What is beneficiaries Services Medicare?
Beneficiary Services Medicare is a health insurance program designed to assist the nation's elderly to meet hospital, medical, and other health costs. Medicare is available to most individuals 65 years of age and older.
What are the different types of Medicare Part A?
1 Medicare Part A. Medicare Part A is hospital insurance. ... 2 Medicare Part B. Medicare Part B is medical insurance that covers everyday care needs like doctor’s appointments, urgent care visits, counseling, medical equipment, and preventive care. 3 Medicare Part C. Medicare Part C is also called Medicare Advantage. ... 4 Medicare Part D. ...
How much does Medicare Part a cost?
Medicare costs at a glance. Most people don't pay a monthly premium for Part A (sometimes called " premium-free Part A "). If you buy Part A, you'll pay up to $437 each month. If you paid Medicare taxes for less than 30 quarters, the standard Part A premium is $437. If you paid Medicare taxes for 30-39 quarters, the standard Part A premium is $240.
What happens if a Medicare beneficiary has other health insurance?
When a Medicare beneficiary has other insurance (like employer group health coverage), rules dictate which payer is responsible for paying first. Please review the Reporting Other Health Insurance page for information on how and when to report other health plan coverage to CMS.
What is the cost for most Medicare beneficiaries?
A total of 5.1 million elderly accounted for expenditures in Medicaid of $54.5 billion, an average of $10,656 per elderly beneficiary. Overall, 16.6% of the elderly had spending over $25,000, which accounted for 64.7% of the spending on the elderly, or 19.6% of all Medicaid spending.
What are 3 groups of people covered by Medicare?
What's Medicare?People who are 65 or older.Certain younger people with disabilities.People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
How much does Medicare cost per recipient?
In 2021, the average Medicare cost per beneficiary in the US was $15,671, an increase of 9% or $1,323 from 2020.
What does Medicare beneficiary pay?
Beneficiaries enrolled in Part B are generally required to pay a monthly premium ($104.90 in 2015). Beneficiaries with annual incomes greater than $85,000 for a single person or $170,000 for a married couple in 2015 pay a higher, income-related monthly Part B premium, ranging from $146.90 to $335.70.
What are Medicare costs for 2021?
The standard monthly premium for Medicare Part B enrollees will be $148.50 for 2021, an increase of $3.90 from $144.60 in 2020. The annual deductible for all Medicare Part B beneficiaries is $203 in 2021, an increase of $5 from the annual deductible of $198 in 2020.
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
How much do Medicare beneficiaries spend out of pocket on health care?
Medicare Beneficiaries' Spending for Health Care People covered by traditional Medicare paid an average of $6,168 for health care in 2018. They spent almost half of that money (47 percent) on Medicare or supplemental insurance premiums.
Are Medicare premiums based on income?
Medicare premiums are based on your modified adjusted gross income, or MAGI. That's your total adjusted gross income plus tax-exempt interest, as gleaned from the most recent tax data Social Security has from the IRS.
How much is deducted from Social Security for Medicare?
In 2021, based on the average social security benefit of $1,514, a beneficiary paid around 9.8 percent of their income for the Part B premium. Next year, that figure will increase to 10.6 percent.
How do you qualify to get $144 back from Medicare?
How do I qualify for the giveback?Are enrolled in Part A and Part B.Do not rely on government or other assistance for your Part B premium.Live in the zip code service area of a plan that offers this program.Enroll in an MA plan that provides a giveback benefit.
