Will Medicare pay for a PSA test?
If you have a PSA test, you won’t be liable for costs. But you’ll need to be sure your doctor accepts Medicare, or you could have to pay the full costs. Medicare Advantage policies must cover a minimum of what Medicare will cover. What exactly does this mean for you? While you’ll get a routine PSA test at no charge to you, there may be extra fees.
How often can you get preventive screening tests with Medicare?
Medicare now has a long list of preventive screenings that are covered at no cost to the patient. But how often can you get these preventive screening tests? The answer varies from test to test. I had a call today from a man who is new to Medicare and was asking about getting an annual physical.
Does Medicare cover prostate screenings?
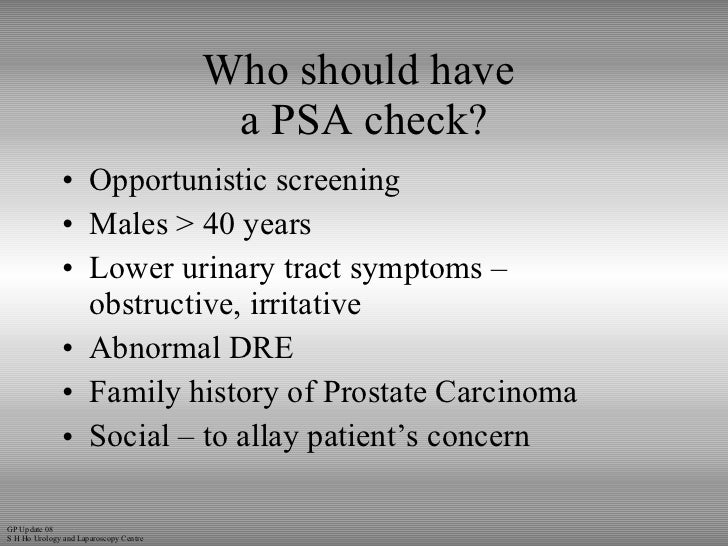
Medicare covers one prostate screening a year ( every 12 months) for all male Medicare patients age 50 and older. This screening includes a Prostate-Specific Antigen (PSA) blood test and a digital rectal exam (DRE).
What is the difference between screening PSA and diagnostic PSA?
Screening PSA tests are defined as those that are performed in the absence of signs or symptoms of prostate cancer. Diagnostic PSA tests are defined as those performed when the patient has signs or symptoms.

How many PSA tests does Medicare cover?
Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. covers digital rectal exams and prostate specific antigen (PSA) blood tests once every 12 months for men over 50 (starting the day after your 50th birthday).
Is PSA screening yearly?
Men who choose to be tested who have a PSA of less than 2.5 ng/mL may only need to be retested every 2 years. Screening should be done yearly for men whose PSA level is 2.5 ng/mL or higher.
When does Medicare stop paying for PSA?
Medicare coverage Medicare covers PSA blood test and a DRE once a year for all men with Medicare age 50 and over. There is no co-insurance and no Part B deductible for the PSA test.
How often do you screen for PSA?
Frequency of PSA testing — For patients who choose to undergo PSA screening, some experts suggest repeating PSA testing every two years until it is appropriate to discontinue screening, whereas other experts repeat PSA testing annually.
How often should a 70 year old man have a PSA test?
In men at average risk, the harms of PSA testing often outweigh the benefits. American Urological Association (AUA) age guidelines: The AUA does not recommend routine PSA screening for men 70 or older or with a life expectancy of less than 10 to 15 years.
What is the average PSA for a 70 year old?
3.5-4.5: Normal for a man 60-70 yrs. 4.5-5.5: Normal for a man 70-80 yrs.
Does Medicare pay for a PSA test after age 75?
One reason is that Medicare pays for annual prostate cancer screening in all men 50 years and older, with no upper age limit.
What diagnosis will cover PSA screening?
PSA when used in conjunction with other prostate cancer tests, such as digital rectal examination, may assist in the decision making process for diagnosing prostate cancer. PSA also, serves as a marker in following the progress of most prostate tumors once a diagnosis has been established.
How much does PSA test cost?
The cost for a PSA test is fairly low—about $40. If your result is abnormal, the costs start adding up. Your doctor will usually refer you to a urologist for a biopsy.
What is the difference between PSA screening and PSA diagnostic?
Screening PSA tests are defined as those that are performed in the absence of signs or symptoms of prostate cancer. Diagnostic PSA tests are defined as those performed when the patient has signs or symptoms.
What is the normal PSA for a 85 year old man?
Regarding the results of the present study, the normal PSA level increased by age from 2.5th percentile to 95th percentile. As a result, the normal PSA level increased from 0.00 ng/mL to 4.89 ng/mL in the age group of 60–64 years and 0.0 ng/mL to 33.17 ng/mL in the age group of 85 years and over.
