Doctors can authorize up to 30 days of physical therapy at a time. But, if you need physical therapy beyond those 30 days, your doctor must re-authorize it. Until recently, Medicare had a cap on the number of physical therapy sessions you can have in a year. However, Medicare no longer enforces these physical therapy limits.
Full Answer
How much physical therapy will Medicare pay for?
On average, Medicare part B will pay between $97 and $105 for a 60-minute, 4-unit physical therapy treatment. The initial evaluation visit typically reimburses at a higher rate of $130 to $160 on average due to the higher relative value of the initial evaluation code. What determines Medicare Part B Reimbursement rates for Physical Therapy?
How much does each physical therapy visit cost?
The cost of physical therapy depends on the number of sessions needed, the physical therapist, the type of session, insurance and the geographical location. On average, a session, after the initial consult has been completed, can range anywhere from $60 to as much as $250 without insurance, but most insurance plans will cover physical therapy as long as it is deemed medically necessary.
How to make the most of physical therapy?
Physical therapy helps you retrain your body and become stronger to recover from an illness or injury. However, many people who attend appointments aren’t quite sure how to maximize their time with the specialist. Here are a few tips for getting the most out of your next session. 3 Tips for Maximizing Your Physical Recovery 1. Dress the Part
How many therapy sessions does Medicare allow?
Unlimited Messaging Therapy Ultimate: The top-tier subscription, this service provides text, video, and audio messaging, four live video sessions per month, and a therapist response within 24 hours.
How many PT sessions will Medicare pay for?
There's no limit on how much Medicare pays for your medically necessary outpatient therapy services in one calendar year.
How often does a PT have to see a Medicare patient?
The PT must recertify the POC “within 90 calendar days from the date of the initial treatment,” or if the patient's condition evolves in such a way that the therapist must revise long-term goals—whichever occurs first.
What does Medicare reimburse for physical therapy?
If your total therapy costs reach a certain amount, Medicare requires your provider to confirm that your therapy is medically necessary. In 2022, Original Medicare covers up to: $2,150 for PT and SLP before requiring your provider to indicate that your care is medically necessary.
Does Medicare cover physical therapy for back pain?
Summary: Medicare may cover diagnostic tests, surgery, physical therapy, and prescription drugs for back and neck pain. In addition, Medicare Advantage plans may cover wellness programs to help back and neck pain. Medicare generally doesn't cover chiropractic care.
How many physical therapy sessions do I need?
On average, non-surgical patients graduate in about 12 visits, but often start to feel improvement after just a few sessions. However, your progress and the number of physical therapy sessions you need will depend on your individual condition and commitment to therapy.
How long is a physical therapy script good for?
A valid doctor's prescription for physical therapy includes the doctor's orders for physical therapy, and the duration of those orders. You must use your prescription within 30 days of it being written to ensure its medical validity.
How do you maximize physical therapy billing?
Ten Ways Physical Therapists Can Maximize BillingSet goals. As a therapist, you've got a lot of experience in the goal-setting department. ... Track your progress. ... Increase efficiency. ... Educate yourself and your staff. ... Clean up your claims. ... Digitize. ... Know your payer mix. ... Keep an eye on cash flow.More items...•
What is the 8 minute rule?
The 8-minute rule states that to receive Medicare reimbursement, you must provide treatment for at least eight minutes. Using the “rule of eights,” billing units that are normally based on 15-minute increments spent with a patient can be standardized.
Does Medicare cover physical therapy for arthritis?
Medicare Part B Medicare will usually cover doctor's visits related to arthritis, physical therapy, and some DME, such as splints, braces, walkers, or canes. A person is often required to obtain prior authorization from Medicare before purchasing equipment or pursuing therapy services.
Does Medicare pay for physical therapy at home?
Medicare Part B medical insurance will cover at home physical therapy from certain providers including private practice therapists and certain home health care providers. If you qualify, your costs are $0 for home health physical therapy services.
Are nerve blocks covered by Medicare?
Medicare does not have a National Coverage Determination (NCD) for paravertebral facet joint/nerve blocks: diagnostic and therapeutic.
How Much Does Medicare pay for a chiropractic adjustment?
What parts of Medicare cover chiropractic care? Medicare Part B, the portion that helps people pay for doctor visits and some related treatments, covers some aspects of chiropractic care. Once a person meets their yearly deductible, Medicare will usually fund 80% of the cost for chiropractic treatment.
