Full Answer
How much does Medicare pay for diabetic supplies?
supplies. 20% of the Medicare-approved amount after the yearly Part B deductible Diabetes supplies See page 16. Part D covers certain medical supplies to administer insulin (like syringes, needles, alcohol swabs, gauze, and inhaled insulin devices). Coinsurance or copayment Part D deductible may also apply
What diabetic supplies are covered by Original Medicare?
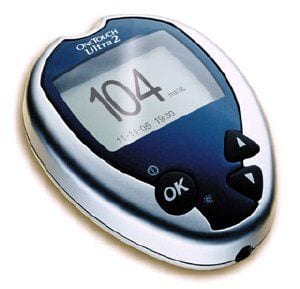
That’s why diabetic supplies are covered by Medicare. Medicare Part B. Part B coverage for diabetes supplies includes: Two diabetes screening tests per year; One glaucoma test per year; A home blood sugar monitor; Blood sugar test strips; Lancet devices; Lancets; Glucose control solutions that will check the accuracy of your test strips; Insulin pumps
How do I get my diabetic supplies through Medicare?
- A National Effort to Prevent Type 2 Diabetes: Participant-Level Evaluation of CDC’s National Diabetes Prevention Program
- Free Diabetes Supplies Available Tomorrow in Houston and Corpus Christi, Plus Extended Hours at 1-800-DIABETES Call Center Through Next Week
- Work to Do Before Medicare's Diabetes Prevention Program Is Set in Place
How to get Medicare covered diabetic supplies?
Medicare Part B covers many management supplies and preventive services including:
- Self-testing supplies like blood glucose test strips, lancets, and continuous glucose monitors (CGMs)
- Insulin pumps and insulin used with the pump
- Preventive diabetes screenings to test blood sugar levels up to twice a year
- Training and education on managing diabetes (find a certified educator)
How many diabetic test strips will Medicare pay for?
If you don't use insulin, you may be able to get 100 test strips and 100 lancets every 3 months. If your doctor says it's medically necessary, and if other qualifications and documentation requirements are met, Medicare will allow you to get additional test strips and lancets.
What diabetic supplies Does Part B cover?
In 2021, a person with Medicare Part B will pay 20% of the cost for diabetes self-management supplies such as glucose monitors, lancets, and test strips. However, to ensure Medicare coverage, they must get the prescription from their doctor and use an in-network pharmacy or supplier.
Are lancets covered by Medicare?
Note: Medicare won't pay for any supplies you didn't ask for, or for any supplies that were sent to you automatically from suppliers, including blood sugar monitors, test strips, and lancets.
What brand of glucose meter does Medicare 2022 cover?
Beginning Feb. 28, 2022, those using a Medtronic CGM integrated with the company's MiniMed insulin pumps will be able to get Medicare coverage for their transmitters, sensors and supplies.
Does Medicare pay for lancets and test strips?
If your doctor says it's medically necessary, Medicare will cover additional test strips and lancets. Test strips can be used to help monitor certain substances in the blood.
Is metformin covered by Medicare?
Yes. 100% of Medicare prescription drug plans cover this drug.
Does Medicare pay for glucose strips?
Medicare Part B covers blood sugar test strips and some other diabetic supplies such as blood glucose self-testing equipment and supplies, therapeutic shoes and inserts, and insulin pumps and the insulin for the pumps. These items are covered for people with diabetes whether or not they take insulin.
How do I get free diabetes testing supplies?
One of the easiest ways to get a free blood glucose meter is to contact the manufacturer directly. The majority of manufacturers offer free glucose monitors as a way to entice patients to purchase other brand-name supplies, such as glucose test strips, through the manufacturer. Contour, for example, offers free meters.
Are insulin pen needles covered by Medicare?
The amount you must pay for health care or prescriptions before Original Medicare, your Medicare Advantage Plan, your Medicare drug plan, or your other insurance begins to pay. ). You pay 100% for syringes, needles, alcohol swabs, and gauze, unless you have Part D.
What is the most accurate glucose meter in 2021?
Best overall: Contour Next. If you are looking for a glucose meter with the highest accuracy, Contour Next has shown 100% compliance in accuracy testing. Home glucose meters should show consistently accurate results because they are meant to monitor your glucose between doctor's visits.
Does Medicare cover A1c test?
Hemoglobin A1c Tests: Your doctor might order a hemoglobin A1c lab test. This test measures how well your blood glucose has been controlled over the past 3 months. Medicare may cover this test for anyone with diabetes if it is ordered by his or her doctor.