Should a 75 year old man have a prostate biopsy?
Prostate biopsies can be avoided in men older than 75 years who have PSA levels above 20 ng/mL because it is highly probable prostate cancer (PCa) will be detected and conservative treatment recommended, Scottish researchers concluded.
How often should you have a PSA test UK?
PSA tests should be done between the ages of 40 to 55. If the patient's PSA level appears to be under 2.5 ng/ml, he'll need to get tested once every two years. If the PSA level is over 2.5 ng/ml, the frequency increases to once every year.
Why PSA test is not recommended?
However, there are some potential downsides once the results are in. These include: Elevated PSA levels can have other causes, such as benign prostate enlargement (benign prostatic hyperplasia) or prostate infection (prostatitis). These false-positives are common.
How much should PSA increase per year?
In the overall study population, the mean change in PSA levels was 2.9% per year and the rate of change in PSA increased modestly with age (P < . 001). Overall, men who developed prostate cancer experienced a more rapid percent change in PSA per year than men who did not (P < .
What percentage of men get PSA tests?
In 2018, 39.0% of men aged 55-69 years had a PSA test within the past year.
How much does a PSA test cost?
A standard PSA test can cost you between $60 and $80. Depending on the care level you need following the initial screen, you can expect to pay more. You may need follow-up visits and screenings to further check for cancer. So, while your initial screen is free, it’s best to prepare for extra charges in the future.
How often does Part B cover prostate?
Part B will cover prostate-specific antigen tests once every 12 months. Men over 50 can have a PSA test, beginning on their 50th birthday. You won’t be responsible for any charges for this testing since it’s preventive care.
What causes high PSA levels?
A high level of PSA in the blood can mean a few things, such as: 1 A reaction to certain medications. 2 You may have an enlarged prostate. 3 You may suffer from a prostate infection.
What is prostate specific antigen test?
A prostate-specific antigen test is a blood test. The PSA level in the blood may be higher for those who are dealing with prostate-related issues.
How many men get prostate cancer?
About one out of every nine men will receive a prostate cancer diagnosis. The blood test is considered a routine screening for beneficiaries. As long as your doctor takes Medicare, you should have coverage. In conjunction with other testing methods, PSA tests can help screen for cancer at an early stage so you can get the best treatment available.
Does Medicare cover prostate specific antigen tests?
Does Medicare Cover Prostate-Specific Antigen Tests? Medicare will cover a PSA test for men over the age of 50. You may even be able to get testing done if you’re under 50. But your doctor must feel it’s medically necessary. Keep in mind that having a vasectomy does not increase your risk for prostate cancer.
Can you overpay for a PSA test?
Remember that early detection is fundamental. Our team of Medicare experts can help answer your coverage questions about PSA tests. You never want to overpay for a plan that's not a perfect fit for you.
What is the test for prostate cancer?
The screening test for prostate cancer is known as a PSA test. It’s a simple blood test that you can get during any doctor visit. The PSA test measures prostate-specific antigen (PSA), which is made only by certain cells within the male prostate gland.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
Does Medicare pay for prostate cancer screening?
Medicare Part B pays for one prostate cancer screening test each year. You pay no out-of-pocket cost for a PSA test if your doctor accepts Medicare assignment, and the Part B deductible does not apply. Medicare Advantage plans also cover a yearly PSA test. Check with your plan for coverage details. Talk with your doctor about prostate cancer ...
Does Medicare cover PSA?
Medicare Advantage plans also cover a yearly PSA test. Check with your plan for coverage details. Talk with your doctor about prostate cancer screening. You may hear different ideas about how often men need to have a PSA test so it’s important for you and your doctor to decide what’s best for you.
What Is the Screening Test for Prostate Cancer?
The PSA test is the primary screening test for prostate cancer. To perform the test, a medical professional collects a blood sample and sends it to a lab for analysis. The test measures how much of a substance called prostate-specific antigen is present in the blood.
What Does a High PSA Level Mean?
Healthy cells in the prostate produce limited amounts of prostate-specific antigen. When prostate problems occur, the cells increase production, leading to elevated PSA levels. A high PSA level may indicate:
How Is a Digital Rectal Exam Different From a Prostate-Specific Antigen Test?
A digital rectal exam is when a doctor inserts his finger into your rectum to feel your prostate for signs of enlargement. A prostate-specific antigen test is a blood test that measures how much PSA is present in your blood. Often, doctors use both digital rectal exams and PSA testing to screen for prostate cancer.
What Is the Cost of a PSA Blood Test?
