If Medicare is primary, it means that Medicare will pay any health expenses first. Your health insurance through your employer will pay second and cover either some or all of the costs left over. If Medicare pays secondary to your insurance through your employer, your employer’s insurance pays first. Medicare covers any remaining costs.
Full Answer
What does Medicare cover and how does it work?
While Original Medicare insurance covers 80 percent of medical and hospital expenses, beneficiaries are responsible for the remaining 20 percent, as well as copayments, coinsurance, and deductibles. And, unless you have additional coverage through a prescription drug (Part D) plan, you end up paying for all your medications out of pocket.
How can you tell if someone has Medicare?
- individual was no longer serving as a volunteer outside of the United States;
- organization no longer has tax-exempt status; or
- individual no longer has health insurance that provides coverage outside of the United States.
What is Medicare supplement insurance and how it works?
- You must have Medicare Part A and Part B.
- A Medigap policy is different from a Medicare Advantage Plan. ...
- You pay the private insurance company a monthly premium The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage. ...
- A Medigap policy only covers one person. ...
How do iGet Medicare as your primary insurance?
Medicare and a private health plan – Typically, Medicare is considered primary if the worker is 65 or older and his or her employer has less than 20 employees. A private insurer is primary if the employer has 20 or more employees. Primary insurance. The primary insurance payer is the insurance company responsible for paying the claim first.

Can I keep my insurance if I have Medicare?
It is possible to have both private insurance and Medicare at the same time. When you have both, a process called “coordination of benefits” determines which insurance provider pays first. This provider is called the primary payer.
Is Medicare separate from insurance?
Original Medicare includes Medicare Part A (Hospital Insurance) and Part B (Medical Insurance). You can join a separate Medicare drug plan to get Medicare drug coverage (Part D).
How do Medicare premiums work?
Medicare premiums are based on your modified adjusted gross income, or MAGI. That's your total adjusted gross income plus tax-exempt interest, as gleaned from the most recent tax data Social Security has from the IRS.
Does Medicare pay for everything?
Original Medicare (Parts A & B) covers many medical and hospital services. But it doesn't cover everything.
Is Medicare primary or secondary insurance?
Medicare is always primary if it's your only form of coverage. When you introduce another form of coverage into the picture, there's predetermined coordination of benefits. The coordination of benefits will determine what form of coverage is primary and what form of coverage is secondary.
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
How much does Social Security take out for Medicare each month?
In 2021, based on the average social security benefit of $1,514, a beneficiary paid around 9.8 percent of their income for the Part B premium. Next year, that figure will increase to 10.6 percent.
How much is taken out of your Social Security check for Medicare?
Medicare Part B If your 2020 income was $91,000 to $408,999, your premium will be $544.30. With an income of $409,000 or more, you'll need to pay $578.30. If you receive Social Security benefits, your monthly premium will be deducted automatically from that amount.
Is Medicare Part A and B free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
Does Medicare pay 100 percent of hospital bills?
According to the Centers for Medicare and Medicaid Services (CMS), more than 60 million people are covered by Medicare. Although Medicare covers most medically necessary inpatient and outpatient health expenses, Medicare reimbursement sometimes does not pay 100% of your medical costs.
What will Medicare not pay for?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
What is the maximum out of pocket for Medicare?
Out-of-pocket limit. In 2021, the Medicare Advantage out-of-pocket limit is set at $7,550. This means plans can set limits below this amount but cannot ask you to pay more than that out of pocket.
How does Original Medicare work?
Original Medicare covers most, but not all of the costs for approved health care services and supplies. After you meet your deductible, you pay your share of costs for services and supplies as you get them.
How does Medicare Advantage work?
Medicare Advantage bundles your Part A, Part B, and usually Part D coverage into one plan. Plans may offer some extra benefits that Original Medicare doesn’t cover — like vision, hearing, and dental services.
How long does Medicare coverage last?
This special period lasts for eight months after the first month you go without your employer’s health insurance. Many people avoid having a coverage gap by signing up for Medicare the month before your employer’s health insurance coverage ends.
What is a small group health plan?
Since your employer has less than 20 employees, Medicare calls this employer health insurance coverage a small group health plan. If your employer’s insurance covers more than 20 employees, Medicare will pay secondary and call your work-related coverage a Group Health Plan (GHP).
Does Medicare pay second to employer?
