How much does Mavyret cost?
Sep 10, 2021 · For patients on Medicare Part D, the cost can range from $660.00 – 2,847.00 per month, based on your coverage phase. Patients with Low-Income Subsidy for Medicare will pay $8.95 per month. Compared to other approved oral HCV treatments, Mavyret tablets are priced very competitively and may be your lowest-cost option.
How much does Medicare Part D drug coverage cost?
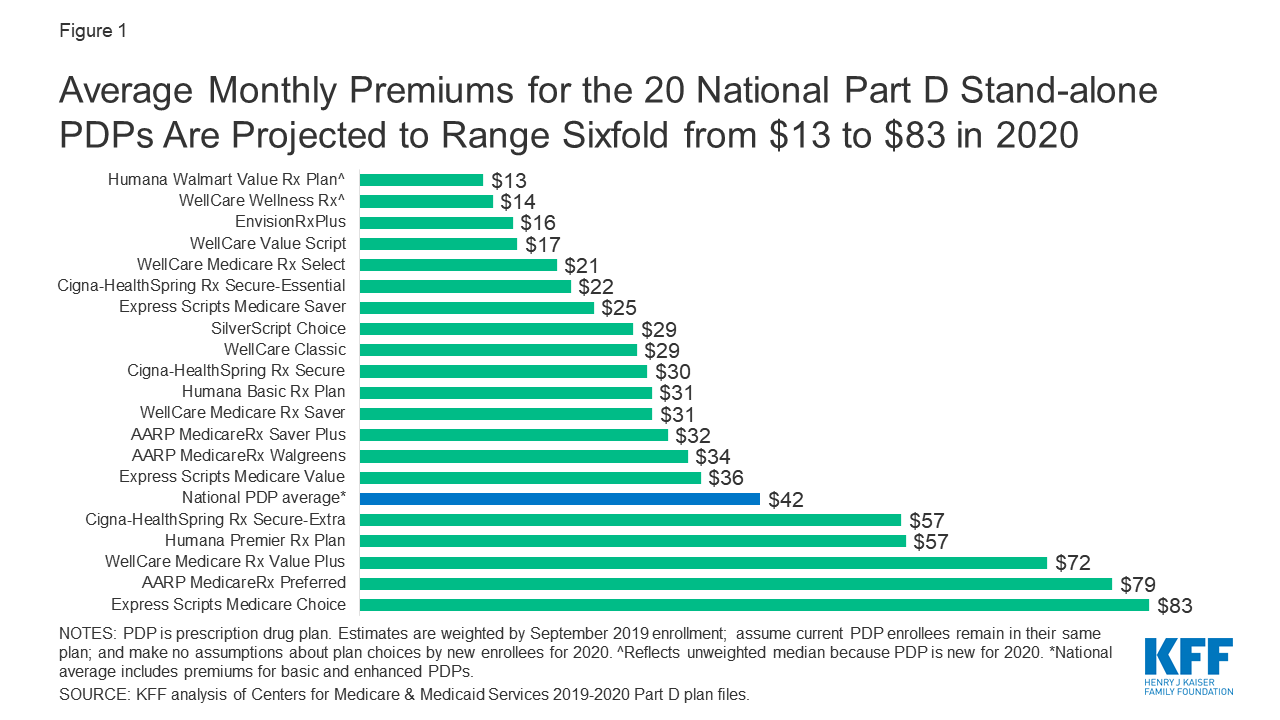
Nov 18, 2021 · Learn about 2021 Medicare prescription drug plan costs and find prescription drug coverage in your area. Medicare Part D provides coverage for prescription medications. The average Part D plan premium in 2021 is $41.64 per month. 1. Because Original Medicare (Part A and Part B) does not cover retail prescription drugs in most cases, millions of Medicare …
What is the maximum Medicare Part D drug deductible for 2022?
Jan 19, 2017 · Under Medicare Part D, Medicare makes partially capitated payments to private insurers, also known as Part D sponsors, ... During the same period, total Part D gross drug costs only grew about 12 percent per year and PMPM Part D gross drug costs only grew nearly 5 percent per year. Gross drug costs and DIR have grown most dramatically since 2013.
How much does Medicare Part D cost in 2021?
2022 Part D national base beneficiary premium— $33.37. This amount is used to estimate the Part D late enrollment penalty and the income-related monthly adjustment amounts listed in the table above. The national base beneficiary premium amount can change each year. If you pay a late enrollment penalty, these amounts may be higher.