Are One Touch test strips covered by Medicare?
#1 Brand used by Medicare patients OneTouch® test strips are ALWAYS covered on Medicare Part B and $0 with most supplemental health plans. * With their red, white and blue Medicare Part B card alone, your patients pay just $1.66 for a box of 50ct test strips.
Does Medicare Cover Diabetes Supplies For Blood Glucose Testing?
Diabetic supplies for blood glucose monitoring are considered durable medical equipment (DME) under Medicare Part B. In order for your diabetes sup...
Is There Medicare Coverage For Insulin Pumps and Insulin-Related Diabetic Supplies?
If you meet certain medical conditions and your doctor believes an external insulin pump is medically necessary to treat your diabetes, Medicare ma...
Will Medicare Cover My Diabetic Shoes and Inserts?
If you have certain medical conditions related to your diabetes, such as severe diabetic foot disease, Part B might cover one pair of depth-inlay o...
Does Medicare Cover Insulin Or Prescription Drugs to Treat My Diabetes?
Original Medicare generally doesn’t cover injectable insulin or prescription medications to treat diabetes. If you want help paying for injectable...
What supplies do you need to treat diabetes?
You may need the following supplies to help manage the disease: Glucose (blood sugar) testing monitors and test strips. Insulin.
What is Medicare Part D?
What Medicare Part D Can Do. Medicare Part D provides prescription drug coverage and may help you pay for some diabetes supplies. If you have Original Medicare, you may enroll in a stand-alone Prescription Drug Plan (PDP). Many Medicare recipients choose to get their benefits through a Medicare Advantage ...
What are the best ways to treat diabetes?
If you are diagnosed with diabetes, you and your physician will create a treatment plan designed to meet your specific needs. You may need the following supplies to help manage the disease: 1 Glucose (blood sugar) testing monitors and test strips 2 Insulin 3 Lancet devices and lancets 4 Blood sugar control solutions (to check the accuracy of the test strips and monitor) 5 Therapeutic shoes or inserts
What is covered by Part B?
Many of the diabetes supplies you will need are covered by Part B’s DME benefits, including: Glucose testing monitors. Blood sugar test strips. Lancets and lancet devices. Glucose control solutions.
Does Medicare cover insulin pumps?
If you use an external insulin pump, the pump may be covered under DME. Part B also covers the furnishing and fitting of either of these each calendar year: Medicare will also cover 2 additional pairs of inserts each calendar year for custom-molded shoes and 3 pairs of inserts each calendar year for extra-depth shoes.
Can you get Medicare for diabetes?
Treatment for diabetes can vary depending on the needs of each individual patient, but many people living with diabetes rely on medical supplies to test blood sugar levels, recognize symptoms, and treat the disease. If you are eligible for Medicare, you may get help paying for the diabetes supplies that can help you manage diabetes.
Does Medicare cover shoes?
One pair of extra-depth shoes. Medicare will also cover 2 additional pairs of inserts each calendar year for custom-molded shoes and 3 pairs of inserts each calendar year for extra-depth shoes. Medicare will cover shoe modifications instead of inserts. In order for Medicare to help cover these supplies, you will likely need to rent ...
How long can you have Medicare Part B?
If you’ve had Medicare Part B for longer than 12 months , you can get a yearly “Wellness” visit to develop or update a personalized prevention plan based on your current health and risk factors. This includes:
What is Part B for diabetes?
In addition to diabetes self-management training, Part B covers medical nutrition therapy services if you have diabetes or renal disease. To be eligible for these services, your fasting blood sugar has to meet certain criteria. Also, your doctor or other health care provider must prescribe these services for you.
What is diabetes self management training?
Diabetes self-management training helps you learn how to successfully manage your diabetes. Your doctor or other health care provider must prescribe this training for Part B to cover it.
Does Medicare cover diabetes?
This section provides information about Medicare drug coverage (Part D) for people with Medicare who have or are at risk for diabetes. To get Medicare drug coverage, you must join a Medicare drug plan. Medicare drug plans cover these diabetes drugs and supplies:
Does Part B cover insulin pumps?
Part B may cover insulin pumps worn outside the body (external), including the insulin used with the pump for some people with Part B who have diabetes and who meet certain conditions. Certain insulin pumps are considered durable medical equipment.
Does Medicare cover diabetic foot care?
