
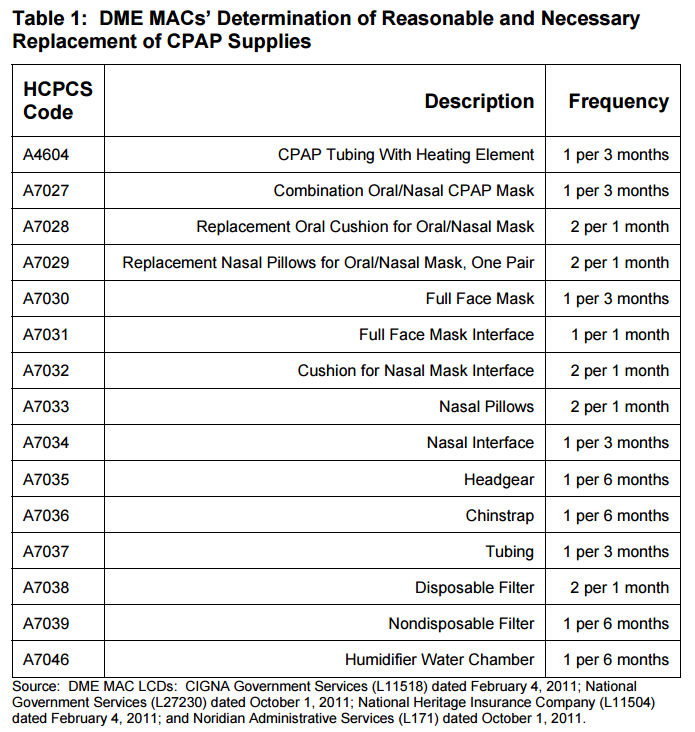
Below is a list of how many times per year Medicare will pay for a portion of certain CPAP supplies, according to the Department of Health and Human Services:
- humidifier water chamber: 2 times per year
- nondisposable filters: 2 times per year
- chinstrap: 2 times per year
- headgear: 2 times per year
- CPAP tubing with heating element: 4 times per year
- combination oral/nasal CPAP mask: 4 times per year
- full face mask: 4 times per year
- nasal interface: 4 times per year
- tubing: 4 times per year
How often does insurance cover a new CPAP machine?
How often does medicare pay for a new CPAP machine? Since CPAP supplies can get dirty and lose effectiveness with use, Medicare covers replacement supplies on a regular schedule. Depending on the item, you may need replacements every two weeks to every six months.
Which CPAP machines are covered by Medicare?
Most insurance plans including Medicaid and Medicare, will offer coverage for the CPAP machine, mask, and supplies. Replacement supplies may also be covered by insurance. Insurance Covered CPAP will serve as an in-network provider with most insurance plans.
Does insurance pay for a CPAP machine?
Most insurance plans partially cover the costs of CPAP machines and related equipment. Often the machines themselves are covered to an extent, but you may be responsible for other components such as tubing. Sometimes replacement parts are covered, with a limit to how many replacement parts can be purchased annually.
Will insurance cover CPAP machine?
Your private insurance may cover some of the costs of your CPAP machine. Many of them follow a process similar to Medicare coverage: The machine must meet the criteria for the medical management of obstructive sleep apnea syndrome and be supported by an order on file from a physician or licensed health care professional.
How often should I replace my CPAP machine?
approximately 5 yearsYour CPAP machine should be replaced after approximately 5 years of use. The good news is, Medicare and most other insurers typically provide coverage for a new CPAP machine around the same time frame.
How Long Does Medicare pay for CPAP machine?
13 monthsfor the machine rental and purchase of related supplies (like masks and tubing). Medicare pays the supplier to rent a CPAP machine for 13 months if you've been using it without interruption. After Medicare makes rental payments for 13 continuous months, you'll own the machine.
What are Medicare requirements for CPAP usage?
Medicare Coverage of CPAP at Home Adherence to CPAP is defined as usage greater or equal to 4 hours per night on 70% of nights during a consecutive 30 days anytime during the first 3 months of initial usage.