Your health insurance through your employer will pay second and cover either some or all of the costs left over. If Medicare pays secondary to your insurance through your employer, your employer’s insurance pays first. Medicare covers any remaining costs. Depending on your employer’s size, Medicare will work with your employer’s health insurance ...
Does Medicare cover health insurance?
Medicare covers any remaining costs. Depending on your employer’s size, Medicare will work with your employer’s health insurance coverage in different ways. If your company has 20 employees or less and you’re over 65, Medicare will pay primary. Since your employer has less than 20 employees, Medicare calls this employer health insurance coverage ...
Can an employer refuse to pay Medicare?
The first problem is that your employer can legally refuse to make any health-related medical payments until Medicare pays first. If you delay coverage and your employer’s health insurance pays primary when it was supposed to be secondary and pick up any leftover costs, it could recoup payments.
How does Medicare work?
Examples of how coordination of benefits works with Medicare include: 1 Medicare recipients who have retiree insurance from a former employer or a spouse’s former employer will have their claims paid by Medicare first and their retiree insurance carrier second. 2 Medicare recipients who are 65 years of age or older and have health insurance coverage through employers with 20 or more employees will have their claims paid by their employer’s health plan first and Medicare second. 3 Medicare recipients who are under 65 years of age and disabled with health insurance coverage through employers with less than 100 employees will have their claims paid by Medicare first and by their employer’s health plan second.
What is Medicare coordination?
Coordination of Benefits with Private Insurance Plan. When a Medicare recipient had private health insurance not related to Medicare, Medicare benefits must be coordinated with that plan provider in order to establish which plan is the primary or secondary payer.
How old do you have to be to get Medicare?
Medicare recipients who are 65 years of age or older and have health insurance coverage through employers with 20 or more employees will have their claims paid by their employer’s health plan first and Medicare second.
Does Medigap cover foreign travel?
For certain plans, Medigap adds a few new benefits, such as foreign travel coverage. The monthly premium for one of these plans is separate from the premium paid for Original Medicare. In order to make identifying Medigap plans easier, they follow a letter-name standardization in most states.
Does Medicare provide expanded benefits?
Through these contractual relationships, Medicare is able to provide recipients with an expanded or enhanced set of benefits in a variety of ways.
How does Medicare work?
Here's how Medicare payments work if your employer covers you: 1 If you work for a company with fewer than 20 employees, Medicare is usually considered primary and your employer is secondary. 2 If you work for a larger company, your employer is primary and Medicare is secondary. 3 If Medicare is the secondary payer, it will reimburse based on what the employer paid, what is allowed in Medicare and what the doctor or provider charged. You will then have to pay what's left over.
How does Medicare work if you work for a company?
Here's how Medicare payments work if your employer covers you: If you work for a company with fewer than 20 employees, Medicare is usually considered primary and your employer is secondary. If you work for a larger company, your employer is primary and Medicare is secondary.
What is Cobra insurance?
COBRA. COBRA lets you keep your employer group health insurance plan for a limited time after your employment ends. This continuation coverage is meant to protect you from losing your health insurance immediately after you lose a job. If you're on Medicare, Medicare pays first and COBRA is secondary.
How to decide if you have dual health insurance?
When deciding whether to have dual health insurance plans, you should run the numbers to see whether paying for two plans would be more than offset by having two insurance plans paying for medical care. If you have further questions about Medicare and COB, call Medicare at 855-798-2627.
Does Medicare cover VA?
Medicare doesn't cover services within the VA. Unlike the other scenarios on this page, there is no primary or secondary payer when it comes to VA vs. Medicare. Having both coverage gives veterans the option to get care from either VA or civilian doctors depending on the situation.
Does Medicare pay a doctor if they are owed money?
The rest is on you if the doctor is still owed money. If Medicare is the secondary payer and the primary insurer doesn't pay swiftly enough, Medicare will make conditional payments to a provider when "there is evidence that the primary plan does not pay promptly.".
Can you have both Medicare and Medicaid?
You're able to have both Medicare and Medicaid. In fact, it's fairly common for people in nursing homes to have both coverage help pay for their care. Medicaid is always the payer of last resort when it pertains to COB. So, Medicare will pay first; Medicaid is the secondary payer.
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. at the start of each year, and you usually pay 20% of the cost of the Medicare-approved service, called coinsurance.
What is Medicare for people 65 and older?
Medicare is the federal health insurance program for: People who are 65 or older. Certain younger people with disabilities. People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
Do you pay Medicare premiums if you are working?
