Does Medicare cover my MNT services?
Section 105 of the Benefits Improvement and Protection (BIPA) Act of 2000 permits Medicare coverage of MNT services when furnished by a registered dietitian or nutrition professional meeting certain requirements, effective January 1, 2002.
What should an RDN review for Medicare Part B beneficiaries?
For Medicare Part B beneficiaries with diabetes or kidney disease, RDNs must review how they provide services to these individuals in order to comply with Medicare regulations.
Does Medicare cover MNT if I get dialysis?
If you get dialysis in a dialysis facility, Medicare covers MNT as part of your overall dialysis care. If you’re in a rural area, a Registered Dietitian or other nutritional professional in a different location may be able to provide MNT to you through telehealth. Return to search results
What happens if a Medicare consumer needs more time for MNT?
If an RD determines that a Medicare consumer needs more time to understand and make behavior changes to meet the MNT goals, then the RD obtains a new referral from the treating physician for additional hours of MNT. DSMT and MNT The CMS considers DSMT and MNT Same as MNT Benefits complementary services.
Can dietitians bill Medicare?
Section 105 of BIPA permits Medicare coverage of Medical Nutrition Therapy (MNT) services when furnished by a registered dietitian or nutrition professional meeting certain requirements.
What can registered dietitians bill for?
The most common CPT codes dietitians can use to bill are : 97802, 97803 and 97804. The CPT codes 97802 and 97803 represent codes dietitians use to bill for individual MNT visits. While the CPT code 97804 would be used to bill for groups of patients of two or more.
Does Medicare cover dietary consult?
Medicare Part B may cover a dietitian or nutritionist if your doctor decides it's medically necessary. Medicare may also cover diabetic counseling, weight-loss counseling, obesity screenings and more.
Can a nurse practitioner order MNT?
However, unlike DSMT that allows for a qualified provider, including a physician, nurse practitioner (NP), or physician assistant (PA) to write an order for DSMT services, MNT can only be provided based on a physician referral.
What codes can dietitians bill?
Licensed dietitians and licensed nutritionists can bill for procedure/service codes S9470, 97802, 97803, and G0447 for diagnosis codes other than eating disorders.
What is the difference between nutrition education and MNT?
Dietetics professional determines the nutrition problem as the individual's knowledge deficit on food choices or cooking techniques for a healthy heart. MNT: RD makes MNT nutrition diagnosis after analyzing assessment data.
What MNT is currently reimbursed by Medicare?
Medical nutrition therapy is covered by Medicare for diagnoses of diabetes, non-dialysis kidney disease, and 36 months post kidney transplant when a Medicare beneficiary has been referred by a physician, and when provided by an RDN who is enrolled as a Medicare Provider.
How do I bill CPT 97802?
Billing Requirements CPT 97802. This service will be billed on the CMS-1450, or its electronic equivalent, but will not change the enrollment requirement for dieticians/nutritionists. The cost of the service is billed under revenue code 942 in FL 42.
Is a dietitian a healthcare professional?
Dietitians are qualified and regulated health professionals that assess, diagnose and treat dietary and nutritional problems at an individual and wider public-health level.
How are dietitians reimbursed?
Dietitians are considered “fee-for-service” providers, meaning that dietitians provide a service to clients and are then reimbursed later by insurance payers with an amount designated within their specific fee schedule.
Does Medicare cover CPT code 97803?
A. Background: As part of CMS' process for adding services to the list of Medicare telehealth services, CMS added individual medical nutrition therapy (MNT) as represented by HCPCS codes G0270, 97802 and 97803 to the list of Medicare telehealth services.
Can CDE bill Medicare?
A: RNs and CDEs are not recognized as Medicare providers, so they can't bill for services under their provider numbers. In order to bill Medicare for DSMT, you must have an accredited program through either the ADA or AADE.
What is MNT in diabetes?
Medical nutrition therapy (MNT) is a key component of diabetes education and management. MNT is defined as a “nutrition-based treatment provided by a registered dietitian nutritionist.” It includes “a nutrition diagnosis as well as therapeutic and counseling services to help manage diabetes.” 57
What is DSMT in healthcare?
DSMT is provided by diabetes educators who: Are licensed or nationally registered health care professionals. Provide overall guidance related to all aspects of diabetes. Increase the person with diabetes’s knowledge and skill about the disease.
