The federal government spent nearly $1.2 trillion on health care in fiscal year 2019. Of that, Medicare claimed roughly $644 billion, Medicaid and the Childrens Health Insurance Pro-gram about $427 billion, and veterans medical care about $80 billion.
Full Answer
What are annual expenditures for Medicaid?
- Older adults and people with physical disabilities
- People with intellectual and/or developmental disabilities
- People receiving behavioral health services
- Other or multiple populations
How much Medicaid and Medicare cost Americans?
This is why the CMS releases information about premiums and deductibles for different parts of Medicare every year to the general public. For 2022, the Part B standard monthly premium for Medicare is $170.10 (up from $148.50 in 2021), and the annual deductible is $233 (up from $203 in 2021).
How much does Medicare cost per person?
That's $11,582 per person. This figure accounted for 17.7% of gross domestic product (GDP) that year. If we look at each program individually, Medicare spending grew 6.7% to $799.4 billion in 2019,...
How much Medicaid pays?
Key Takeaways
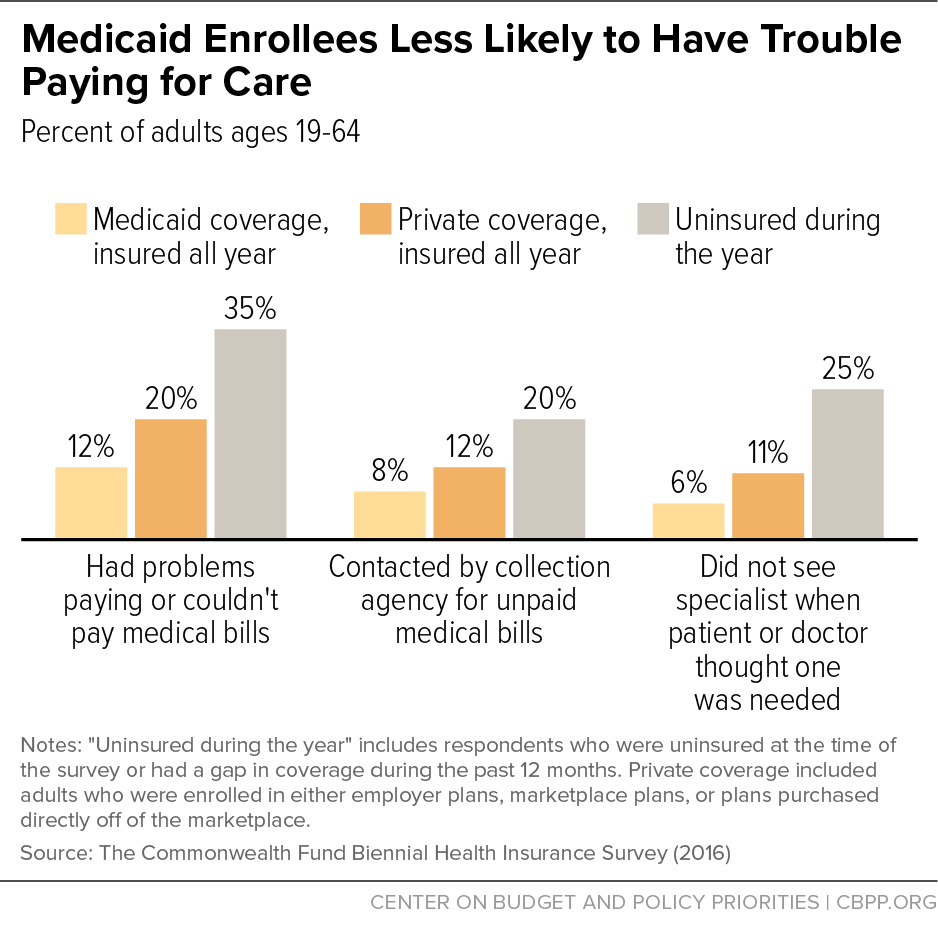
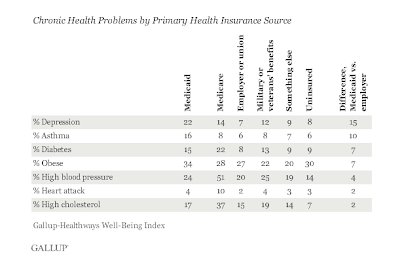
- Both Medicare and Medicaid are government-sponsored health insurance plans.