Medicare may cover more frequent visits if you’ve had a non-traumatic ( not because of an injury ) amputation of all or part of your foot, or your feet have changed in appearance which may indicate you have serious foot disease. Remember, you should be under the care of your primary care doctor or diabetes specialist when getting foot care.
How many therapeutic shoes does Medicare cover?
Medicare Part B covers one pair of therapeutic shoes per year for people with severe diabetic foot disease. An in-network provider must confirm that they need these therapeutic shoes or inserts before allowing coverage.
What do doctors need to certify a diabetic?
A doctor must certify a person has diabetes and requires certain testing supplies, insulin, or other medical materials. The amount of supplies varies according to the beneficiary and their overall health.
What is the maximum copayment for insulin in 2021?
In 2021, Medicare launched a Part D Senior Savings Model, a plan to offer insulin at a maximum co-payment of $35 for a month’s supply. However, not all prescription drug plans are part of this model. Individuals can review what available plans offer using Medicare’s search tool.
How does diabetes affect the body?
Diabetes is a chronic health condition. It affects how a person’s body converts beverages and food into energy. In 2018, 10.5% of the United States population (34.2 million people) had diabetes. In this article, we discuss Medicare coverage for diabetes supplies and services, followed by details for separate services and supplies.
What is the Medicare Part B copayment?
For Medicare Part B, this comes to 20%. Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs.
What is the number to call for insulin pump?
For questions about Part B’s coverage of insulin and insulin pumps, a person can call 1-800-MEDICARE.
Does Medicare cover insulin?
Medicare also generally covers insulin services, including preventive services, under original Medicare Part B, which is medical insurance. Part B covers the following services: outpatient training for a person to learn how to manage their diabetes. an annual glaucoma test. a biannual foot exam.
What is Medicare Part D?
Medicare Part D plans are private plans that cover medications that treat diabetes, including insulin and supplies to inject insulin. You must be enrolled in original Medicare (parts A and B) to be eligible for Part D.
What are the parts of Medicare?
Medicare parts B, C, and D each covers different supplies, medications, and services needed to manage diabetes. Make sure you go to pharmacies or equipment providers that are enrolled in Medicare and accept the assignment prices set by Medicare.
How often do you need to take insulin test strips?
number of test strips and lancets you need (Part B typically pays for 100 strips and lancets every 3 months if you don’t use insulin) New prescriptions are needed each year from your doctor. If you need to monitor your blood sugar more often, your supply limits for each month will need to be increased.
What are the challenges of diabetics?
Older adults with diabetes face unique challenges. Trusted Source. including hypoglycemia, brain and nervous system problems, and social support issues that require special monitoring to manage risks. There are many types of diabetic supplies needed for preventive screening, monitoring, and managing the condition.
How many people have type 2 diabetes?
Type 2 diabetes is the most common form. Of the 30 million Americans with diabetes, 90 percent have type 2. Twenty–four million people 65 and older have prediabetes (higher than normal blood sugar concentrations).
What are the risk factors for diabetes?
Risk factors for diabetes can be different for each type, but family history, age, race, and environmental factors may all impact the condition.
What is the most common type of diabetes?
Diabetes is a metabolic condition that leads to high blood sugar levels. Most people who have diabetes have type 2 diabetes. According to the American Diabetes Association, around 14 million Americans 65 and older have diabetes, some who are undiagnosed.
What is Medicare Supplement Plan?
Enroll in a Medicare Supplement plan to limit your out-of-pocket costs from Original Medicare (Medicare Part A and Part B) Enroll in the Medicare Part D Prescription Drug plan that saves you the most money. Get a prescription from your doctor for your supplies.
What does Medicare Part B cover?
Medicare Part B (which is your outpatient coverage) covers about 80% of the costs of a variety of supplies that are used to treat diabetes. Part B will typically cover these services and supplies up to 80%, leaving you responsible for the other 20% as well as any deductibles or copays. In order to help with the expenses, ...
Does Medicare cover blood sugar monitors?
If you buy your supplies without a prescription, or from a seller that’s not authorized, Medicare won’t cover any of the costs. Medicare Part B covers the following supplies, if they are prescribed by your doctor following their guidelines: Glucose test strips. Blood sugar testing monitors.
Can you get prescriptions covered by Medicare?
In order to have your supplies covered by Medicare, you must have a prescription from your doctor, and receive the items over the counter from an authorized seller. The items must also be on Medicare’s approved list, otherwise they won’t be covered.