Does Medicare pay for physical therapy at home?
Medicare Part B medical insurance will cover at home physical therapy from certain providers including private practice therapists and certain home health care providers. If you qualify, your costs are $0 for home health physical therapy services.
What is a plan of care for physical therapy?
The POC consists of statements that specify the anticipated goals and expected outcomes, predicted level of optimal improvement, specific interventions to be used, and proposed duration and frequency of the interventions. The POC describes the specific patient/client management for the episode of physical therapy care.
Which of the following may certify a Medicare plan of care?
Medicare states that certification of the plan of care requires a dated signature on the plan of care, or some other document, by the physician or non-physician practitioner who is the primary care provider for the patient.
What is the Medicare cap for 2022?
$2,150KX Modifier and Exceptions Process This amount is indexed annually by the Medicare Economic Index (MEI). For 2022 this KX modifier threshold amount is: $2,150 for PT and SLP services combined, and. $2,150 for OT services.
How long can you get physical therapy with Medicare?
Therapy doctors are now paid based on a complex formula that considers several factors related to a patient’s needs. Doctors can authorize up to 30 days of physical therapy at a time. But, if you need physical therapy beyond that 30 days, ...
How much does Medicare pay for speech therapy?
However, the threshold amount that Medicare pays for physical and speech therapy combined is $3,000 before reviewing a patient’s case to ensure medical necessity. Also, once a patient spends $2,080 on physical and speech therapy, providers add special billing codes to flag this amount.
What do you need to do to get home therapy?
You must: Be under a doctor’s care. Improve or to maintain your current physical condition. Have your doctor must certify that you’re homebound. Also , Medicare pays a portion of the cost for Durable Medical Equipment used in your home therapy.
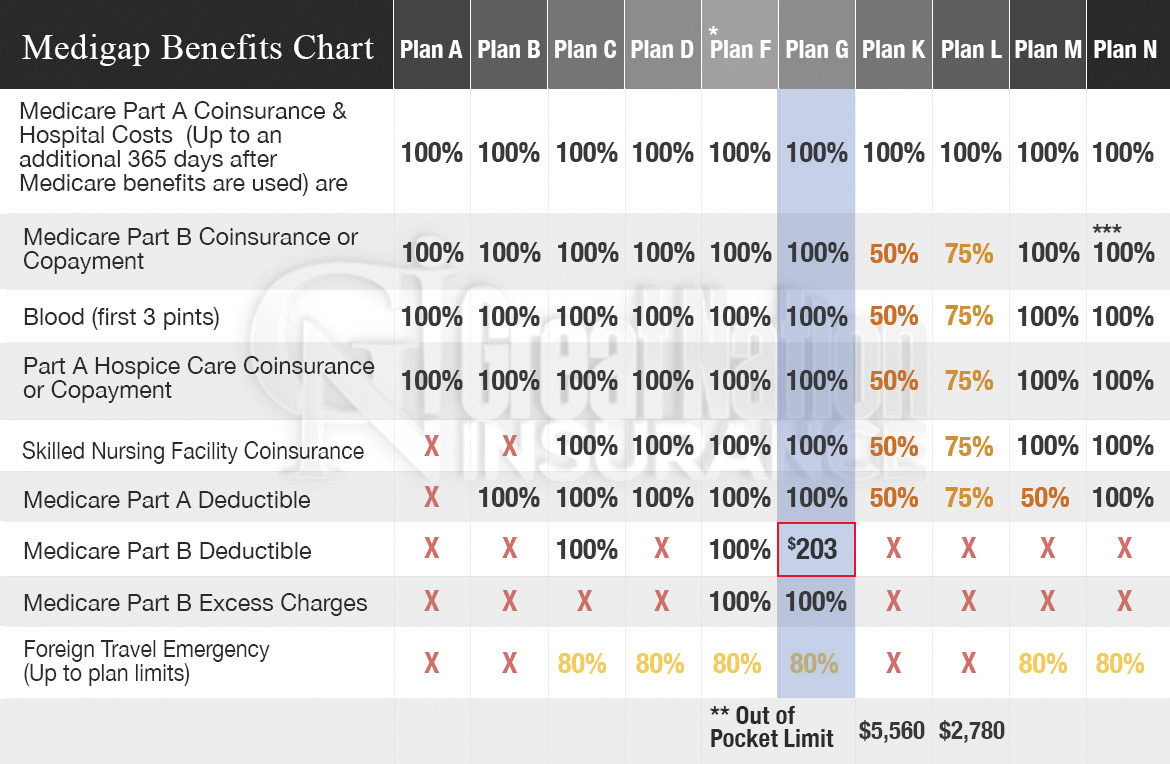
Does Medigap cover deductibles?
