After you meet the Medicare Part B deductible (which is $203 per year in 2021), you are typically responsible for paying 20 percent of the Medicare-approved amount for the rehab services. There is no limit as to how long Medicare Part B will cover these outpatient rehab services, as long as the rehab is considered medically necessary by your primary health care provider.
Full Answer
How many days will Medicare pay for rehab?
Days 1-60: $1,556 deductible.*. Days 61-90: $389 coinsurance each day. Days 91 and beyond: $778 coinsurance per each “lifetime reserve day” after day 90 for each benefit period (up to a maximum of 60 reserve days over your lifetime). Each day after the lifetime reserve days: All costs. *You don’t have to pay a deductible for inpatient rehabilitation care if you were already …
How long does Medicare cover inpatient rehab?
· The costs for a rehab stay in a skilled nursing facility are as follows: You usually pay nothing for days 1–20 in one benefit period, after the Part A deductible is met. You pay a per-day charge set by Medicare for days 21–100 in a benefit period. You pay 100 percent of the cost for day 101 and beyond in a benefit period.
Does Medicare cover rehab cost?
Medicare reimburses a portion of the cost of inpatient rehabilitation treatments on a sliding scale basis. After you have met your deductible, Medicare can cover 100 percent of the cost of your first 60 days of care. After that, you will be charged a $341 co-payment for each day of treatment for the next 30 days.
When does Medicare cover rehab?
· These types of rehab are typically covered by Medicare Part B. After you meet the Medicare Part B deductible (which is $233 per year in 2022), you are typically responsible for paying 20 percent of the Medicare-approved amount for the rehab services.

How long does Medicare cover inpatient rehab?
Medicare covers inpatient rehab in a skilled nursing facility – also known as an SNF – for up to 100 days. Rehab in an SNF may be needed after an injury or procedure, like a hip or knee replacement.
How long does it take to get Medicare to cover rehab?
The 3-day rule for Medicare requires that you are admitted to the hospital as an inpatient for at least 3 days for rehab in a skilled nursing facility to be covered. You must be officially admitted to the hospital by a doctor’s order to even be considered an inpatient, so watch out for this rule. In cases where the 3-day rule is not met, Medicare ...
What is the medical condition that requires rehab?
To qualify for care in an inpatient rehabilitation facility, your doctor must state that your medical condition requires the following: Intensive rehabilitation. Continued medical supervision.
What is an inpatient rehab facility?
An inpatient rehabilitation facility (inpatient “rehab” facility or IRF) Acute care rehabilitation center. Rehabilitation hospital. For inpatient rehab care to be covered, your doctor needs to affirm the following are true for your medical condition: 1. It requires intensive rehab.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
How many reserve days can you use for Medicare?
You may use up to 60 lifetime reserve days at a per-day charge set by Medicare for days 91–150 in a benefit period. You pay 100 percent of the cost for day 150 and beyond in a benefit period. Your inpatient rehab coverage and costs may be different with a Medicare Advantage plan, and some costs may be covered if you have a Medicare supplement plan. ...
How long do you pay nothing for Medicare?
You usually pay nothing for days 1–60 in one benefit period, after the Part A deductible is met.
How long does rehab last in a skilled nursing facility?
When you enter a skilled nursing facility, your stay (including any rehab services) will typically be covered in full for the first 20 days of each benefit period (after you meet your Medicare Part A deductible). Days 21 to 100 of your stay will require a coinsurance ...
How long does Medicare cover skilled nursing?
Medicare Part A covers 100 days in a skilled nursing facility with some coinsurance costs. After day 100 of an inpatient SNF stay, you are responsible for all costs.
How many reserve days do you have to have to be in the hospital?
You have a total of 60 lifetime reserve days. Once you have exhausted all of your lifetime reserve days, you will be responsible for all hospital costs for any stay longer than 90 days.
How much is coinsurance for inpatient care in 2021?
If you continue receiving inpatient care after 60 days, you will be responsible for a coinsurance payment of $371 per day (in 2021) until day 90. Beginning on day 91, you will begin to tap into your “lifetime reserve days,” for which a daily coinsurance of $742 is required in 2021. You have a total of 60 lifetime reserve days.
What is Medicare Advantage?