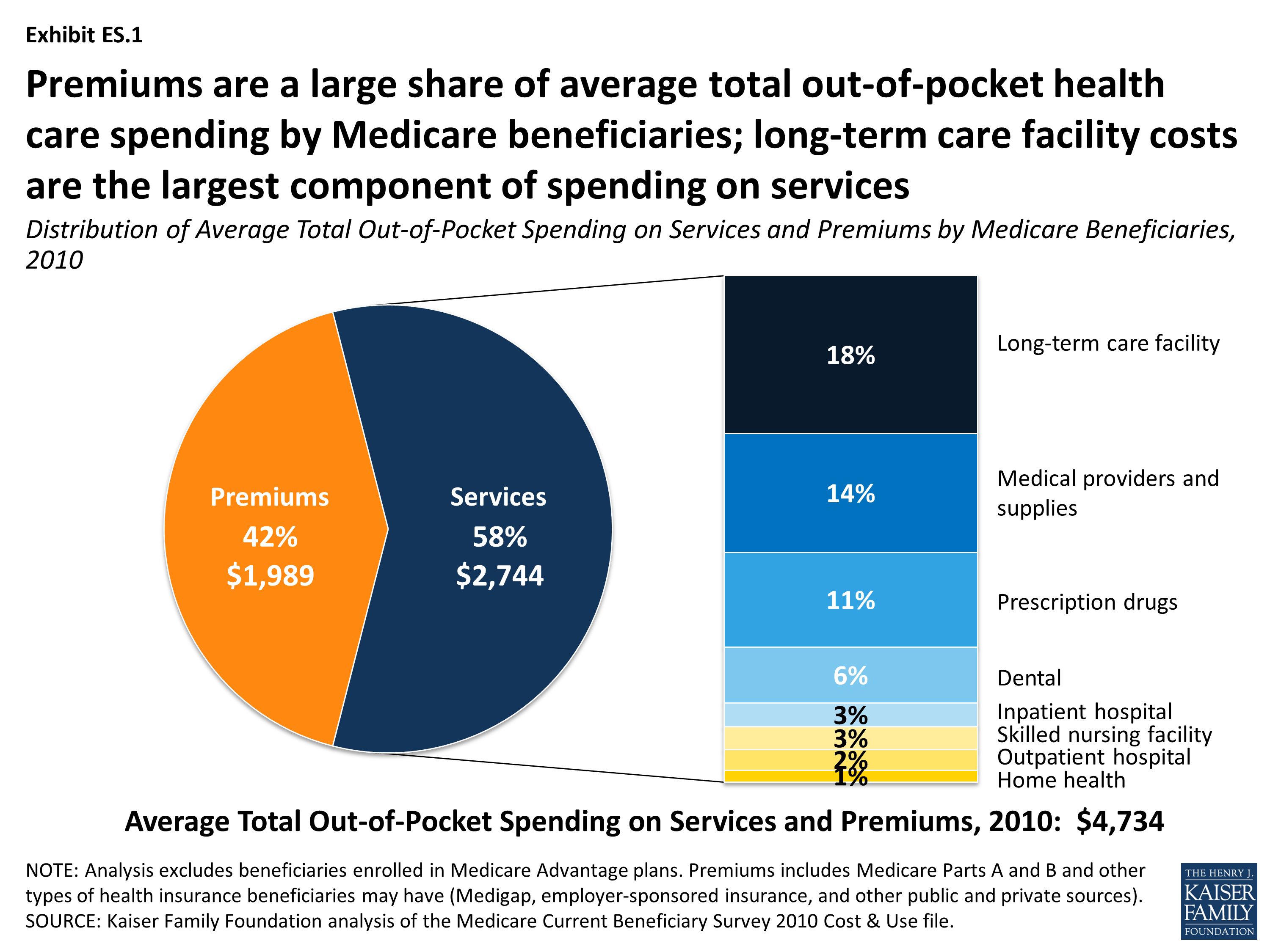
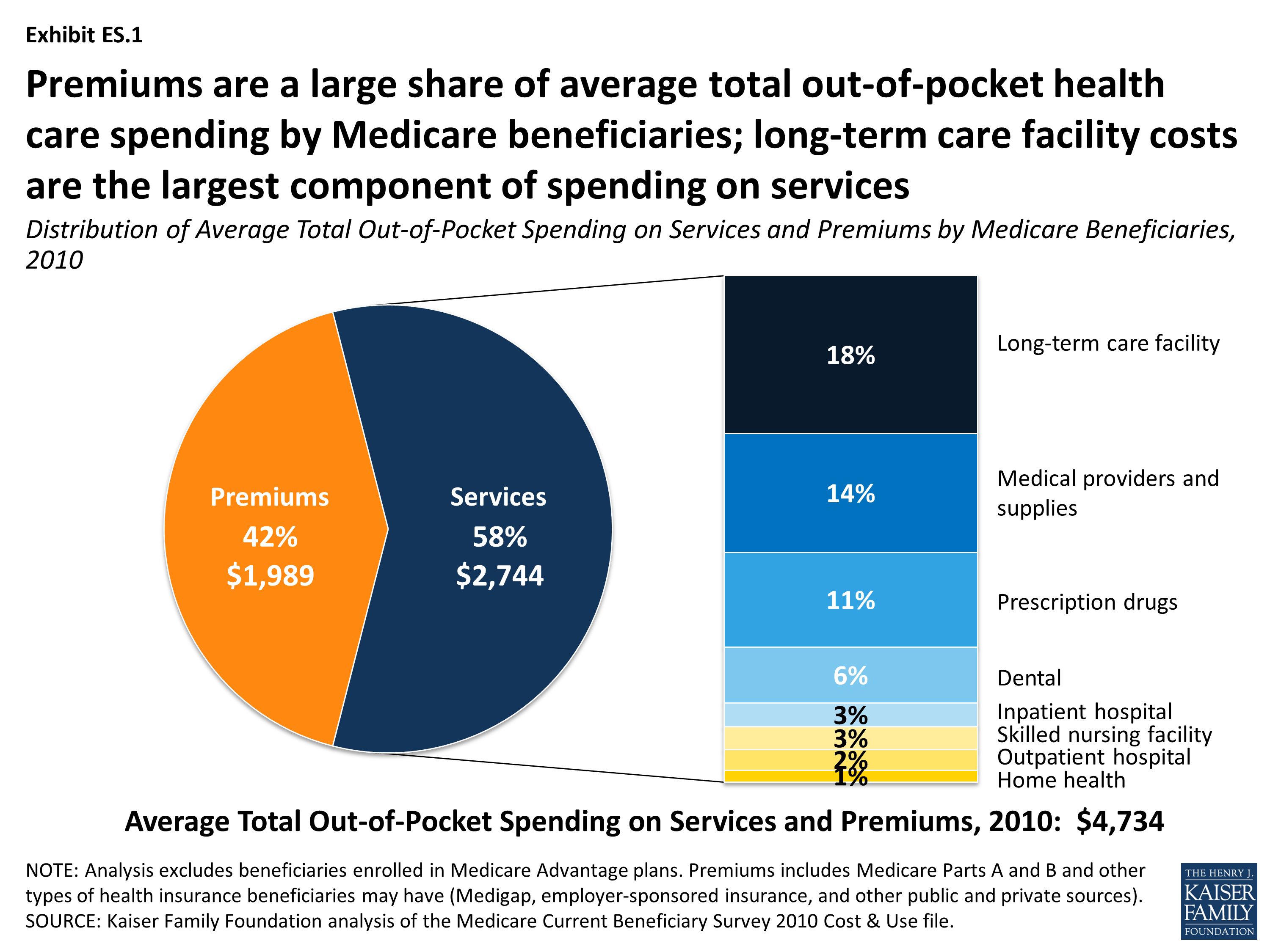
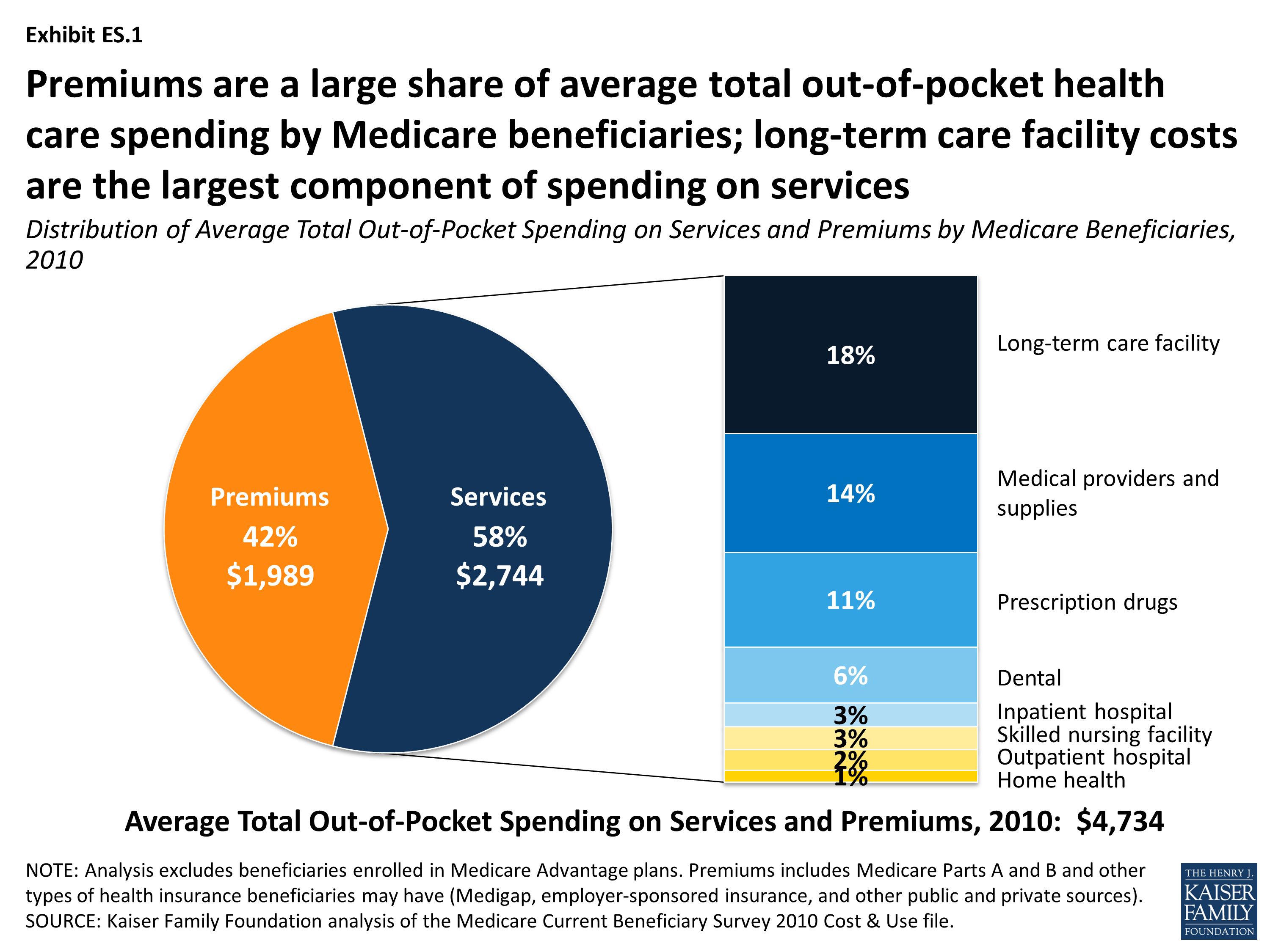
How much did Medicare spend in 2010?
In 2010, Medicare beneficiaries spent $4,745 out of their own pockets for health care spending, on average, including premiums for Medicare and other types of supplemental insurance and costs incurred for medical and long-term care services (Figure 6). Premiums for Medicare and supplemental insurance accounted for 42 percent ...
How much is the Part A deductible for 2015?
In 2015, the Part A deductible for each “spell of illness” is $1,260 for an inpatient hospital stay. Beneficiaries are generally subject to coinsurance for Part A benefits, including extended inpatient stays in a hospital ($315 per day for days 61-90 and $630 per day for days 91-150 in 2015) or skilled nursing facility ...
Does Supplemental Insurance cover out-of-pocket expenses?
Supplemental insurance coverage can help beneficiaries pay their out-of-pocket costs for Medicare-covered services. Even with supplemental insurance, however, beneficiaries can face out-of-pocket expenses in the form of copayments for services including physician visits and prescription drugs as well as costs for services not covered by Medicare.
Is Part B deductible?
Part B benefits are subject to an annual deductible ($147 in 2015), and most Part B services are subject to coinsurance of 20 percent. No coinsurance or deductible is charged for the annual wellness visit or for preventive services that are rated ‘A’ or ‘B’ by the USPSTF.
Does Medicare Advantage pay monthly premium?
Medicare Advantage plan enrollees generally pay the monthly Part B premium and many also pay an additional premium directly to their plan. Medicare Advantage plans are required to place a limit on beneficiaries’ out-of-pocket expenses for Medicare Part A and Part B covered services ($6,700 in 2015). This limit is not applied to beneficiaries in ...
What happens when Medicare beneficiaries have other health insurance?
When a Medicare beneficiary has other insurance (like employer group health coverage), rules dictate which payer is responsible for paying first. Please review the Reporting Other Health Insurance page for information on how and when to report other health plan coverage to CMS.
What is Medicare for seniors?
