Does Medicare cover office visits?
This typically depends on the telemedicine company youre using or the healthcare providers preferences. Since March 6, 2020, Medicare has covered telehealth appointments for all Medicare beneficiaries for office, hospital visits and other services that typically take place in person.
How to find a Medicare office near you?
- Dial 1-800-MEDICARE. ...
- Ask the customer service agent who answers your call to help you determine the nearest Medicare office. ...
- Write the address and phone number of any offices you are interested in on a piece of paper. ...
How much is a doctor visit with Medicare?
Let’s say the Medicare-approved costs were $100 for the doctor visit and $900 for the MRI. Assuming that you’ve paid your Part B deductible, and that Part B covered 80% of these services, you’d still be left with some costs. In this scenario, you’d typically pay $20 for the doctor visit and $180 for the x-rays.
Will Medicare cover the costs of my doctor visits?
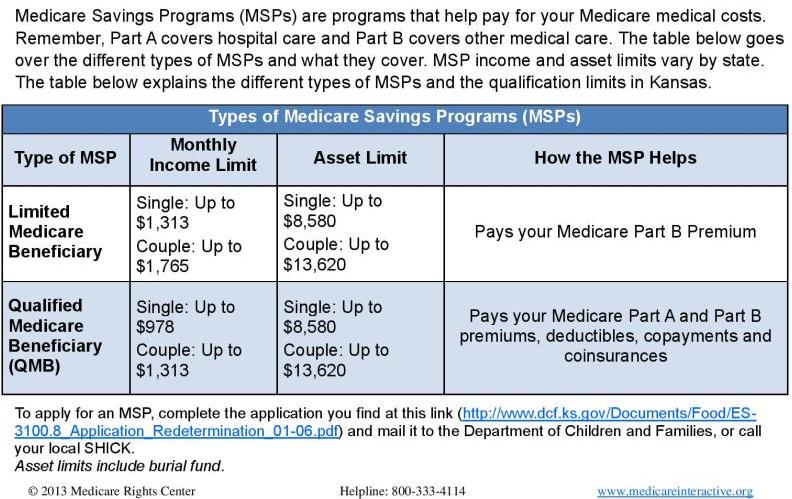
Medicare may cover doctor visits if certain conditions are met, but in some cases, you’ll have out-of-pocket costs, like deductibles and coinsurance amounts. No matter what kind of Medicare coverage you may have, it’s important to understand that your doctor must accept Medicare assignment.
What is the Medicare rate for an office visit?
For new patient visits most doctors will bill 99203 (low complexity) or 99204 (moderate complexity) These codes pay $122.69 and $184.52 respectively. So, if you see a new doctor and your medical case is moderately complex you could expect to pay almost $37 for that visit.
How Much Does Medicare pay for 99214 in 2021?
$132.94By Christine Frey posted 12-09-2020 15:122021 Final Physician Fee Schedule (CMS-1734-F)Payment Rates for Medicare Physician Services - Evaluation and Management99213Office/outpatient visit est$93.5199214Office/outpatient visit est$132.9499215Office/outpatient visit est$185.9815 more rows•Dec 9, 2020
What percentage of the allowable fee does Medicare pay a doctor?
80 percentUnder current law, when a patient sees a physician who is a “participating provider” and accepts assignment, as most do, Medicare pays 80 percent of the fee schedule amount and the patient is responsible for the remaining 20 percent.
What is Medicare reimbursement fee schedule?
A fee schedule is a complete listing of fees used by Medicare to pay doctors or other providers/suppliers. This comprehensive listing of fee maximums is used to reimburse a physician and/or other providers on a fee-for-service basis.
How does Medicare reimburse physician services?
In general, Medicare pays each of these providers separately, using payment rates and systems that are specific to each type of provider. The remaining share of Medicare benefit payments (37%) went to private plans under Part C (the Medicare Advantage program; 26%) and Part D (the Medicare drug benefit; 11%).
How much is reimbursement for 99213?
$43.2399213 Reimbursement Rates: – Medicaid:CPT CodeService TimeRate9921210 minutes$31.369921315 minutes$43.239921425 minutes$66.809921540 minutes$99.95
Does Medicare pay 100 percent of hospital bills?
According to the Centers for Medicare and Medicaid Services (CMS), more than 60 million people are covered by Medicare. Although Medicare covers most medically necessary inpatient and outpatient health expenses, Medicare reimbursement sometimes does not pay 100% of your medical costs.
Do doctors lose money on Medicare patients?
Summarizing, we do find corroborative evidence (admittedly based on physician self-reports) that both Medicare and Medicaid pay significantly less (e.g., 30-50 percent) than the physician's usual fee for office and inpatient visits as well as for surgical and diagnostic procedures.
What percentage does Medicare B pay?
Medicare Part B pays 80% of the cost for most outpatient care and services, and you pay 20%. For 2022, the standard monthly Part B premium is $170.10.
Is the 2021 Medicare fee schedule available?
The CY 2021 Medicare Physician Fee Schedule Final Rule was placed on display at the Federal Register on December 2, 2020. This final rule updates payment policies, payment rates, and other provisions for services furnished under the Medicare Physician Fee Schedule (PFS) on or after Jan. 1, 2021.
How much is Medicare reimbursement enhanced?
As a result, depending on physician performance within this program, Medicare reimbursements can be enhanced or penalized by up to 9%, although there is a two-year delay in this application (e.g. provider performance in 2021 will lead to the enhancement or penalty in 2023).
When will CMS change the physician fee schedule?
CMS has announced changes to the physician fee schedule for 2021. On December 2, 2020, the Centers for Medicare and Medicaid Services (CMS) published its final rules for the Part B fee schedule, referred to as the Physician Fee Schedule (PFS). Substantial changes were made, with some providers benefiting more than others, ...
When will the CPT code 99201 be revised?
On Nov. 1, 2019, CMS finalized revisions to the evaluation and management (E/M) office visit CPT codes 99201-99215. These revisions will go into effect on Jan. 1, 2021. They build on the goals of CMS and providers to reduce administrative burden and put “patients over paperwork” thereby improving the health system.
When will CMS update the E/M code?
These revisions build on the goals of CMS and the provider community to reduce administrative burden and put “patients over paperwork.” These revisions will be effective Jan. 1, 2021 .
Is telehealth included in CMS 2021?
In the 2021 Final Rule, CMS has included several Category 1 Telehealth Service additions as well as the addition of telehealth services, on an interim basis, to those services put in place during COVID-19.
How much is Medicare reimbursement for 2020?
Reimbursements match similar in-person services, increasing from about $14-$41 to about $60-$137, retroactive to March 1, 2020. In addition, Medicare is temporarily waiving the audio-video requirement for many telehealth services during the COVID-19 public health emergency. Codes that have audio-only waivers during the public health emergency are ...
What is the CPT code for Telehealth?
Medicare increased payments for certain evaluation and management visits provided by phone for the duration of the COVID-19 public health emergency: Telehealth CPT codes 99441 (5-10 minutes), 99442 (11-20 minutes), and 99443 (20-30 minutes)
Does Medicare cover telehealth?
Telehealth codes covered by Medicare. Medicare added over one hundred CPT and HCPCS codes to the telehealth services list for the duration of the COVID-19 public health emergency. Telehealth visits billed to Medicare are paid at the same Medicare Fee-for-Service (FFS) rate as an in-person visit during the COVID-19 public health emergency.