Do people have Medicare Supplement?
In order to help with the expenses, most people have a Medicare Supplement plan or a Medicare Advantage plan. It’s important to note that Medicare Supplement plans range in coverage, and they’ll all pay their portion as long as Medicare pays first.
Is diabetes expensive to manage?
Diabetes can be difficult and expensive to manage, and you may find the services that Medicare offers helpful. If you’d like to learn more about how to take advantage of the benefits Medicare provides, contact your healthcare provider for more information.
Does Medicare cover diabetic supplies?
The simple answer is yes; Medicare covers some diabetic supplies. It also provides coverage for services that can help you treat or prevent diabetes. How much you have to pay out-of-pocket depends on whether or not you have other insurance.
How much does Medicare pay for diabetes?
In general, Medicare pays 80% and you pay 20% of the Medicare-approved amount for diabetes supplies and services covered by Part B after the yearly deductible is met. Your percentage share of the cost is called coinsurance.
What supplies are covered by Medicare Part D?
Diabetes Supplies and Services Covered by Medicare Part D. Medications to manage blood glucose. Insulin taken by injection. Supplies for taking insulin by injection (syringes, needles, alcohol swabs and gauze) Inhaled insulin.
What does Medicare cover?
Medicare covers various diabetes medications, supplies and services to help treat diabetes and keep your blood glucose in a healthy range. Medicare Part B covers blood glucose testing and other supplies you may need plus some medical and education services. Medicare Part D covers diabetes medications and supplies for injecting or inhaling insulin.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
What does Medicare Advantage cover?
Medicare Advantage plans (Part C) cover diabetes supplies and services, too, and often additional services such as vision, dental and hearing care. The costs and items covered will depend on the specific plan you have.
Do you pay coinsurance for Part D?
You may pay a coinsurance amount or a copayment for items covered by Part D. What you pay depends on the terms of your specific Part D plan. Some services, such as medical nutrition therapy and A1C tests, may be provided at no additional cost to you.
Does Medicare cover insulin?
Medicare Part D covers diabetes medications and supplies for injecting or inhaling insulin. Here’s a rundown of the diabetes supplies and services that Medicare covers. Some require a prescription or recommendation from your doctor. Coverage limits may include the amount of some supplies you can get or how often some services are covered.
How much does Medicare cover?
If your doctors and suppliers are enrolled in and participate in Medicare, and if the supplies are considered medically necessary, Medicare typically covers 80% of the Medicare-approved amount, and you pay the remaining 20% (after you pay your yearly Part B deductible).
What is Medicare Supplement?
A Medicare Supplement (Medigap) plan can help cover these diabetes supplies costs.
What is Medicare Part B?
Therapeutic shoes or inserts. Medicare Part B also provides coverage for some services for people with diabetes: Training in diabetes self-management. Annual eye exams. Foot exams. Tests for Glaucoma.
Does Medicare cover insulin?
Medicare Part B will not cover insulin unless it is used in an insulin pump. Medicare Part B also does not cover certain medical supplies used to administer insulin such as syringes, needles, insulin pens, alcohol swabs or inhaled insulin devices. Medicare does not cover anti-diabetic drugs used to maintain blood sugar.
Does Medicare cover diabetic supplies?
If Medicare covers your diabetic supplies, you may face out-of-pocket costs such as deductibles, copays and coinsurance.
Does Medicare Part B cover coinsurance?
For example, each of the 10 standardized Medigap plans that are available in most states provide at least partial coverage for the Medicare Part B coinsurance or copayments you might face when you receive covered outpatient treatments and covered supplies.
What is CMS in healthcare?
The Centers for Medicare & Medicaid Services (CMS) has developed a variety of educational resources for use by health care professionals and their staff as part of a broad outreach campaign to promote awareness and increase utilization of preventive services covered by Medicare. For more information about coverage, coding, billing, and reimbursement of Medicare-covered preventive services and screenings, visit
Does Medicare cover therapeutic shoes?
If a beneficiary has Medicare Part B, has diabetes, and meets certain conditions (see below), Medicare will cover therapeutic shoes if they need them. The types of shoes that are covered each year include one of the following:
Does Medicare pay for insulin pumps?
In the Original Medicare Plan, the beneficiary pays 20 percent of the Medicare-approved amount after the yearly Part B deductible. Medicare will pay 80 percent of the cost of the insulin pump. Medicare will also pay for the insulin that is used with the insulin pump.