- Medicare is federally administered and covers older or disabled Americans, while Medicaid operates at the state level and covers low-income families and some single adults.
- Funding for Medicare is done through payroll taxes and premiums paid by recipients.
How much does Medicare cost each year?
2022If your yearly income in 2020 (for what you pay in 2022) wasYou pay each month (in 2022)File individual tax returnFile joint tax return$91,000 or less$182,000 or less$170.10above $91,000 up to $114,000above $182,000 up to $228,000$238.10above $114,000 up to $142,000above $228,000 up to $284,000$340.203 more rows
What is the monthly cost for Medicare 2021?
$148.50 forThe standard monthly premium for Medicare Part B enrollees will be $148.50 for 2021, an increase of $3.90 from $144.60 in 2020. The annual deductible for all Medicare Part B beneficiaries is $203 in 2021, an increase of $5 from the annual deductible of $198 in 2020.
What is the average monthly cost for Medicare?
How much does Medicare cost?Medicare planTypical monthly costPart B (medical)$170.10Part C (bundle)$33Part D (prescriptions)$42Medicare Supplement$1631 more row•Mar 18, 2022
What is the cost of Medicare in 2020?
$144.60The Centers for Medicare & Medicaid Services has announced that the standard monthly Part B premium will be $144.60 in 2020, an increase from $135.50 in 2019. However, some Medicare beneficiaries will pay less than this amount.
Is Medicare Part A and B free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
Is Medicare premium based on income?
Medicare premiums are based on your modified adjusted gross income, or MAGI. That's your total adjusted gross income plus tax-exempt interest, as gleaned from the most recent tax data Social Security has from the IRS.
How much does Medicare cost at age 62?
Reaching age 62 can affect your spouse's Medicare premiums He can still receive Medicare Part A, but he will have to pay a monthly premium for it. In 2020, the Medicare Part A premium can be as high as $458 per month.
What is the cheapest Medicare plan?
Plan K is the cheapest Medigap plan, with an average cost of $77 per month for 2022. For those who are only interested in protecting themselves against major medical expenses, a high-deductible plan is another way to have low-cost coverage.
Is Medicare Part A free at age 65?
You are eligible for premium-free Part A if you are age 65 or older and you or your spouse worked and paid Medicare taxes for at least 10 years. You can get Part A at age 65 without having to pay premiums if: You are receiving retirement benefits from Social Security or the Railroad Retirement Board.
How much comes out of your Social Security check for Medicare?
Medicare Part B (medical insurance) premiums are normally deducted from any Social Security or RRB benefits you receive. Your Part B premiums will be automatically deducted from your total benefit check in this case. You'll typically pay the standard Part B premium, which is $170.10 in 2022.
What is the cost of Medicare Part B for 2022?
$170.10The standard Part B premium amount in 2022 is $170.10. Most people pay the standard Part B premium amount. If your modified adjusted gross income as reported on your IRS tax return from 2 years ago is above a certain amount, you'll pay the standard premium amount and an Income Related Monthly Adjustment Amount (IRMAA).
How much are Social Security premiums?
Monthly Medicare Premiums for 2022Modified Adjusted Gross Income (MAGI)Part B monthly premium amountPrescription drug coverage monthly premium amountIndividuals with a MAGI above $114,000 up to $142,000 Married couples with a MAGI above $228,000 up to $284,000Standard premium + $170.10Your plan premium + $32.105 more rows
How much do you pay for Medicare after you pay your deductible?
