, and between the fall of 2013 and August 2018, the state’s total Medicaid enrollment grew by 14 percent, to nearly 6.5 million people. New York State of Health, the state-run health insurance exchange, ...
Is Medicaid expansion beneficial in New York?
So the expansion of Medicaid in New York under the ACA has been particularly beneficial to the state from a financial perspective. For New York Medicaid enrollees who continue to be eligible based on pre-ACA guidelines, the state and federal government split the cost (since New York is a relatively wealthy state, ...
How many people would lose Medicaid in New York if the ACA was repealed?
In January 2017, as President Trump was poised to take office and it was clear that GOP lawmakers were going to push hard for ACA repeal, New York Governor Andrew Cuomo, announced that 2.7 million people were at risk of losing Medicaid coverage in New York if the ACA was repealed and not replaced with something equally robust, and that the state budget impact would be $3.7 billion.
What is the ACA in New York?
The ACA’s Medicaid provisions allowed New York to utilization federal funding to expand Medicaid to everyone with incomes up to 138 percent of poverty. New York went a step further than most other states by implementing the ACA’s Basic Health Program, which covers people with income a little too high for Medicaid.
What percentage of income is eligible for Medicaid in New York?
Adults in New York with incomes up to 138 percent of poverty level are now eligible for Medicaid. Pregnant women and children under the age of one are eligible with an income of up to 218 percent of poverty level (for Medicaid eligibility determinations, a pregnant woman counts as two people for household income calculations).
How much did Medicaid expansion cost in North Carolina?
The states’ portion will never exceed 10 percent, though. In North Carolina, the state’s cost to expand Medicaid is estimated at between $210 million ...
How much does it cost to expand medicaid in North Carolina?
In North Carolina, the state’s cost to expand Medicaid is estimated at between $210 million and $600 million per year. Cooper and other Medicaid expansion advocates have long noted that the state is missing out on billions of federal dollars by rejecting Medicaid expansion.
When did North Carolina start Medicaid?
North Carolina was one of the last states to adopt the Medicaid program: Only two states took longer to implement original Medicaid coverage. The first states to provide Medicaid did so in January 1966, and North Carolina’s program didn’t become effective until January 1970.
What percentage of poverty is covered by Medicaid?
The ACA called for Medicaid expansion in every state, covering all legally-present residents with incomes up to 133 percent of poverty (138 percent with the built-in five percent income disregard).
When was the Medicaid transition nixed?
And, then the February 2020 transition was nixed when the Gov. McCrory and the legislature failed to agree on a budget during the 2019 General Assembly session. Implementation and open enrollment in the managed Medicaid plans was halted following an announcement of the indefinite delay.
What did Governor McCrory say about Medicaid expansion?
Expansion discussion during McCrory administration. Former Governor McCrory said that he was open to the idea of Medicaid expansion, but only after they “fix the current system.”. This was a reference to the legislature’s Medicaid reform efforts, primarily aimed at transitioning to Medicaid managed care.
Who is Ken Goodman?
And State Rep. Ken Goodman (D, Richmond) — a Medicaid expansion supporter — questioned whether McCrory would have the political clout to expand coverage anyway, given SB4 and the fact that the majority of the state legislature was opposed to Medicaid expansion.
How to apply for medicaid in Florida?
Review Florida’s eligibility criteria, and if you believe you are eligible to enroll in Medicaid you have several options: 1 Enroll at Healthcare.gov (if you’re under 65 and don’t have Medicare). 2 Apply online at ACCESS Florida, or fill out a paper form. Use this application for low-income children, pregnant women, families, and aged or disabled individuals who are not currently receiving Supplemental Security Income (SSI). 3 Use this application to apply for food or cash assistance in addition to Medicaid. You should also use this form if you currently receive SSI or if you are applying for home-based and community services, hospice care, or nursing home care. 4 Submit a paper application submitted by mail, fax or in person to a local service center.
Does Florida have Medicaid?
Florida is one of 12 states that, as of August 2020, has not expanded Medicaid eligibility as allowed under Affordable Care Act (ACA). The ACA doesn’t provide subsidies for people with income below the poverty level, because the law called for them to have Medicaid instead. But in states that have refused Medicaid expansion people who aren’t ...
Does Florida have income limits for Medicaid?
Florida has set below-average limits for the mandatory coverage groups, and since the state has not accepted federal funding to expand Medicaid, the eligibility rules have not changed with the implementation of the ACA.
Has Florida expanded Medicaid?
Although Florida has not expanded Medicaid under the ACA, enrollment in the state’s program has continued to grow. Enrollment stood at 2.2 million in 2005, and had grown to 3.7 million by the end of 2013. By June 2020, total Florida Medicaid enrollment was about 3.7 million, and CHIP enrollment was about 219,200.
When did Florida start Medicaid?
Florida was one of the later states to implement a Medicaid, not adopting the program until January of 1970 (the first states to implement Medicaid did so in early 1966).
What percent of Florida Medicaid beneficiaries are HMOs?
Ninety percent of all Florida Medicaid beneficiaries are now enrolled in managed care plans, like health maintenance organizations (HMOs). The state hopes to improve quality through better coordination of care and save money through smaller networks of providers.
How much Medicaid did Florida lose?
According to an analysis by the Robert Wood Johnson Foundation and the Urban Institute, Florida was projected to lose out on $66.1 billion in Medicaid funding — more than any other state — over the decade beginning in 2014 as a result of their decision to not expand Medicaid.
How many people are in the Medicaid expansion?
Medicaid Expansion. More than 14.5 million are newly enrolled in Medicaid, and AAF estimates that 9.6 million of these individuals are newly eligible as a result of the Medicaid expansion provision, which has been implemented by 31 states and the District of Columbia.
How many people are newly insured under the Affordable Care Act?
The Department of Health and Human Services (HHS) recently announced that 20 million people are newly insured as a result of the Affordable Care Act (ACA). [i] This has led many to espouse claims that, accordingly, 20 million people would lose their health insurance if the ACA is repealed.
How many people are not receiving ACA subsidies?
Of the estimated 5.8 million newly insured in the individual market, at least 1 million are not receiving ACA subsidies. While some have gained employer-sponsored insurance (ESI), as many as 5.9 million may have lost ESI because of the ACA.
How many people lost their employer coverage?
Finally, at least a few million people are believed to have lost their employer coverage as a result of the ACA, particularly the cost and complexity of the many new regulations. Ultimately, the number of people likely to be negatively impacted by a repeal of the ACA is certainly less than 20 million.