What's the average lifespan of a CPAP machine?
roughly three to five yearsThe life expectancy of a CPAP machine differs based on the specific piece of equipment. In general, CPAP machines are used for roughly three to five years. CPAP masks, however, should be replaced several times per year.
Do I own my CPAP machine?
After the rental period is over, you own the device. However, these insurance companies are often requiring proof that you are using the equipment and meeting their usage requirements (at least 4 hours per night for 70% of nights) in order to continue payment.
What is the average cost of a CPAP machine?
A CPAP machine's cost can range anywhere from $250 to $1,000 or more, with prices generally rising for the best cpap machines with more advanced features. Most CPAP machines fall in the $500 to $800 range, however. BiPAP (Bilevel Positive Airway Pressure) machines are more complex and tend to cost more as a result.
Does ResMed accept Medicare?
Do you accept either Medicare or Medicaid? Medicare and Medicaid will pay for medical equipment and supplies only if a supplier has a Medicare or Medicaid supplier number. Expedite, LLC, the operator of the ResMed Shop, does not have a Medicare or Medicaid supplier number.
How long is a sleep study good for Medicare?
There is no lifetime limit on sleep studies. You may need a new study if you discontinue CPAP therapy or fail during the three-month trial period when testing and trials restart.
How is a CPAP machine monitored?
Your RANA sleep clinician routinely checks your CPAP machine for as long as you use it. Inside the machine is an electronic card that collects information about usage, apnea resolve and mask fit. The card also tells us what pressures were needed to keep your apneas controlled.
Does CPAP shorten your life?
The study found that the CPAP users cut their odds of dying from any cause over those 11 years by almost two-thirds, compared to nonusers.
How many years does sleep apnea Take off your life?
If left untreated, obstructive sleep apnea can shorten your life from anywhere between 12-15 years. While there is no permanent cure for obstructive sleep apnea, diagnosis and treatment will alleviate its effects. Proper treatment can ensure that your OSA won't shorten your life.
Does sleep apnea shorten your life expectancy?
Risks of obstructive sleep apnea Sleep apnea is dangerous because if untreated, it leads to high blood pressure and is associated with an increased chance of heart attack, abnormal heart rhythms and heart failure. Studies have shown that sleep apnea can decrease life expectancy by several years.
How Often Does insurance cover a new CPAP machine?
If you’ve been diagnosed with sleep apnea, it’s likely that you’ll need a CPAP mask, as this is considered the best course of treatment for the con...
Does Anthem cover CPAP machines?
Thankfully, the majority of Anthem Blue Cross Blue Shield PPO and HMO plans cover CPAP therapy supplies. So if you’re close to meeting your deducti...
How often will insurance pay for CPAP supplies?
Because CPAP machines and their tubing are required daily, they’re subject to significant wear and tear, so you may be wondering how often insuranc...
How often can you get a CPAP machine with Medicare?
Medicare may cover a 3-month trial of CPAP therapy, and they may cover it longer if your doctor documents in your medical record that you meet cert...
How long is a CPAP Prescription good for?
Seen as you’ll need a CPAP prescription from your doctor in order to make an insurance claim, you may be wondering how long your prescription is va...
Can I just buy a CPAP machine?
No. In order to buy a CPAP machine, you must have results from a sleep study and a CPAP prescription from your doctor or healthcare professional. T...
How long does it take to replace a CPAP machine?
Your CPAP machine should be replaced after approximately 5 years of use. The good news is, Medicare and most other insurers typically provide coverage for a new CPAP machine around the same time frame.
Does ResMed Air10 have a humidifier?
All ResMed Air10 machines come with a built-in humidifier that ’s easier to fill and clean and takes up less space. You can also try using ClimateLineAir™, a heated tubing option designed to maintain the temperature of the air as it passes from the humidifier through the tube.
Medicare Coverage for CPAP Machines
Caitlin McCormack Wrights has over a decade of experience writing hundreds of articles on all things finance. She specializes in insurance, mortgages, and investing and relishes making dull subject matter gripping and everyday topics amazing. Caitlin has a bachelor's from Duke and a master's from Princeton.