You’ll usually pay 20% of the cost for each Medicare-covered service or item after you’ve paid your deductible.
How much will Medicare premiums be in 2021?
If you don’t qualify for a premium-free Part A, you might be able to buy it. In 2021, the premium is either $259 or $471 each month, depending on how long you or your spouse worked and paid Medicare taxes.
How often do you pay premiums on a health insurance plan?
Monthly premiums vary based on which plan you join. The amount can change each year. You may also have to pay an extra amount each month based on your income.
How often do premiums change on a 401(k)?
Monthly premiums vary based on which plan you join. The amount can change each year.
Do you have to pay Part B premiums?
You must keep paying your Part B premium to keep your supplement insurance.
What is managed care expenditure?
Managed care expenditures cover the same services that are delivered via fee-for-service. Data do not permit allocation of managed care expenditures to the different service categories.
Who funds Medicaid and CHIP?
The federal government and states jointly fund and administer Medicaid and the Children’s Health Insurance Program (CHIP). The following data present a snapshot of recent annual expenditure statistics, such as expenditures by service category and state.
How much will Medicare cost in 2021?
Most people don't pay a monthly premium for Part A (sometimes called " premium-free Part A "). If you buy Part A, you'll pay up to $471 each month in 2021. If you paid Medicare taxes for less than 30 quarters, the standard Part A premium is $471. If you paid Medicare taxes for 30-39 quarters, the standard Part A premium is $259.
How much does Medicare pay for outpatient therapy?
After your deductible is met, you typically pay 20% of the Medicare-approved amount for most doctor services (including most doctor services while you're a hospital inpatient), outpatient therapy, and Durable Medical Equipment (DME) Part C premium. The Part C monthly Premium varies by plan.
How long does a SNF benefit last?
The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row. If you go into a hospital or a SNF after one benefit period has ended, a new benefit period begins. You must pay the inpatient hospital deductible for each benefit period. There's no limit to the number of benefit periods.
How much is the Part B premium for 91?
Part B premium. The standard Part B premium amount is $148.50 (or higher depending on your income). Part B deductible and coinsurance.
What is Medicare Advantage Plan?
A Medicare Advantage Plan (Part C) (like an HMO or PPO) or another Medicare health plan that offers Medicare prescription drug coverage. Creditable prescription drug coverage. In general, you'll have to pay this penalty for as long as you have a Medicare drug plan.
How much is coinsurance for days 91 and beyond?
Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime). Beyond Lifetime reserve days : All costs. Note. You pay for private-duty nursing, a television, or a phone in your room.
What is periodic payment?
The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage.
What is Medicaid spend down?
These states are sometimes referred to as “spend down” states and allow Medicaid applicants to spend their “excess” income on medical expenses until they reach the medically needy income limit. Once they have done so, they are income eligible for the remainder of the spend down period.
What is long term care Medicaid?
Long term care Medicaid, however, is intended for persons who have limited financial means (low income and assets). That said, beneficiaries may have to contribute the majority of their income towards the cost of their care. (State-by-state financial eligibility criteria can be found here ).
Do nursing home recipients have to contribute to Medicaid?
It’s important to mention that Medicaid nursing home recipients must contribute the majority of their income towards the cost of their nursing home care. Stated differently, even when the income limit is met, they are not able to retain monthly income up to this level.
Who manages a Medicaid trust?
A trustee (someone other than the Medicaid applicant) is named to manage the trust and the income deposited into the trust can only be used for very limited reasons. For example, it may go towards the cost of the Medicaid beneficiary’s long term care.
Is Medicaid denial automatic?
Being over Medicaid’s income limit (approximately $2,349 / month in 2020 for nursing home Medicaid and home and community based services via a Medicaid waiver) is not automatic cause for Medicaid denial.
How much did Medicare spend?
Medicare spending increased 6.4% to $750.2 billion, which is 21% of the total national health expenditure. The rise in Medicaid spending was 3% to $597.4 billion, which equates to 16% of total national health expenditure.
