How often does Medicare pay for A1c blood test?
Also to know is, how often does medicare pay for a1c blood test? The A1c test, which doctors typically order every 90 days, is covered only once every three months. If more frequent tests are ordered, the beneficiary needs to know his or her obligation to pay the bill, in this case $66 per test.
How much does a hemoglobin A1c test cost?
The A1c test, which doctors typically order every 90 days, is covered only once every three months. If more frequent tests are ordered, the beneficiary needs to know his or her obligation to pay the bill, in this case $66 per test. Likewise, what diagnosis will cover a hemoglobin a1c?
Does Medicare cover HbA1c tests?
Medicare did not cover A1c, howver, deeming it "medically not necessary." If Medicare rejects the blood order claim, then apparently his AARP supplemental also doesn't kick in. Is this correct? You have to be a diabetic to have HbA1c test covered by Medicare Part B? Diagnostic testing is not covered?
How often should the HbA1c test be performed?
Performance of the HbA1c test at least two times a year in patients who are meeting treatment goals and who have stable glycemic control is supported by the American Diabetes Association Standards of Medical Care in Diabetes - 2016 (ADA Standards) 1.

How often does Medicare pay for AIC test?
The A1c test, which doctors typically order every 90 days, is covered only once every three months. If more frequent tests are ordered, the beneficiary needs to know his or her obligation to pay the bill, in this case $66 per test.
Does Medicare cover hemoglobin A1c blood test?
Hemoglobin A1c Tests: Your doctor might order a hemoglobin A1c lab test. This test measures how well your blood glucose has been controlled over the past 3 months. Medicare may cover this test for anyone with diabetes if it is ordered by his or her doctor.
How often can you bill an A1c?
“HbA1c testing should be performed at least biannually in all patients and quarterly for patients whose therapy has changed or who are not meeting treatment goals.” “HbA1c may be used for the diagnosis of diabetes, with values >6.5% being diagnostic.
How often does Medicare cover routine lab work?
every 5 yearsBoth Original Medicare and Medicare Advantage cover a cholesterol screening test every 5 years. Coverage is 100%, which makes the test free of charge.
What diagnosis code covers A1c for Medicare?
Medicare recommends and provides coverage for diabetes screening tests through Part B Preventive Services for beneficiaries at risk for diabetes or those diagnosed with prediabetes....Table 1: HCPCS/CPT Codes and Descriptors.HCPCS/CPT CodesCode Descriptors83036Hemoglobin A1C3 more rows
What ICD 10 code will cover hemoglobin A1c?
R73. 09 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM R73.
What are the new guidelines for A1C?
ADA now recommends A1C below 7% or TIR above 70%, and time below range lower than 4% for most adults. In previous years, the Standards of Care included an “A1C Testing” subsection that recommended people with diabetes test their A1C two to four times a year with an A1C target below 7%.
How do you bill for A1C?
CPT code 83037 represents the HbA1c test performed in the provider's office or clinic when using a device cleared by the United States Food and Drug Administration (FDA) for home use. CPT code 83037 is allowed up to four times per calendar year.
How often can you bill 83036 Medicare?
every 3 monthsWe are getting these denials also. We bill the 83036 with a qw. I did some research and this is only payable every 3 months for most patients.
Does Medicare pay for blood work every 6 months?
Medicare Part B also covers 80 percent of the Medicare-approved cost of preventive services you receive from your doctor or other medical provider. This includes wellness appointments, such as an annual or 6-month checkup.
Is an annual wellness visit required by Medicare?
Medicare covers a “Welcome to Medicare” visit and annual “wellness” visits. While both visit types are available to Medicare recipients, recipients aren't required to participate in either visit type to maintain their Medicare Part B coverage.
Does Medicare pay for annual wellness visit?
If you qualify, Original Medicare covers the Annual Wellness Visit at 100% of the Medicare-approved amount when you receive the service from a participating provider. This means you pay nothing (no deductible or coinsurance).
How often does Medicare pay for A1C blood tests?
The A1c test, which is normally ordered every 90 days by doctors, is only covered once every three months. If more frequent tests are needed, the r...
Why would a doctor order an A1C test?
The A1C test is a diabetes test that evaluates a person's average blood glucose level over a three-month period. It can be used by doctors to diagn...
What happens when your A1C goes up?
When a person's blood glucose levels remain persistently high over time, A1c levels rise because more red blood cells get sugar-coated. Because the...
How does diabetes affect kidney function?
Diabetes increases your risk of developing chronic kidney disease (CKD). CKD is present when your kidneys fail to work properly. Your body cannot r...
What are the symptoms of diabetic nephropathy?
Symptoms of diabetic nephropathy include increased urinary frequency, intensity, and volume. You may also experience pain in your lower back, hips,...
What is your A1C in blood work?
The A1C test, commonly known as the hemoglobin A1C or HbA1c test, is a straightforward blood test that examines your average blood sugar levels ove...
How often is A1C covered?
The A1c test, which doctors typically order every 90 days, is covered only once every three months. If more frequent tests are ordered, the beneficiary needs to know his or her obligation to pay the bill, in this case $66 per test.