Medicare is a health insurance program designed to assist the nation's elderly to meet hospital, medical, and other health costs. Medicare is available to most individuals 65 years of age and older.
What is the CMS?
The Centers for Medicare & Medicaid Services (CMS) is the federal agency that manages Medicare. When a Medicare beneficiary has other health insurance or coverage, each type of coverage is called a "payer.". "Coordination of benefits" rules decide which one is the primary payer (i.e., which one pays first). To help ensure that claims are paid ...
How long does it take for Medicare to pay a claim?
When a Medicare beneficiary is involved in a no-fault, liability, or workers’ compensation case, his/her doctor or other provider may bill Medicare if the insurance company responsible for paying primary does not pay the claim promptly (usually within 120 days).
Does Medicare pay a conditional payment?
In these cases, Medicare may make a conditional payment to pay the bill. These payments are "conditional" because if the beneficiary receives an insurance or workers’ compensation settlement, judgment, award, or other payment, Medicare is entitled to be repaid for the items and services it paid.
How much does Medicare pay for outpatient therapy?
After your deductible is met, you typically pay 20% of the Medicare-approved amount for most doctor services (including most doctor services while you're a hospital inpatient), outpatient therapy, and Durable Medical Equipment (DME) Part C premium. The Part C monthly Premium varies by plan.
What is Medicare Advantage Plan?
A Medicare Advantage Plan (Part C) (like an HMO or PPO) or another Medicare health plan that offers Medicare prescription drug coverage. Creditable prescription drug coverage. In general, you'll have to pay this penalty for as long as you have a Medicare drug plan.
How much is coinsurance for days 91 and beyond?
Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime). Beyond Lifetime reserve days : All costs. Note. You pay for private-duty nursing, a television, or a phone in your room.
How much is coinsurance for 61-90?
Days 61-90: $371 coinsurance per day of each benefit period. Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime) Beyond lifetime reserve days: all costs. Part B premium.
What happens if you don't buy Medicare?
If you don't buy it when you're first eligible, your monthly premium may go up 10%. (You'll have to pay the higher premium for twice the number of years you could have had Part A, but didn't sign up.) Part A costs if you have Original Medicare. Note.
Do you pay more for outpatient services in a hospital?
For services that can also be provided in a doctor’s office, you may pay more for outpatient services you get in a hospital than you’ll pay for the same care in a doctor’s office . However, the hospital outpatient Copayment for the service is capped at the inpatient deductible amount.
Does Medicare cover room and board?
Medicare doesn't cover room and board when you get hospice care in your home or another facility where you live (like a nursing home). $1,484 Deductible for each Benefit period . Days 1–60: $0 Coinsurance for each benefit period. Days 61–90: $371 coinsurance per day of each benefit period.
What are the parts of Medicare?
Each part covers different healthcare services you might need. Currently, the four parts of Medicare are: Medicare Part A. Medicare Part A is hospital insurance. It covers you during short-term inpatient stays in hospitals and for services like hospice.
How many people are on medicare in 2018?
Medicare is a widely used program. In 2018, nearly 60,000 Americans were enrolled in Medicare. This number is projected to continue growing each year. Despite its popularity, Medicare can be a source of confusion for many people. Each part of Medicare covers different services and has different costs.
How long do you have to sign up for Medicare if you have delayed enrollment?
Special enrollment period. If you delayed Medicare enrollment for an approved reason, you can later enroll during a special enrollment period. You have 8 months from the end of your coverage or the end of your employment to sign up without penalty.
What is the maximum amount you can pay for Medicare in 2021?
In 2021, the out-of-pocket maximum for plans is $7,550. Note.
What does Medicare Part A cover?
Medicare Part A covers the care you receive when you’re admitted to a facility like a hospital or hospice center. Part A will pick up all the costs while you’re there, including costs normally covered by parts B or D.
What is Medicare for seniors?
Medicare is a health insurance program for people ages 65 and older, as well as those with certain health conditions and disabilities. Medicare is a federal program that’s funded by taxpayer contributions to the Social Security Administration.
How old do you have to be to get Medicare?
You can enroll in Medicare when you meet one of these conditions: you’re turning 65 years old. you’ve been receiving Social Security Disability Insurance (SSDI) for 24 months at any age. you have a diagnosis of end-stage renal disease (ESRD) or amyotrophic lateral sclerosis (ALS) at any age.