When Will Medicare Cover CPAP Machines?
Medicare Part B covers the use of CPAP machines by adult patients with obstructive sleep apnea. Medicare initially will cover the cost of the CPAP for up to three months if your sleep apnea diagnosis is documented by a sleep study.
How To Get Medicare To Cover a CPAP Machine
Medicare will cover a CPAP machine if you meet two conditions. You must first be diagnosed with obstructive sleep apnea, and you must submit your primary doctor’s order or prescription to the right supplier to receive coverage. Here are the steps you’ll need to take to make that happen.
How Much Does a CPAP Machine Cost With Medicare?
Medicare typically covers the most basic level of equipment, and it may not pay for upgrades. In the case where Medicare doesn’t cover upgrades or extra features, you’ll need to sign an Advance Beneficiary Notice (ABN) before you get the equipment.
The Bottom Line
The rules of how DMEs are covered, including CPAP machines, are generally the same whether you have Original Medicare or a Medicare Advantage Plan. However, the amount you pay with Original Medicare and a Medicare Advantage Plan may often differ. Compare Medicare and Medicare Advantage to learn more.
How often can I get a new CPAP machine while on Medicare?
Once you’ve continuously used your CPAP machine for the approved 13-month rental, you will own it. However, CPAP supplies may lose effectiveness with use, and Medicare covers their replacement. Guidelines suggest replacing a CPAP mask every three months and a non-disposable filter every six months. 4
How do I get CPAP supplies covered by Medicare?
Medicare will only help cover CPAP supplies and accessories if you get them from a Medicare-approved contract supplier after completing the necessary medical steps.
What happens if you start CPAP therapy but your symptoms remain?
If you start therapy but your symptoms remain, you may need to be tested again to evaluate for another sleep disorder or to adjust your machine pressure. Weight gain or weight loss (this is one of the most desirable side effects of CPAP therapy).
Why are CPAPs so important?
(1) If a CPAP machine is more attractive and user-friendly, someone diagnosed with sleep apnea is more likely to use it. They’re quieter and smaller.
Does snoring go away with pressure?
If the symptoms that lead you to get tested and start therapy (snoring, gasping at night, daytime sleepiness) return, you should talk to your doctor about evaluating your sleep problems and potentially changing your machine pressure. Your symptoms don’t go away.
Does Anthem cover CPAP machines?
Thankfully, the majority of Anthem Blue Cross Blue Shield PPO and HMO plans cover CPAP therapy supplies. So if you’re close to meeting your deductible, you may be able to acquire your CPAP device at almost no cost to you.
How often will insurance pay for CPAP supplies?
Because CPAP machines and their tubing are required daily, they’re subject to significant wear and tear, so you may be wondering how often insurance will cover CPAP supplies.
How often can you get a CPAP machine with Medicare?
Medicare may cover a 3-month trial of CPAP therapy, and they may cover it longer if your doctor documents in your medical record that you meet certain conditions regarding the use of the device and they claim that the CPAP therapy is helping you.
How long is a CPAP Prescription good for?
Seen as you’ll need a CPAP prescription from your doctor in order to make an insurance claim, you may be wondering how long your prescription is valid for. Your prescription may display an expiration date, in which case it will be valid until this date.
Can I just buy a CPAP machine?
No. In order to buy a CPAP machine, you must have results from a sleep study and a CPAP prescription from your doctor or healthcare professional.
Final Verdict
According to SoClean CEO Bob Wilkins, there are roughly 8 million CPAP users in the United States, and this is growing yearly.
Medicare CPAP Compliance
Medicare can and will cover CPAP therapy for a three-month trial or longer, provided your doctor provides proper documentation that the treatment is helping you and that you meet specific requirements.
Does Medicare cover sleep studies?
Medicare Part B—the medical insurance portion—does cover Type I, II, III, and IV sleep tests and devices. Note that, like many other covered services, you’ll pay 20% of the Medicare-approved amount after you meet your Part B deductible. Doctors may require an at-home sleep apnea test.