What percentage of Medicare is paid to MA?
Based on a federal annual report, KFF performed an analysis to reveal the proportion of expenditure for Original Medicare, Medicare Advantage (MA) and Part D (drug coverage) from 2008 to 2018. A graphic depiction on the KFF website illustrates the change in spending of Medicare options. Part D benefit payments, which include stand-alone and MA drug plans, grew from 11% to 13% of total expenditure. Payments to MA plans for parts A and B went from 21% to 32%. During the same time period, the percentage of traditional Medicare payments decreased from 68% to 55%.
What is the agency that administers Medicare?
To grasp the magnitude of the government expenditure for Medicare benefits, following are 2018 statistics from the Centers for Medicare & Medicaid Services (CMS), which is the agency that administers Medicare:
What is the largest share of health spending?
The biggest share of total health spending was sponsored by the federal government (28.3%) and households (28.4%) while state and local governments accounted for 16.5%. For 2018 to 2027, the average yearly spending growth in Medicare (7.4%) is projected to exceed that of Medicaid and private health insurance.
Is Medicare a concern?
With the aging population, there is concern about Medicare costs. Then again, the cost of healthcare for the uninsured is a prime topic for discussion as well.
Does Medicare pay payroll taxes?
Additionally, Medicare recipients have seen their share of payroll taxes for Medicare deducted from their paychecks throughout their working years.
How much does Medicare cost?
If you’re eligible for Medicare, but not other federal benefits, you’ll pay a Part A premium of $259 or $471 each month , depending on how long you’ve paid Medicare taxes.
How much does Medicare pay for inpatient care?
Here’s how much you’ll pay for inpatient hospital care with Medicare Part A: Days 1-60 : $0 per day each benefit period, after paying your deductible. Days 61-90 : $371 per day each benefit period. Day 91 and beyond : $742 for each "lifetime reserve day" after benefit period. You get a total of 60 lifetime reserve days until you die.
How do I make my Medicare payments?
If you’re on federal retirement benefits, your Medicare Part B premiums get deducted from your Social Security checks. You can elect to get your Medicare Part D premiums deducted from your benefit checks , too. Contact your insurer.
How much does Medicare Part A cost in 2022?
Premiums for Medicare Part A are $0 if you’re getting or are eligible for federal retirement benefits. It’s also premium-free if you’re under 65 and receiving Social Security disability benefits for 24 months, or are diagnosed with end-stage kidney disease. If you’re eligible for Medicare, but not other federal benefits, you’ll pay a Part A premium of $274 or $499 each month, depending on how long you’ve paid Medicare taxes.
What is the coinsurance amount for Medicare Part B?
The Medicare Part B coinsurance amount is 20% for covered supplies and services.
How much can you spend on Medicare Part C?
After that limit, your Medicare Part C plan will pick up all the remaining cost of covered health care services. The out-of-pocket limit for Medicare Advantage can’t exceed $7,550 a year for in-network services. That means you could save more money if you have a lower out-of-pocket expenses limit. The limit is $11,300 for out-of-network services.
What are the out-of-pocket expenses of Medicare?
Medicare costs. Beneficiaries face the same three major out-of-pocket expenses associated with any health insurance plan, which include: Premiums : The monthly payment just to have the plan. Deductible : The amount you must pay on your own before insurance starts to cover the costs.
When was the Medicaid and CHIP scorecard released?
This version of the Medicaid and CHIP Scorecard was released in October 2020. To view the version of the Medicaid and CHIP Scorecard that was published in November 2019, please visit the archived Scorecard page.
What is a monthly beneficiary payment?
Monthly beneficiary payments are all monthly payments reported in the TAF Other claims file (OT) which would be claims with claim type = 2: Medicaid or Medicaid-Expansion Capitated Payment. They include: capitated payments to HMOs, HIOs, or PACE plans; capitated payments for primary care case management (PCCM); premium payments for private health insurance; and capitated payments to prepaid health plans (PHPs).