Does Medicare cover insulin?
Medicare Part B covers the same type of blood glucose testing supplies for people with diabetes whether or not they use insulin. However, the amount of supplies that are covered varies. Uses insulin, they may be able to get up to 100 test strips and lancets every month, and 1 lancet device every 6 months.
Does Medicare cover hemoglobin A1C?
This test measures how well your blood glucose has been controlled over the past 3 months. Medicare may cover this test for anyone with diabetes if it is ordered by his or her doctor.
Why would a doctor order an A1C test?
The A1C test is a diabetes test that evaluates a person's average blood glucose level over a three-month period. It can be used by doctors to diagnose type 2 diabetes and to monitor patients' diabetes. A blood glucose test determines the amount of sugar (or glucose) in a person's blood.
What happens when your A1C goes up?
When a person's blood glucose levels remain persistently high over time, A1c levels rise because more red blood cells get sugar-coated. Because the association between a red blood cell and sugar is permanent, the test is typical of a 2 to 3-month average.
What is your A1C in blood work?
The A1C test, commonly known as the hemoglobin A1C or HbA1c test, is a straightforward blood test that examines your average blood sugar levels over the previous three months.
What is CMS in healthcare?
The Centers for Medicare & Medicaid Services (CMS), the federal agency responsible for administration of the Medicare, Medicaid and the State Children's Health Insurance Programs, contracts with certain organizations to assist in the administration of the Medicare program. Medicare contractors are required to develop and disseminate Local Coverage Determinations (LCDs). CMS believes that the Internet is an effective method to share LCDs that Medicare contractors develop. While every effort has been made to provide accurate and complete information, CMS does not guarantee that there are no errors in the information displayed on this web site. THE UNITED STATES GOVERNMENT AND ITS EMPLOYEES ARE NOT LIABLE FOR ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION, PRODUCT, OR PROCESSES DISCLOSED HEREIN. Neither the United States Government nor its employees represent that use of such information, product, or processes will not infringe on privately owned rights. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information, product, or process.
What is the ICD-10 code for uncontrolled diabetes?
Under ICD-10 Codes That Support Medical Necessity-Group 2-Secondary Dual Codes-diagnoses that must be used in conjunction with a Group 1 code that indicates a current state of uncontrolled diabetes (hyperglycemia) added E10.21 as it was inadvertently omitted from Group 2.
Can you use CPT in Medicare?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
Does the 21st Century Cures Act apply to new LCDs?
At this time 21st Century Cures Act will apply to new and revised LCDs that restrict coverage which requires comment and notice. This revision is not a restriction to the coverage determination; and, therefore not all the fields included on the LCD are applicable as noted in this policy.
Is CPT a year 2000?
CPT is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon no upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
When will Medicare start paying for insulin?
Insulin savings through the Part D Senior Savings Model. Starting January 1, 2021, you may be able to get Medicare drug coverage that offers broad access to many types of insulin for no more than $35 for a month's supply.
What is original Medicare?
Your costs in Original Medicare. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance. .
When is open enrollment for insulin?
You can join during yearly Open Enrollment (October 15 – December 7) .
Does Medicare cover blood sugar screening?
A history of high blood sugar (glucose) Medicare also covers these screenings if 2 or more of these apply to you: You’re age 65 or older. You’re overweight. You have a family history of diabetes (parents or siblings).
What is the fasting glucose for A1C?
You have a hemoglobin A1c test result between 5.7 and 6.4%, a fasting plasma glucose of 110-125mg/dL, or a 2-hour plasma glucose of 140-199 mg/dL (oral glucose tolerant test) within 12 months before attending the first core session.
What is Medicare Diabetes Prevention Program?
The Medicare Diabetes Prevention Program is a proven health behavior change program to help you prevent type 2 diabetes.
What percentage of people with diabetes have poor glycemic control?
The CDC reports that 12.6% of adults with diabetes exhibit poor glycemic control. 2 CDC researchers state that the majority of adults with diabetes would benefit from reduction of A1c levels to ≤ 7%, and that an A1c level of 9% represents a modifiable, high level of risk that warrants additional intervention. ...
Is insulin required for type 2 diabetics?
Required for all type 2 diabetic patients, regardless of insulin therapy status
Does Aspen Healthcare have Medicare?
Aspen Healthcare is aware of the new requirements and will help doctors make sure all plans of care are in compliance with all Medicare regulations . Top points from the new local coverage determination include: Required for all type 2 diabetic patients, regardless of insulin therapy status.
Does Medicare cover diabetes mellitus?
1 The local coverage determination applies to sixteen states including Texas, and it took effect earlier this year.
Does a home health plan have to monitor HBA1C?
All home health plans of care for patients with type 2 diabetes must include HbA1c level monitoring at least quarterly, and such plans of care must also include intermittent capillary blood/serum glucose level monitoring.
How often should you check glycated hemoglobin?