How often will Medicare pay for a new CPAP machine?
Medicare will generally pay for CPAP machine replacement every five years. Medicare can also pay 80% of the cost for replacement supplies. The Part B deductible will still apply. Replacement supplies for CPAP machines include:
Are CPAP machines considered Durable Medical Equipment?
CPAP machines are considered Durable Medical Equipment (DME), which means that they’re covered by Medicare. DME must be durable, used for a medical reason and used in your home. DME should not be useful to someone who is well.
Are CPAP cleaners covered by Medicare?
Unlike CPAP machines themselves or their tubing, masks or replacement parts, CPAP cleaners aren’t covered by Medicare. Because CPAP cleaners and sanitizers aren’t considered DME, they’re not eligible for coverage. They can, however, be purchased with HSA/FSA funds.
Review your Medicare Coverage with SelectQuote
If your doctor has ordered a sleep test and/or CPAP therapy for sleep apnea, you’ll want to be sure that your Medicare coverage can help pay for your treatment and medical care. If you have questions about Medicare or would like a licensed insurance agent to help review your current coverage, SelectQuote can help.
How long does it take to use CPAP for Medicare?
How does Medicare define CPAP compliance or adherence? Medicare defines adherence as using the device more than 4 hours per night for 70% of nights (that’s 21 nights) during a consecutive 30 day period any time in the first three months of initial usage.
When does Medicare continue to cover PAP?
If you are successful with the 3-month trial of PAP, Medicare may continue coverage if the following criteria are met: Clinical re-evaluation between the 31st and 91st day after starting therapy, to include: Treating physician documents that the patient is benefiting from therapy; and.
How long does a bi level CPAP trial last?
If the patient switches to a bi-level device within the 3-month trial, the length of the trial is not changed as long as there are at least 30 days remaining. If less than 30 days remain of the trial period, re-evaluation must occur before the 120th day (following the same criteria as CPAP adherence).
How much does Medicare pay for a PAP?
Medicare will pay 80% of the Medicare-approved amount for a PAP device after you’ve met your Part B deductible (learn about this and other insurance terms here ). If you have a secondary insurance, they may pick up the remaining 20% (read our post about how much sleep studies cost here ).
Does Medicare cover bi level respiratory assist?
Medicare will cover a bi-level respiratory assist device without backup (this is what they call a bi-level or BiPAP) for patients with obstructive sleep apnea if the patient meets the criteria for PAP therapy (outlined above) and:
Does Medicare require proof of usage?
Many other insurance companies are now following Medicare’s lead and requiring proof of usage before continuing to pay for the machine. Learn more about that here. If adherence to therapy is not documented within the first three months, the patient fails the trial period.
Does Medicare cover CPAP?
Yes. Medicare covers a 3-month trial of for CPAP therapy (learn more about CPAP here) if you’ve been diagnosed wtih obstructive sleep apnea (learn more about OSA here) and meet one of the following criteria: AHI or RDI > 15 events per hour with a minimum of 30 events or. AHI or RDI > 5 to14 events per hour with a minimum ...
How often does Medicare pay for CPAP?
nondisposable filters: 2 times per year. chinstrap: 2 times per year.
How long does a CPAP machine last?
Your CPAP machine is paid for after 13 months and you’ll own it, but it should last several years . You may have it replaced with your medical benefit after this time.
What is Medicare Part B?
Medicare Part B is the section that pays for durable medical equipment (DME), such as CPAP machines. To have your CPAP machine covered, you need to make sure that your clinician and device supplier participate in the Medicare program.
How long can you rent a CPAP machine?
CPAP rental for 13 months if you’ve been using it consistently (after 13 months , you’ll own the CPAP machine) masks or nose pieces you wear when using the machine. tubing to connect the mask or nose piece to the machine. This Medicare coverage applies only if your doctor and supplier participate in the Medicare program.
Does Medicare cover CPAP machines?