What data sources does CMS use?
To conduct this analysis, CMS used two data sources: (1) MBES expenditure data and (2) T-MSIS data. MBES expenditure data (reported by states on CMS-64 forms) are at the state level and do not include expenditures at the enrollee or at the eligibility group levels; therefore CMS used T-MSIS data to classify enrollees, allocate expenditures into eligibility groups, and construct the denominator (number of enrollee years) for each eligibility group.
What is the minimum claim volume required for CMS?
To ensure CMS based spending estimates on a comparatively complete set of claims, claims volume must have been at least 20 percent of the national median of claims per 1,000 enrollee months for each claim type.
Is per capita expenditure the same as 2019 scorecard?
The approach used to calculate the per capita expenditure estimates is almost entirely the same as that used in the 2019 Scorecard. One notable exception is how we distributed certain CMS-64 expenditures not typically reported to T-MSIS. In addition, we modified how we identified capitation and monthly payments to be more inclusive. Per capita expenditures for 2017 in this version of the Scorecard will differ from 2017 values displayed in the 2019 Scorecard because the data have been updated and because the per capita expenditures methodology has changed. See the methodology document for further details.
How much does Medicare Advantage cost per month?
In 2021, the average monthly premium for Medicare Advantage plans with prescription drug coverage is $33.57 per month. 1
What is the average cost of Medicare Supplement Insurance (Medigap)?
The average premium paid for a Medicare Supplement Insurance (Medigap) plan in 2019 was $125.93 per month. 3
What will Medicare Part A cost in 2021?
Medicare Part A is hospital insurance. It covers some of your costs when you are admitted for inpatient care at a hospital, skilled nursing facility and some other types of inpatient facilities.
What is the average cost of Medicare Part D prescription drug plans?
In 2021, the average monthly premium for a Medicare Part D plan is $41.64 per month. 1
How much is Medicare Part A deductible for 2021?
The Part A deductible is $1,484 per benefit period in 2021.
What is Medicare Part B?
Medicare Part B covers medical insurance benefits and includes monthly premiums, an annual deductible, coinsurance and other potential costs.
How much is respite care in 2021?
You might also be charged a 5 percent coinsurance for inpatient respite care costs. Medicare Part A requires a coinsurance payment of $185.50 per day in 2021 for inpatient skilled nursing facility stays longer than 20 days. You are responsible for all costs after day 101 of an inpatient skilled nursing facility stay.
What are the expenses that go away when you receive Medicaid at home?
When persons receive Medicaid services at home or “in the community” meaning not in a nursing home through a Medicaid waiver, they still have expenses that must be paid. Rent, mortgages, food and utilities are all expenses that go away when one is in a nursing home but persist when one receives Medicaid at home.
How long does it take to get a medicaid test?
A free, non-binding Medicaid eligibility test is available here. This test takes approximately 3 minutes to complete. Readers should be aware the maximum income limits change dependent on the marital status of the applicant, whether a spouse is also applying for Medicaid and the type of Medicaid for which they are applying.
Is income the only eligibility factor for Medicaid?
Medicaid Eligibility Income Chart by State – Updated Mar. 2021. The table below shows Medicaid’s monthly income limits by state for seniors. However, income is not the only eligibility factor for Medicaid long term care, there are asset limits and level of care requirements.
Can you qualify for medicaid if you exceed your income limit?
Exceeding the income limits does not mean an individual cannot qualify for Medicaid. Most states have multiple pathways to Medicaid eligibility. Furthermore, many states allow the use of Miller Trusts or Qualified Income Trusts to help person who cannot afford their care costs to become Medicaid eligible. There are also Medicaid planning professionals that employ other complicated techniques to help person become eligible. Finally, candidates can take advantage of spousal protection law that allow income (or assets) to be allocated to a non-applicant spouse.