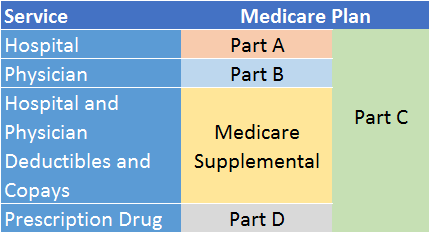
Medicare Advantage (Medicare Part C) and Medicare Part D can each provide coverage for prescription medication related to treatment for drug or alcohol dependency. Coverage will depend on your individual plan.
Does Medicare Part B cover outpatient therapy?
Medicare Part B may cover outpatient treatment services as part of a partial hospitalization program (PHP), if your doctor certifies that you need at least 20 hours of therapeutic services per week. Part B may also cover outpatient substance abuse counseling sessions performed by a doctor, clinical psychologist, nurse practitioner or clinical social worker.
How much is Medicare Part A deductible for 2021?
In 2021, the Medicare Part A deductible is $1,484 per benefit period. A benefit period begins the day you are admitted to the hospital. Once you have reached the deductible, Medicare will then cover your stay in full for the first 60 days. You could potentially experience more than one benefit period in a year.
How long does Medicare rehab last?
Standard Medicare rehab benefits run out after 90 days per benefit period. If you recover sufficiently to go home, but you need rehab again in the next benefit period, the clock starts over again and your services are billed in the same way they were the first time you went into rehab. If your stay in rehab is continuous, ...
Who can help with Medicare rehab?
You can also plan your coverage with a certified Medicare benefits counselor or senior financial planner. These professionals can give you up-to-date information and help you plan your Medicare coverage for rehab.
Why do people go to rehab?
People go into rehab for many reasons. At a SNF, staff can monitor your condition and care for you 24 hours a day. Nursing staff may dispense your medication, while facility caregivers help you with personal care needs and other activities of daily living. You may have a doctor on site who can assist with your treatment. Many people receive physical, occupational and mental health therapy during their time in rehab, as well as prosthetic or orthopedic devices that can help them return to independent living after leaving the facility.
What is rehab in nursing?
Rehab is a form of inpatient care many seniors receive after a stay in the hospital. If your injury or illness requires close coordination between your doctor and caregivers, you might spend some time getting skilled nursing care to rehabilitate after your initial treatment. This care may be delivered in a standalone skilled nursing facility (SNF), or you might be transferred to a rehab unit at the hospital where you were initially treated.
How many days can you use for Medicare?
When you sign up for Medicare, you are given a maximum of 60 lifetime reserve days. You can apply these to days you spend in rehab over the 90-day limit per benefit period. These days are effectively a limited extension of your Part A benefits you can use if you need them, though they cannot be renewed and once used, they are permanently gone.
Can you get Medicare and Medicaid for rehab?
If you are dual-eligible for both Medicare and Medicaid, your rehab services will probably be billed first to Medicare, with any remaining costs transferred to Medicaid. You may still have to meet a deductible or share of cost before your Medicaid benefits can kick in, but these benefits will likely continue for as long as your rehab is deemed medically necessary.
Does Medicare Supplement cover out of pocket expenses?
A Medicare Supplement plan can pick up some or all of the deductible you would otherwise be charged, assist with some Part B expenses that apply to your treatment and potentially cover some additional out-of-pocket Medicare costs.
How much does it cost to get physical therapy in 2020?
In 2020, your provider must confirm your therapy is medically necessary once your total costs reach $2,080 for physical therapy, speech-language pathology or occupational therapy care. Original Medicare (Parts A & B) will continue to pay for up to 80 percent of the Medicare-approved amount once your care is confirmed as medically necessary. Your costs with a Medicare Advantage plan may be different, so ask your provider before seeking care.
What is the Medicare therapy cap?
The Medicare therapy cap was a set limit on how much Original Medicare would pay for outpatient therapy in a year. Once that limit was reached, you had to request additional coverage through an exception in order to continue getting covered services. However, by law, the therapy cap was removed entirely by 2019.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
What is an ABN for a physical therapist?
This is true for physical therapy, speech-language pathology and occupational therapy. This notice is called an Advance Beneficiary Notice of Noncoverage (ABN). If your provider gives you an ABN, you may agree to pay for the services that aren’t medically necessary. However, Medicare will not help cover the cost.