When you have Medigap, the plan pays your portion of the coinsurance bill. Some plans even cover deductibles. Those that anticipate needing physical therapy should consider Mediga p. To better explain how Medigap could benefit someone in need of physical therapy I’m going to use Josie as an example.
Does physical therapy improve quality of life?
Whether you’re in an accident or you have a medical condition, therapy can improve the quality of life. If a doctor says that physical therapy will improve your quality of life, you can consider it necessary. In the context below, we’ll go into detail about when Medicare coverage applies, how often coverage applies, ...
Does Medicare cover physiotherapy?
Some physical therapy doctors in the U.S. may use the term “physiotherapy” to describe what they do. Medicare will cover your therapy , regardless of whether it is called physical therapy or physiotherapy.
Is physical therapy good for chronic health?
Physical therapy can make a huge difference in your healing process after an injury or illness. And, it can help you manage chronic health issues. Our agents know the benefits of having quality coverage. To find the most suitable plan option for you, give us a call at the number above today!
Why is Physical Therapy Valuable?
According to the American Physical Therapy Association (APTA), physical therapy can help you regain or maintain your ability to move and function after injury or illness. Physical therapy can also help you manage your pain or overcome a disability.
Does Medicare Cover Physical Therapy?
Medicare covers physical therapy as a skilled service. Whether you receive physical therapy (PT) at home, in a facility or hospital, or a therapist’s office, the following conditions must be met:
What Parts of Medicare Cover Physical Therapy?
Part A (hospital insurance) covers physical therapy as an inpatient service in a hospital or skilled nursing facility (SNF) if it’s a Medicare-covered stay, or as part of your home health care benefit.
Does Medicare Cover In-home Physical Therapy?
Medicare Part A covers in-home physical therapy as a home health benefit under the following conditions:
What Are the Medicare Caps for Physical Therapy Coverage?
Medicare no longer caps medically necessary physical therapy coverage. For outpatient therapy in 2021, if you exceed $2,150 with physical therapy and speech-language pathology services combined, your therapy provider must add a modifier to their billing to show Medicare that you continue to need and benefit from therapy.
What are the different types of physical therapy?
Medical News Today describes several different types of physical therapy across a wide spectrum of conditions: 1 Orthopedic: Treats injuries that involve muscles, bones, ligaments, fascias and tendons. 2 Geriatric: Aids the elderly with conditions that impact mobility and physical function, such as arthritis, osteoporosis, Alzheimer’s, hip and joint replacements, balance disorders and incontinence. 3 Neurological: Addresses neurological disorders, Alzheimer’s, brain injury, cerebral palsy, multiple sclerosis, Parkinson’s disease, spinal cord injury and stroke. 4 Cardiovascular: Improves physical endurance and stamina. 5 Wound care: Includes manual therapies, electric stimulation and compression therapy. 6 Vestibular: Restores normal balance and coordination that can result from inner ear issues. 7 Decongestive: Promotes draining of fluid buildup.
How much is the Medicare Part B deductible for 2020?
In 2020, the Part B deductible is $198 per year under Original Medicare benefits.
What is Medicare Part B?
With your healthcare provider’s verification of medical necessity, Medicare Part B covers the evaluation and treatment of injuries and diseases that prohibit normal function. Physical therapy may be needed to remedy the issue, maintain the present functionality or slow the decline.
What is the difference between geriatric and orthopedic?
Orthopedic: Treats injuries that involve muscles, bones, ligaments, fascias and tendons. Geriatric: Aids the elderly with conditions that impact mobility and physical function, such as arthritis, osteoporosis, Alzheimer’s, hip and joint replacements, balance disorders and incontinence.
How much does physical therapy cost on Medicare?
Although Medicare does not have a spending limit on physical therapy sessions, once the cost reaches $2,080, a person’s healthcare provider will need to indicate that their care is medically necessary.