Medicare will cover a part of the cost of a CPAP machine if you’ve been diagnosed with obstructive sleep apnea. Coverage for CPAP machines falls under the Medicare Part B coverage of durable medical equipment. You’ll still pay a portion of the cost for your CPAP machine, unless you have a Medigap plan to cover those costs.
Do you pay for a CPAP machine?
You’ll still pay a portion of the cost for your CPAP machine, unless you have a Medigap plan to cover those costs. A continuous positive airway pressure (CPAP) machine is a medical device that gives you extra oxygen with a bit of force.
How much does Medicare cover for a CPAP machine?
After you pay the $185 yearly Part B deductible (for 2019), Medicare will cover 80% of the Medicare-approved rental costs of the CPAP machine for 3 months, ...
How long is a CPAP trial?
If you have been formally diagnosed with sleep apnea, you are likely eligible for a 3-month trial of CPAP therapy. If the therapy is successful, your doctor can extend the treatment and Medicare will cover it.
What is the best treatment for sleep apnea?
A continuous positive airway pressure (CPAP) machine is the most common treatment for moderate to severe sleep apnea. The machine is equipped with a mask that blows air into your throat while you are sleeping to keep your airway ...
How long does breathing pause last?
Breathing pauses from sleep apnea can last from several seconds to minutes and can occur over 30 times per hour. Sleep apnea is a chronic condition that disrupts your sleep and can lead to daytime sleepiness and more serious health conditions.
Does Medicare Supplement have a 20% deductible?
Depending on the Medicare Supplement insurance plan you choose, you could get full coverage for both the Part B deductible and the 20% Part B coinsurance cost. You can use the comparison chart below to see the benefits that are offered by each type of standardized Medigap plan sold in most states.
Can you take a prescription for a CPAP machine?
After you are approved for therapy, your doctor will give you a medical prescription for the CPAP machine. You can take this to any medical equipment supplier that accepts Medicare payments. If they accept Medicare, the supplier will bill Medicare directly for your Medicare-covered CPAP supplies.
Does Medicare cover CPAP?
Medicare does cover CPAP machine therapy if you are diagnosed with sleep apnea. You may be eligible for sleep apnea treatment options if you are enrolled in Medicare Part B and have been diagnosed with obstructive sleep apnea. If you have been formally diagnosed with sleep apnea, you are likely eligible for a 3-month trial of CPAP therapy.
Get A Second Clinical Evaluation
If Medicare covers your CPAP machine for the three-month trial period, you must undergo a second clinical evaluation to establish medical necessity for continued coverage. During the face-to-face evaluation, your doctor must document that your symptoms of sleep apnea have improved and that youve adhered to consistent CPAP therapy.
Does Medicare Pay For Cpap Machines And Supplies
Many or all of the products featured here are from our partners who compensate us. This may influence which products we write about and where and how the product appears on a page. However, this does not influence our evaluations. Our opinions are our own. Here is a list of our partners and here’s how we make money.
How Do You Treat Sleep Apnea
Mild cases of sleep apnea are often managed through simple lifestyle changes such as quitting smoking, losing weight or treating nasal allergies. For individuals who have a moderate or severe case of sleep apnea, treatment may be more complex, and can include supplemental oxygen, oral appliances or airway-pressure devices, including CPAP machines.
What Are Medicare Guidelines For Cpap
You have a three-month trial period covered by Medicare. After three months, your doctor will check how the treatment is working for you. Medicare may cover CPAP therapy long-term if your doctor verifies in your medical record that:
Option : Use Medicares Website
If you have a Medicarehealthcare plan, you can also find in-network durable medical equipment providers by using Medicares Supplier Directory. After you click the link, enter your zipcode and select the corresponding product category. For CPAP machines and related supplies, select .
When Should I Contact My Private Insurance
Once you think you have sleep apnea, check with your insurance company to find out what type of coverage you get for CPAP.
Insurance And Cpap Machines
The terms of your CPAP machine, insurance coverage depends on your provider. Some providers reimburse you for the cost of purchasing the machine outright, while others require a rent-to-own plan under which you must use the machine for a set amount of time before it becomes your property.