Does Medicare pay for MAVYRET?
Yes. 78% of Medicare prescription drug plans cover this drug.
How much does maverick for hep C cost?
Abbvie has priced Mavyret at $13,200 per month, or $26,400 per treatment course, before discounts. Although this is still expensive, Macyret is priced significantly lower than other hepatitis C treatments.Aug 23, 2017
What is the generic for MAVYRET?
No. There is currently no therapeutically equivalent version of Mavyret available in the United States. Note: Fraudulent online pharmacies may attempt to sell an illegal generic version of Mavyret. These medications may be counterfeit and potentially unsafe.
Does Medicaid pay for MAVYRET?
MAVYRET has preferred formulary status on the majority of2: Patients on Medicaid can have out-of-pocket costs of $20 or less depending on state plan. Most patients with commercial insurance will pay as little as $5 per month with their MAVYRET copay card.
What drugs affect MAVYRET?
Coadministration of MAVYRET with drugs that induce P-gp/CYP3A may decrease glecaprevir and pibrentasvir plasma concentrations. Carbamazepine, phenytoin, efavirenz, and St. John's wort may significantly decrease plasma concentrations of glecaprevir and pibrentasvir, leading to reduced therapeutic effect of MAVYRET.
Is MAVYRET or Epclusa better?
If you have liver disease, Epclusa may be a better treatment choice for you. Severe scarring of your liver. Mavyret isn't used for treating hepatitis C if you have severe cirrhosis. However, Epclusa can be used with the drug ribavirin for this purpose.Feb 19, 2021
Is Mavyret better than Harvoni?
Mavyret is reported to have some advantages over Harvoni including the number of HCV genotypes it covers, the length of treatment required, and the cost of a course of treatment.Aug 25, 2021
Does Mavyret cause weight gain?
Weight loss and weight gain weren't reported as side effects of Mavyret during clinical trials. However, Mavyret can cause nausea, which may lead to weight loss in some people. If you feel nauseous while taking this drug, you're likely to eat less food, which may result in weight loss.Aug 18, 2019
How long does it take for Mavyret to start working?
How long does Mavyret take to work? Studies show Mavyret cures hepatitis C in most people within 8 to 16 weeks when it's taken as directed. After that time period, your doctor will order blood tests to see if you still have hepatitis C.Mar 22, 2021
What is the success rate of Mavyret?
Yes, Mavyret is a treatment that can clinically cure hepatitis C viral infection (HCV). The success rate for curing hepatitis C with Mavyret ranges from 95 to 99%.Jul 22, 2020
What are the side effects of Mavyret?
Common side effects of Mavyret include nausea, headache, fatigue (lack of energy), and diarrhea. These side effects could make you feel unwell. While taking Mavyret, talk with your doctor if you feel sick or have side effects that become severe or don't go away.Jan 22, 2021
How can I get Mavyret?
Visit Mavyret.com. Available to patients with commercial prescription insurance coverage who meet eligibility criteria.
Who sells Medicare Part D?
Medicare Part D plans are sold by private insurance companies . These insurance companies are generally free to set their own premiums for the plans they sell. Medicare Part D plan costs in any particular area may depend partly on the cost of other plans being sold in the same area by competing carriers. Cost-sharing.
How much is Medicare Part D 2021?
How much does Medicare Part D cost? As mentioned above, the average premium for Medicare Part D plans in 2021 is $41.64 per month. The table below shows the average premiums and deductibles for Medicare Part D plans in 2021 for each state. Learn more about Medicare Part D plans in your state.
What is the Medicare donut hole?
After 2020, Medicare Part D plans have a shrunken coverage gap, or “donut hole,” which represents a temporary limit on what the plan will cover for prescription drugs. You enter the Part D donut hole once you and your plan have spent a combined $4,130 on covered drugs in 2021.
What is coinsurance and copayment?
Copayments and coinsurance are the amounts that you must pay once your plan’s coverage does begin. A copayment is usually a fixed dollar amount (such as $5) while coinsurance is most often a percentage of the cost (such as 20 percent). Plans might have different copayment or coinsurance amounts for each tier of drugs.
What is the average Medicare Part D premium for 2021?
The average Part D plan premium in 2021 is $41.64 per month. 1. Because Original Medicare (Part A and Part B) does not cover retail prescription drugs in most cases, millions of Medicare beneficiaries turn to Medicare Part D or Medicare Advantage prescription drug (MA-PD) plans to get help paying for their drugs.
What is Part D premium?