Glycated hemoglobin in whole blood assesses glycemic control over a period of 4-8 weeks and appears to be the more appropriate test for monitoring a patient who is capable of maintaining long-term, stable control. Measurement may be medically necessary every 3 months to determine whether a patient's metabolic control has been on average within the target range. More frequent assessments, every 1-2 months, may be appropriate in the patient whose diabetes regimen has been altered to improve control or in whom evidence is present that intercurrent events may have altered a previously satisfactory level of control (for example, post-major surgery or as a result of glucocorticoid therapy). Glycated protein in serum/plasma assesses glycemic control over a period of 1-2 weeks. It may be reasonable and necessary to monitor glycated protein monthly in pregnant diabetic women. Glycated hemoglobin/protein test results may be low, indicating significant, persistent hypoglycemia, in nesidioblastosis or insulinoma, conditions which are accompanied by inappropriate hyperinsulinemia. A below normal test value is helpful in establishing the patient's hypoglycemic state in those conditions.
Why is glycated hemoglobin important?
Glycated hemoglobin/protein testing is widely accepted as medically necessary for the management and control of diabetes. It is also valuable to assess hyperglycemia, a history of hyperglycemia or dangerous hypoglycemia. Glycated protein testing may be used in place of glycated hemoglobin in the management of diabetic patients, and is particularly useful in patients who have abnormalities of erythrocytes such as hemolytic anemia or hemoglobinopathies.
What is the name of the blood test used to measure glucose levels in diabetics?
The management of diabetes mellitus requires regular determinations of blood glucose levels. Glycated hemoglobin/protein levels are used to assess long-term glucose control in diabetes. Alternative names for these tests include glycated or glycosylated hemoglobin or Hgb, hemoglobin glycated or glycosylated protein, and fructosamine.
Can glycated hemoglobin be analyzed?
When the glycated hemoglobin assay is initially performed in these patients, the laboratory may inform the ordering physician of a possible analytical interference. Alternative testing, including glycated protein, for example, fructosamine, may be indicated for the monitoring of the degree of glycemic control in this situation. It is therefore conceivable that a patient will have both a glycated hemoglobin and glycated protein ordered on the same day. This should be limited to the initial assay of glycated hemoglobin, with subsequent exclusive use of glycated protein. These tests are not considered to be medically necessary for the diagnosis of diabetes.
How long does it take for Medicare to pay for A1C?
Medicare will not pay for an A1c sooner than 90 days from the last one. Was one done less than 90 days before this one?
Is a 126 HBA1C diabetic?
In the past they have used 2 fasting bgs done on different days. A reading over 126 is considered diabetic.
Do all doctors have Medicare codes?
Ask the doctor to put in the proper codes and if they don't know they should contact Medicare directly. Would appear to me that all doctors have the codes.
Does Medicare cover A1C?
Medicare did not cover A1c, howver, deeming it "medically not necessary.". If Medicare rejects the blood order claim, then apparently his AARP supplemental also doesn't kick in.
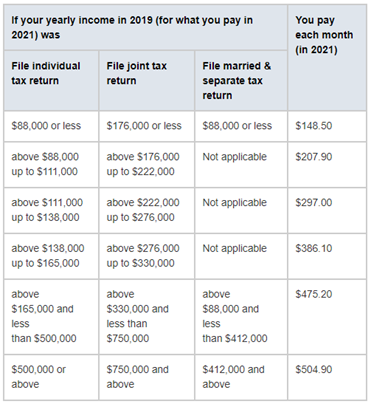
How much is Medicare Part B 2021?
You have to meet your annual deductible for this coverage as well. In 2021, the deductible is $203 for most people. Remember, you also have to pay your monthly Part B premium, which is $148.50 in 2021 for most beneficiaries.
How often does Medicare cover mammograms?
once a year if you meet criteria. *Medicare covers diagnostic mammograms more often if your doctor orders them. You are responsible for the 20 percent coinsurance cost. Other nonlaboratory diagnostic screenings Medicare covers include X-rays, PET scans, MRI, EKG, and CT scans.
What is Medicare Part A?
Medicare Part A offers coverage for medically necessary blood tests. Tests can be ordered by a physician for inpatient hospital, skilled nursing, hospice, home health, and other related covered services. Medicare Part B covers outpatient blood tests ordered by a physician with a medically necessary diagnosis based on Medicare coverage guidelines.
How much does a blood test cost?
The costs are based on the particular test, your location, and the lab used. Tests can run from a few dollars to thousands of dollars. That’s why it’s important to check that your test is covered before you have it done.
Does Medigap cover out of pocket costs?
Medigap (Medicare supplemental insurance) plans can help pay for some out-of-pocket costs like coinsurance, deductibles, or copayments of covered screenings and other diagnostic tests.
Does Medicare cover 20 percent coinsurance?
You have to pay your 20 percent coinsurance as well as your deductible and any copays. Remember to go to providers that accept assignment to avoid charges Medicare won’t cover. Helpful links and tools. Medicare offers a tool you can use to check which tests are covered.
Does Medicare Advantage cover blood work?
Medicare Advantage, or Part C, plans also cover blood tests. These plans may also cover additional tests not covered by original Medicare (parts A and B). Each Medicare Advantage plan offers different benefits, so check with your plan about specific blood tests. Also consider going to in-network doctors and labs to get the maximum benefits.