Does Medicare Advantage cover rehab?
Your costs for Medicare rehab coverage with a Medicare Advantage plan (Part C) depend on the specific plan you have. Medicare Advantage plans are offered by private insurance companies and approved by Medicare. These plans must provide coverage at least as good as what’s provided by Original Medicare (Parts A & B).
What is Medicare Part B?
Occupational therapy. Speech-language pathology services. Medicare Part B pays 80 percent of the Medicare-approved amount for outpatient therapy services received from a provider who accepts Medicare assignment. You are responsible for 20 percent of the cost ...
Does Medicare pay for outpatient therapy?
Technically, no. There is no limit on what Medicare will pay for outpatient therapy, but after your total costs reach a certain amount, your provider must confirm that your therapy is medically necessary in order for Medicare to cover it.1.
How long does Medicare require for rehabilitation?
In some situations, Medicare requires a 3-day hospital stay before covering rehabilitation. Medicare Advantage plans also cover inpatient rehabilitation, but the coverage guidelines and costs vary by plan. Recovery from some injuries, illnesses, and surgeries can require a period of closely supervised rehabilitation.
How long do you have to pay a deductible for rehab?
Days 1 through 60. You’ll be responsible for a $1,364 deductible. If you transfer to the rehab facility immediately after your hospital stay and meet your deductible there, you won’t have to pay a second deductible because you’ll still be in a single benefit period. The same is true if you’re admitted to a rehab facility within 60 days of your hospital stay.
How much is coinsurance for days 61 through 90?
Days 61 through 90. During this period, you’ll owe a daily coinsurance amount of $341.
How to contact Medicare directly?
If you want to confirm you’re following Medicare procedures to the letter, you can contact Medicare directly at 800-MEDICARE (800-633-4227 or TTY: 877-486-2048) .
Is hip replacement considered inpatient only?
In 2020, Medicare also removed total hip replacements from the list. The 3-day rule now applies to both of those procedures. If you have a Medicare Advantage plan, talk with your insurance provider to find out if your surgery is considered an inpatient-only procedure.
Does Medicare cover knee replacement surgery?
The 3-day rule does not apply for these procedures, and Medicare will cover your inpatient rehabilitation after the surgery. These procedures can be found on Medicare’s inpatient only list. In 2018, Medicare removed total knee replacements from the inpatient only list.
How long does it take for a skilled nursing facility to be approved by Medicare?
Confirm your initial hospital stay meets the 3-day rule. Medicare covers inpatient rehabilitation care in a skilled nursing facility only after a 3-day inpatient stay at a Medicare-approved hospital. It’s important that your doctor write an order admitting you to the hospital.
How much does nursing home care cost?
Nursing home care can cost tens of thousands of dollars per year for basic care, but some nursing homes that provide intensive care can easily cost over $100,000 per year or more. How Much Does Medicare Pay for Nursing Home Care?
How long does Medicare cover nursing home care?
If you have Original Medicare, you are fully covered for a stay up to 20 days. After the 20th day, you will be responsible for a co-insurance payment for each day at a rate of $176 per day. Once you have reached 100 days, the cost of care for each day after is your responsibility and Medicare provides no coverage.
Do skilled nursing facilities have to be approved by Medicare?
In order to qualify for coverage in a skilled nursing facility, the stay must be medically necessary and ordered by a doctor. The facility will also need to be a qualified Medicare provider that has been approved by the program.
Do you have to have Medicare to be a skilled nursing facility?
In addition, you must have Medicare Part A coverage to receive care in a residential medical facility. The facility must qualify as a skilled nursing facility, meaning once again that traditional residential nursing homes are not covered.
Is Medicare good or bad for seniors?
For seniors and qualifying individuals with Medicare benefits, there’s some good news and some bad news. While Medicare benefits do help recipients with the cost of routine doctor visits, hospital bills and prescription drugs, the program is limited in its coverage of nursing home care.
Can Medicare recipients get discounts on at home care?
At-Home Care as an Alternative. Some Medicare recipients may also qualify for discounts on at-home care provided by a nursing service. These providers often allow seniors to stay in their own homes while still receiving routine monitoring and basic care from a nurse who visits on a schedule.