Your Part D deductible is the amount that you must spend out of your own pocket for covered drugs in a calendar year before the plan kicks in and begins providing coverage.
How much will Part D cost in 2021?
You enter the Part D donut hole once you and your plan have spent a combined $4,130 on covered drugs in 2021. Once you reach the coverage gap, you will pay up to 25 percent of the cost of covered brand name and generic drugs until you reach total out-of-pocket spending of $6,550 for the year in 2021.
What is Medicare Part D?
Under Medicare Part D, Medicare makes partially capitated payments to private insurers, also known as Part D sponsors, for delivering prescription drug benefits to Medicare beneficiaries . Medicare relies on transaction data reported by Part D sponsors to make sure these payments are accurate. Often, the Part D sponsor or its pharmacy benefits ...
What does higher DIR mean?
Higher levels of DIR generally mean a greater difference between the price assessed at the point-of-sale and the actual financial obligation of the Part D sponsor. The cost of rebates and other price concessions received after the point-of-sale is built into the list price charged at the point-of-sale.
What is PBM in pharmacy?
Often, the Part D sponsor or its pharmacy benefits manager (PBM) receives additional compensation after the point-of-sale that serves to change the final cost of the drug for the payer, or the price paid to the pharmacy for the drug. Examples of such compensation include rebates provided by manufacturers and concessions paid by pharmacies.
Does DIR reduce Medicare premiums?
Higher levels of DIR can reduce beneficiary premiums and some government costs. Under the Part D payment rules, rebates and price concessions received after the point-of-sale are factored into the calculation of beneficiary premiums and Medicare’s direct subsidy payments to Part D sponsors.
What is Medicare Part D?
Since 2006, Americans have had the option to purchase Medicare Part D, an insurance plan that helps cover drug costs for those with Medicare. 1. Unlike Medicare Part A and Part B, you purchase Part D from private insurers or get it as part of your Medicare Advantage Plan. 2 The average Medicare beneficiary had 30 prescription drug plans ...
How much is the deductible for Medicare 2021?
Your deductible varies based on your plan but cannot exceed $445 in 2021, up from $435 in 2020. 9 Some Medicare drug plans don’t have any deductible at all. Before choosing a low- or no-deductible plan, it’s important to calculate the total cost of your plan, including premiums and copays or coinsurance.
How much will the Donut Hole cost in 2021?
Once the total amount of drug costs (including those paid by both you and the plan) reach $4,130 in 2021 on plan-covered drugs, you enter the Coverage Gap, also known as the “ donut hole ” and have to pay 25% of your drug costs. 10. Once you’ve spent $6,550 out of pocket, you enter Catastrophic Coverage.
What are the tiers of drugs?
What Are Drug Tiers? Drug plans publish a formulary, or list of covered drugs. Often, they separate their formularies into “tiers,” with Tier 1 drugs (usually generic drugs) costing the least and Tier 4 drugs (non-preferred, brand name prescription drugs) costing the most.
How much is extra help?
If you have limited resources, you can apply for “Extra Help,” worth about $5,000 from the Social Security Administration. 12 To qualify, you’ll need to have a net worth (excluding your home and personal possessions) of less than $14,610 and an income of less than $19,140.
Who is Beth Braverman?
Beth Braverman is a full-time freelance journalist covering personal finance, healthcare, and careers. A former reporter for MONEY magazine, her work has appeared in dozens of publications, including CNBC.com, CNNMoney.com, and WebMD. ×.
What are the 12 classes of medications in Medicare?
These classes include ACE inhibitors, angiotensin-II reductase inhibitors including direct renin antagonists , antidepressants, antidiabetes therapies including all treatments, anti-ulcerants, beta blockers, calcium channel blockers, epilepsy and movement disorders, narcotic analgesics, respiratory agents including those for asthma and COPD, statins for cholesterol management, and thyroid therapies. These 12 therapy classes represent 55% of overall prescriptions and 57% of branded prescriptions utilized in Medicare Part D in the U.S. in 2015.
What factors influence the cost of medicines?
The drug pricing process is complex and reflects the influence of numerous factors, including manufacturer list prices, confidential negotiated discounts and rebates, insurance plan benefit designs, and patient choices.
What is QuintilesIMS Institute?
The QuintilesIMS Institute leverages collaborative relationships in the public and private sectors to strengthen the vital role of information in advancing healthcare globally. Its mission is to provide key policy setters and decision-makers in the global health sector with unique and transformational insights into healthcare dynamics derived from granular analysis of information.