You usually don't pay a monthly premium for Part A if you or your spouse paid Medicare taxes for a certain amount of time while working. This is sometimes called "premium-free Part A."
Does Medicare Advantage cover vision?
Most plans offer extra benefits that Original Medicare doesn’t cover — like vision, hearing, dental, and more. Medicare Advantage Plans have yearly contracts with Medicare and must follow Medicare’s coverage rules. The plan must notify you about any changes before the start of the next enrollment year.
Does Medicare cover all of the costs of health care?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like copayments, coinsurance, and deductibles.
Does Medicare cover prescription drugs?
Medicare drug coverage helps pay for prescription drugs you need. To get Medicare drug coverage, you must join a Medicare-approved plan that offers drug coverage (this includes Medicare drug plans and Medicare Advantage Plans with drug coverage).
What do I need to know about Medicare?
What else do I need to know about Original Medicare? 1 You generally pay a set amount for your health care (#N#deductible#N#The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay.#N#) before Medicare pays its share. Then, Medicare pays its share, and you pay your share (#N#coinsurance#N#An amount you may be required to pay as your share of the cost for services after you pay any deductibles. Coinsurance is usually a percentage (for example, 20%).#N#/#N#copayment#N#An amount you may be required to pay as your share of the cost for a medical service or supply, like a doctor's visit, hospital outpatient visit, or prescription drug. A copayment is usually a set amount, rather than a percentage. For example, you might pay $10 or $20 for a doctor's visit or prescription drug.#N#) for covered services and supplies. There's no yearly limit for what you pay out-of-pocket. 2 You usually pay a monthly premium for Part B. 3 You generally don't need to file Medicare claims. The law requires providers and suppliers to file your claims for the covered services and supplies you get. Providers include doctors, hospitals, skilled nursing facilities, and home health agencies.
What is Medicare Advantage?
Medicare Advantage Plans may also offer prescription drug coverage that follows the same rules as Medicare drug plans. .
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. ) before Medicare pays its share. Then, Medicare pays its share, and you pay your share (. coinsurance.
What is a referral in health care?
referral. A written order from your primary care doctor for you to see a specialist or get certain medical services. In many Health Maintenance Organizations (HMOs), you need to get a referral before you can get medical care from anyone except your primary care doctor.
What is a coinsurance percentage?
Coinsurance is usually a percentage (for example, 20%). An amount you may be required to pay as your share of the cost for a medical service or supply, like a doctor's visit, hospital outpatient visit, or prescription drug. A copayment is usually a set amount, rather than a percentage.
Does Medicare cover assignment?
The type of health care you need and how often you need it. Whether you choose to get services or supplies Medicare doesn't cover. If you do, you pay all the costs unless you have other insurance that covers it.
Do you have to choose a primary care doctor for Medicare?
No, in Original Medicare you don't need to choose a. primary care doctor. The doctor you see first for most health problems. He or she makes sure you get the care you need to keep you healthy. He or she also may talk with other doctors and health care providers about your care and refer you to them.
What is Medicare Part A?
Medicare Part A covers some costs associated with inpatient hospital treatment, a skilled nursing facility, or hospice. Medicare Part B covers some costs associated with medically necessary outpatient services ...
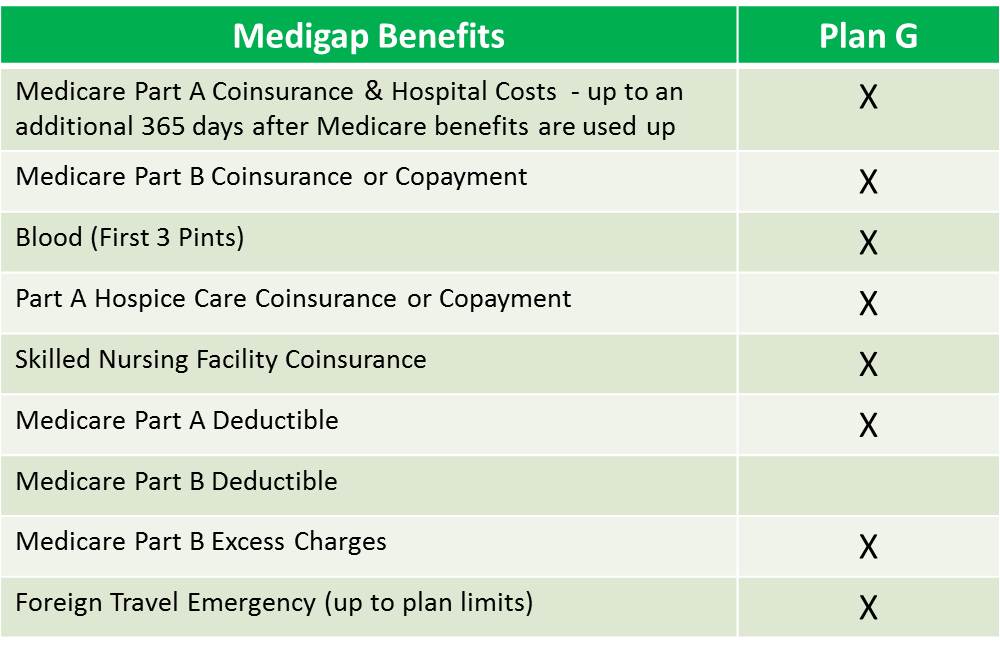
What are the benefits of Medicare Supplement?