When did Medicare start covering outpatient DSMT?
Section 4105 of the Balanced Budget Act (BBA) of 1997 permits Medicare coverage of the outpatient DSMT services when these services are furnished by a certified provider who meets certain quality standards, effective July 1, 1998. Provider Qualifications and Requirements.
How many hours of training is required for DSMT?
When training under a POC is changed, the treating provider must sign it. In the initial DSMT benefit, nine of the 10 hours must be provided in a group setting (2–20 individuals) unless special conditions exist: No group class is available within two months of the date the training is ordered.
What is the DSMT statute?
Statute. Section 105 of the Benefits Improvement and Protection (BIPA) Act of 2000 permits Medicare coverage of MNT services when furnished by a registered dietitian or nutrition professional meeting certain requirements , effective January 1, 2002.
Can DSMT and MNT be provided on the same date?
DSMT and MNT services cannot be provided on the same date. No payment will be made for group sessions unattended (class attendance sheet) Only face-to-face time with patient. DSMT and MNT services cannot be provided on the same date.
Can a facility have multiple units of the G0109?
Yes, if facility does not have one. Yes, if facility does not have one. Multiple units of the codes can be used based on medical necessity and the complexity of the MNT decision-making. G0109 – Diabetes outpatient self-mgmt training services, group session (two or more), per 30 minutes.
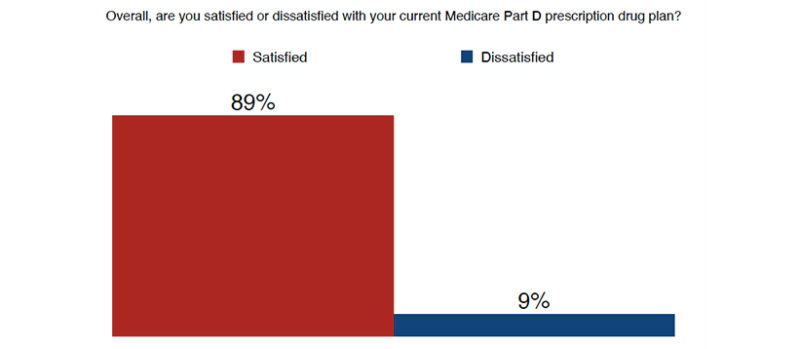
Does Medicare cover DSMT?
This means Medicare will cover both DSMT and MNT without decreasing either benefit as long as the referring physician determines that both are medically necessary. CMS considers DSMT and MNT complementary services.
Who does medicaid cover?
Medicaid provides health coverage to millions of low-income Americans, including eligible adults, children, pregnant women, the elderly, and people with disabilities. As dietitians, it's also wise to understand Medicaid coverage, which is administered by states and thus varies state to state.
Can I get credentialed for private practice insurance?
Yes, getting credentialed and contracted with private practice insurance companies certainly can be challenging, but it doesn't have to be daunting. Navigating the reimbursement maze on behalf of clients and patients also can be tricky, but the following guide provides a roadmap to help.
Can RDs take Medicare?
In addition to self-pay and private insurance, RDs can accept public or government insurance on behalf of clients in the form of Medicare and Medicaid. Medicare is a federal health insurance program that provides insurance for US citizens aged 65 and older, as well as those younger than 65 with certain disabilities.
Can a dietitian accept insurance?
When dietitians choose to accept insurance, they can still set their billable rate, but the insurance company will set the reimbursement rate. Research what's considered a competitive rate for your geographic location, and when possible, negotiate for a higher reimbursement level from the carrier.
Does Medicare cover kidney transplants?
Medicare covers individuals with diabetes (all types except prediabetes) and kidney disease (except inpatient dialysis) and for three years following a kidney transplant. By becoming Medicare Part B providers, dietitians can seek referrals from physicians and make a difference in this growing and underserved population.
Does Medicaid cover telehealth?
For example, in select states, Medicaid covers telehealth, nutrition counseling for pregnant women who are considered at risk nutritionally, and preventive nutrition assessments for children up to age 21. Yet, in other states, Medicaid may not cover such services.
Can a dietitian take self pay?
Some dietitians, however, opt to take self-pay clients only, citing that accepting insurance may lead to more no-shows or cancellations if clients aren't "on the hook" and paying via cash, check, or credit card. However, dietitians who have moved from self-pay to accepting insurance often see growth in their practices.