Key Takeaways
Does Medicare pay for prescriptions? Yes—drug coverage is available through Medicare Part D.
How much does Medicare Part D cost?
Medicare will pay part of the costs of prescription drug coverage for everyone who enrolls in a Part D plan. How much you pay will depend on which prescription drug plan you choose and whether or not you qualify for Extra Help that assists in covering the costs of this coverage.
Medicare Part D Deductible
Remember, a plan with a deductible will not pay for your prescriptions until you pay the deductible amount out-of-pocket. The highest deductible a plan can charge in 2022 is $480. Some plans offer $0 deductible and will pay for your prescriptions right away. Other plans may offer a deductible lower than the maximum of $480 such as $150 or $250.
Copayments and Coinsurance
A copayment, or copay, is a fixed dollar amount for your prescriptions. For example, you might have to pay $5 for a generic drug, $25 for a "preferred" brand name drug and $40 for a non-preferred brand name drug.
What are copay tiers?
Each plan places the drugs it will pay for in different levels, called tiers. Each tier has its own copay or coinsurance amount. Your drugs may be included in all the plans in your area, but they could be listed on different tiers with different copay amounts.
Phases of Part D Prescription Costs
Prescription drug costs may change throughout the year depending on which phase of Part D coverage you are in. There are four phases of Part D coverage:
When does the coverage gap end (catastrophic coverage)?
In Part D, you and the plan you join share the cost of drugs. The money that you spend is called your out-of-pocket costs. That determines if and when the catastrophic coverage begins. In 2022, the catastrophic coverage starts when you have paid $7,050 out-of-pocket.
What is Medicare Part D?
Medicare Part D provides outpatient prescription drug coverage to the elderly and disabled. It is delivered through private plans, including standalone prescription drug plans (PDPs) or Medicare Advantage plans with prescription drug coverage (MA-PDs). Medicare specifies a standard Part D benefit package, but plans can modify the benefits as long as their schemes are equal in value to the standard package.
What drugs did Part D cover?
All Part D plans covered 2 new HCV drugs, Olysio and Sovaldi, and 98% of plans covered Harvoni ( ). Only 33% of MAPDs and 30% of PDPs covered Viekira Pak. Nearly every plan that covered these new drugs used prior authorization and nearly half of the plans used quantity limits. Almost all plans placed new HCV agents in a specialty tier and required coinsurance rather than co-payment. The average coinsurance rate was slightly higher among MAPDs than PDPs (31.4% vs 28.7%), but it varied more among MAPDs (20%-50%) than PDPs (25%-33%).
How long is Sovaldi used?
However, Sovaldi is used with either Olysio (AASLD recommendation) or PR therapy for 12 weeks; it can also be used in combination with ribavirin for 24 weeks. Total spending for a combination of Sovaldi + Olysio was $150,360, and total spending for Sovaldi + PR therapy was $94,950.
How much did HCV drugs cost in 2013?
The financial impact of the new HCV drugs has been particularly salient in Medicare Part D, where spending on these drugs jumped from $283 million in 2013 to $4.5 billion in 2014.
How many people in the US have HCV?
More than 3 million Americans are infected with HCV, with its prevalence concentrated among baby boomers, who were born between 1945 and 1965. 7 HCV causes more deaths in the United States than HIV/AIDS. 8 Chronic HCV is a cause of serious and costly liver diseases, such as cirrhosis and liver cancer, and related hospitalizations and costs have increased during the past decade. 9 Although the burden of HCV can be reduced through screening and treatments, the implementation of recommended screening is limited, and half of the infected population goes undiagnosed. 9
What is the primary data source for Medicare Advantage?
The primary data source was the July 2015 Prescription Drug Plan Formulary and Pharmacy Network Files from CMS, which contains information on plan characteristics and benefits for drugs covered by each Part D plan. We excluded special needs plans (n = 540) because they serve certain specific beneficiaries (eg, institutionalized people) and may have special benefit schemes. After this exclusion, we identified 1635 Medicare Advantage prescription drug plans (MAPDs) and 1013 PDPs.
Is HCV covered by Part D?
It is discouraging that the effectiveness or the therapeutic values of drugs are not considered in benefit decisions. New HCV drugs are highly efficacious, but Part D plans’ coverage for them differs little from coverage for less-effective HCV drugs, such as the first DAAs.
How much does a zepatier cost?