These are the benefits that may be available with a Medicare Supplement plan: 1 Coverage for Part A hospital coinsurance costs for up to 365 days once Part A’s coverage is used up. 2 Part B copayments and coinsurance amounts. 3 Coverage for the first three pints of blood if required during treatment. 4 Hospice care share-of-cost obligations with Part A. 5 Coinsurance related to a stay in a skilled nursing facility. 6 Coverage for the deductibles for Part A or Part B. 7 Excess charges not covered by Part B. 8 Medical emergencies while traveling in a foreign country.
How long does Medigap coverage last?
This waiting period may last for up to 6 months.
How long does Medicare Supplement cover hospital coinsurance?
These are the benefits that may be available with a Medicare Supplement plan: Coverage for Part A hospital coinsurance costs for up to 365 days once Part A’s coverage is used up. Part B copayments and coinsurance amounts. Coverage for the first three pints of blood if required during treatment.
How long does it take to enroll in Medigap?
The initial enrollment period for a Medigap plan begins the month a recipient turns 65 and is enrolled in Part B. Recipients have a 6-month period to purchase any Medigap plan available in their state.
Which states have supplemental Medicare plans?
Some states, such as Massachusetts, Minnesota and Wisconsin, may label and regulate their supplemental plans differently. Nationally, Medicare laws can also change and that can have an impact on which Medigap plans are still valid and which may be phased out.
Does Medicare Part A cover coinsurance?
Although Medicare Part A and Part B can help cover many expenses, recipients are still obligated to pay deductibles, copayments and coinsurance amounts. A Medigap plan can help alleviate the burden of some of the costs of deductibles, coinsurance, copayment, and medical care outside of the United States. There are a variety of policies that offer ...
What is Medicare Supplement?
Medicare supplement insurance policies help fill in the gaps left by Original Medicare health care insurance. For many people, Medicare Supplement, also known as Medigap, insurance helps them economically by paying some of the out-of-pocket costs associated with Original Medicare.
How long does Medicare cover travel?
Each plan varies in what it covers, but all plans pay for Medicare Part A (hospital insurance) coinsurances for up to 365 days beyond the coverage that Medicare offers. Some of the plans cover a percentage of the cost for emergency health care while traveling abroad.
What percentage of Medicare supplement is paid?
After this is paid, your supplement policy pays your portion of the remaining cost. This is generally 20 percent. Some policies pay your deductibles The deductible is a set amount which you must pay before Medicare begins covering your health care costs.
How many people does Medicare Supplement cover?
Keep in mind that, just like Medicare, Medicare Supplement plans are individual insurance policies. They only cover one person per plan. If you want coverage for your spouse, you must purchase a separate plan.
How long does it take to get a Medigap plan?
When you turn 65 and enroll in Part B, you will have a 6-month Initial Enrollment Period to purchase any Medigap plan sold in your state. During this time, you have a “guaranteed issue right” to buy any plan available. They are required to accept you and cannot charge you more due to any pre-existing conditions.
How old do you have to be to qualify for medicare?
To be eligible for Medicare, you must be at least 65 years old, a citizen of the United States or permanent legal resident for at least five consecutive years. Also, you, or your spouse, must have worked and paid federal taxes for at least ten years (or 40 quarters).
Does Medicare cover long term care?
Most plans do not cover long-term care, vision, dental, hearing care, or private nursing care. All Medicare Supplement insurance coverage comes with a monthly premium which you pay directly to your provider. How much you pay depends on which plan you have.