What happens after a physical therapist completes a physical therapy visit?
At this time, the therapist may release the individual from further physical therapy. Alternatively, the referring doctor may recommend participating in additional sessions.
What is the process of creating a physical therapy plan?
The process of creating and maintaining a physical therapy plan may include the following steps: A physical therapist evaluates the person who needs physical therapy and creates a plan of care. This plan includes a recommended number of sessions, treatment types, and treatment goals.
What is an example of a woman with Medicare?
Here is an example: A woman with Medicare was in a car accident and injured her knee. Her doctor recommended physical therapy to improve her strength and range of motion. She participated in the recommended physical therapy sessions and made improvements in strength but had not fully reached her goals for mobility.
Does Medicare consider progress in physical therapy?
Treatment progress is not the only consideration when Medicare evaluates continued funding for an individual’s physical therapy. For example, Medicare requires a physical therapist to recertify that physical therapy is medically necessary after the total costs for therapy exceed $2,080.
What is physical therapy and why is it so important for seniors?
Physical therapy is an important part of recovery for many seniors after undergoing an injury or surgery. This vital healthcare specialty includes the well-rounded evaluation, assessment, and treatment of individuals who deal with physical limitations as a result of illness, disability, surgery, or injury.
Does Medicare pay for physical therapy?
You may be pleasantly surprised to learn that Original Medicare will, in fact, pay for at least a portion of physical therapy visits that are considered to be medically necessary by a patient’s doctor.
How can I get even more comprehensive Medicare coverage for my specific healthcare needs?
The simple answer to the question “does Medicare cover physical therapy?” is yes, with conditions. That said, did you know that it may be possible to enroll in a Medicare plan that offers even more comprehensive healthcare coverage than Original Medicare?
Physical Therapy and Medicare Coverage
Medicare Part A can cover some of the cost of physical therapy at either an inpatient facility or your home. The longevity of the treatment as well as your deductibles and other payments are taken into consideration when calculating the overall costs for physical therapy coverage.
Medicare and the Costs of Physical Therapy
The costs of physical therapy vary depending on your Medicare coverage, but it can range between $75 to $350 per session (out of pocket). Fortunately, there are many ways to ease the financial burden if you qualify for coverage through Medicare.
Bottom Line
Medicare coverage for physical therapy largely depends on the specific plan and services you’re enrolled in. For the most part, Medicare can cover part or the full cost of physical therapy, depending on what your physician or physical therapist deems as medically necessary.
What is the threshold for a physical therapy session?
It is instead seen as a "threshold" limit. After you have spent $3,000 for physical therapy and speech therapy combined or $3,000 for occupational therapy, Medicare may audit your case to make sure continued sessions are medically necessary .
When did the Medicare cap on therapy sessions end?
There used to be a therapy cap on how much Medicare would pay but the cap was lifted in 2018. To be sure that services are not being overutilized, Medicare will audit cases after $3,000 is spent in a calendar year to make sure that continued therapy sessions are medically necessary.
What is the difference between occupational therapy and physical therapy?
Physical therapy aims to treat or at least improve an impairment whereas occupational therapy teaches you how to function with that impairment. For example, physical therapy strengthens a shoulder injury but occupational therapy helps you to use the shoulder in everyday activities. Speech therapy also falls under therapy services ...
What does it mean when a provider denies a therapy request?
If Medicare or Medicaid denies the request for therapy, it could be that the wrong diagnosis code has been selected.
How much is the therapy cap?
This was known as the therapy cap. In 2018, there was a $2,010 cap for physical therapy and speech therapy combined and a separate $2,010 cap for occupational therapy. However, later in 2018, Congress passed the Bipartisan Budget Act of 2018 and the therapy cap met its timely end. 2 The legislation affected claims retroactively starting on ...
Is home therapy covered by Medicare?
Most people will drive to an office or facility to complete their therapy sessions but some people may not have the means to get out of the house. In these cases, home therapy may be covered by Medicare or Medicaid . The first requirement is that you be homebound to receive home health services.
Is ride share a Medicare benefit?
As of 2019, some Medicare Advantage plans may be offering ride shares as a supplemental benefit. This could improve access to physical therapy and occupational therapy outside of the home for people who do not otherwise have the means to travel to their appointments.