For 28 of the 30 studied specialty drugs used to treat four health conditions—cancer, hepatitis C, multiple sclerosis (MS), and rheumatoid arthritis (RA)—expected annual out-of-pocket costs for a single drug in 2019 range from $2,622 for Zepatier, a treatment for hepatitis C, to $16,551 for Idhifa, a leukemia drug.
How much does a drug cost in 2019?
Expected annual out-of-pocket costs in 2019 average $8,109 across the 28 specialty tier drugs covered by some or all plans in this analysis. For 28 of the 30 studied specialty drugs used to treat four health conditions—cancer, hepatitis C, multiple sclerosis (MS), and rheumatoid arthritis (RA)—expected annual out-of-pocket costs for a single drug in 2019 range from $2,622 for Zepatier, a treatment for hepatitis C, to $16,551 for Idhifa, a leukemia drug. Two of the 30 drugs are not covered by any plan in our analysis. (See Tables 1 and 2 for drug-specific cost and coverage information.)
Does Medicare cover Gleevec?
One of the 15 cancer drugs, Gleevec, is not covered by any plan in our analysis in 2019, but the generic equivalent, imatinib mesylate, is covered by all plans, which is sufficient to meet the formulary coverage requirement that plans cover all or substantially all drugs in six so-called “protected” classes, including cancer drugs.
Does Medicare Part D cover out of pocket costs?
Discussion. This analysis shows that Medicare Part D enrollees who do not receive low-income subsidies can expect to pay thousands of dollars in out-of-pocket costs for a single specialty tier drug in 2019, even though the Part D coverage gap for brands is now fully closed. Although Part D offers catastrophic coverage for high drug costs, ...
Does Part D cover cancer?
Although Part D offers catastrophic coverage for high drug costs, beneficiaries can still face substantial out-of-pocket costs for expensive medications, including many drugs for cancer, hepatitis C, multiple sclerosis, and rheumatoid arthritis, because there is no hard cap on spending in the Part D benefit.
Does Medicare cover specialty drugs?
Figure 5: Medicare Part D plans vary in whether they cover specialty tier drugs that are not in a protected class. Some plans cover a larger number of specialty drugs to treat each condition than other plans (outside of the protected-class cancer drugs).
Is glatiramer acetate higher than copaxone?
Expected annual out-of-pocket costs for glatiramer acetate are actually higher than costs for the brand Copaxone in 2019 —and higher than out-of-pocket costs for the other branded MS drugs—while the share of out-of-pocket costs above the catastrophic threshold is lower.
How is Awp calculated?
The drug manufacturer may report the AWP to the individual publisher of drug pricing data, such as MediSpan or First Data Bank. The AWP may also be calculated by the publisher based upon a mark-up specified by the manufacturer that is applied to the wholesale acquisition cost (WAC) ...
What is the Awp of a drug?
What is the average wholesale price (AWP)? In the United States, the average wholesale price ( AWP) is a pharmaceutical term that describes the average price paid by a retailer to buy a drug from the wholesaler. The AWP benchmark has been used for over four decades to determine pricing and reimbursement of prescription drugs to third parties such as ...
What is the AWP benchmark?
The AWP benchmark has been used for over four decades to determine pricing and reimbursement of prescription drugs to third parties such as the government and private payers. However, the AWP is not a true representation of actual market prices for either generic or brand drug products, and is usually inflated about 20 percent.
What is wholesale acquisition cost?
The wholesale acquisition cost (WAC) is the manufacturer’s list price of the drug when sold to the wholesaler, while the DIRP is the manufacturer’s list price when sold to non-wholesalers. WAC is the most common benchmark used today by pharmacies to buy drugs from wholesalers. Typically a 20% mark-up is applied to the manufacturer-supplied WAC ...
What is an AMP in wholesale?
The AMP, which was established as part of OBRA in 1990, is the average price a wholesaler pays to purchase drug products from the pharmaceutical manufacturer after any rebate or discount is included.
What is coinsurance in pharmacy?
Many patients have coinsurance or copayments, where they only pay for a portion of their prescription cost. The insurance company then pays the rest of the cost (the reimbursement) to the pharmacy. Insurance companies include: prescription benefit managers (PBMs) like Express Scripts, CVS Health, or OptumRx.
Is Awp a government figure?
AWP is not a government-regulated figure, does not include buyer volume discounts or rebates often involved in prescription drug sales, and is subject to manipulation by manufacturers or even wholesalers. As such, the AWP, while used throughout the industry, is a controversial pricing benchmark. 1, 2.