The cost of a PSA blood test varies based on where you live, but the American Board of Internal Medicine Foundation reports that the average cost of the test is $40. Your doctor may charge an additional fee or copayment for the office visit. If your PSA levels are elevated, you are likely to have additional costs for further testing.
Does Medicare Cover a PSA Test?
Medicare Part B usually covers 100% of the cost of annual PSA blood testing for men aged 50 and over. If your doctor assesses additional fees, Medicare Part B typically covers 80% of the costs, leaving you responsible for the remaining 20%. You may also be responsible for a copay.
Does Medicare Pay for Prostate Cancer Screenings?
In addition to paying for the PSA test, Medicare Part B will cover 80% of the cost of annual digital rectal examinations and additional fees assessed by your doctor. You are also likely to be assessed a copay.
At What Age Does Medicare Start Paying for the PSA Test?
For most men, Medicare begins paying for PSA testing at age 50. If your doctor believes that the test is medically necessary due to symptoms you are experiencing or a family history of prostate cancer, Medicare may cover the cost of a PSA test before you turn 50.
Medicare Coverage For Prostate Specific Antigen Test
Medicare will cover prostate-specific antigen tests for those who need it. Prostate cancer is prevalent among men. About one out of every nine men will receive a prostate cancer diagnosis. The blood test is considered a routine screening for beneficiaries. As long as your doctor takes Medicare, you should have coverage.
Personal Stories About Having A Prostate
These stories are based on information gathered from health professionals and consumers. They may be helpful as you make important health decisions.
What Do The Experts Recommend
Experts have set up guidelines to advise men about prostate cancer screening.
What Is The Cost Of A 4kscore Test And Will Insurance Cover It
We often hear from patients and physicians interested in learning more about the cost associated with the 4Kscore test, and whether the test is covered under Medicare, Medicaid or other health insurance plans. This is a confusing area and the answers always vary because of different insurance carriers and plans.
Medical Insurance Coverage For Prostate Cancer
Understanding the benefits provided by your medical insurance is critical as you explore the possible tests and treatments for prostate The prostate is a walnut-sized gland located between the bla… Full Definition cancer Cancer is a group of diseases where cells grow abnormally an… Full Definition.
How Is A Digital Rectal Exam Different From A Prostate
A digital rectal exam is when a doctor inserts his finger into your rectum to feel your prostate for signs of enlargement. A prostate-specific antigen test is a blood test that measures how much PSA is present in your blood. Often, doctors use both digital rectal exams and PSA testing to screen for prostate cancer.
Medicare Advantage And Cancer
If you have Medicare Advantage , this means that youve purchased your Medicare plan from a private insurance company as opposed to getting it directly from the federal government. These types of plans are required to give you the same basic coverages as Original Medicare, but the CMS warns that they can have different rules and costs.
Does Medicare Cover a PSA Test?
Cancer is a disease that is best treated before it spreads. Early stages of prostate cancer may not present signs and symptoms. The initial tests doctors usually perform to detect prostate cancer are the digital rectal exam and prostate specific antigen (PSA) blood test.
PSA blood test
The cells in your prostate gland produce a protein known as PSA. Though mostly found in semen, a lesser amount is found in the blood. If the PSA level in the blood rises, your doctor may suggest a PSA blood test.
How often does Medicare pay for a sex test?
Medicare pays in full (no coinsurances, copays or deductibles) for this test once every two years for people whose doctor or other health care provider prescribed the test because they: Are an estrogen-deficient women who is at risk for osteoporosis based on her medical history and other findings.
How often does Medicare cover blood work?
Medicare covers blood tests every five years to test cholesterol, lipid and triglyceride levels. My note: If you have health issues or are taking drugs to lower your cholesterol, you would have your blood checked more regularly, but those tests would be coded as “diagnostic”, meaning you would have a 20% co-pay.
How much is a Pap smear covered by Medicare?
Pap smear: For women with Medicare who are considered at low risk for cervical or vaginal cancer, Original Medicare covers 100 percent of the cost of one Pap smear every two years (24 months).
How often does Medicare pay for mammograms?
Medicare covers: One baseline mammogram for women 35 to 39 years of age. One screening mammogram every 12 months for women ages 40 and over. Medicare will also pay for both men and women to have diagnostic mammograms more frequently than once a year.
What percentage of Medicare coverage is required for preventive screening?
If an exam is considered diagnostic, Medicare covers 80 percent of the cost and the patient or their supplemental insurance is responsible for the other 20 percent. For a complete list of Medicare preventive screenings go to Medicareinteractive.org preventive screening page.
What is the Medicare screening test for diabetes?
you are 65 years of age or older. The Medicare-covered diabetes screening test includes : a fasting blood glucose tests; and/or. a post-glucose challenge test.
How often do you need to get a diabetes screening?
Diabetes Screening: You are eligible for one Medicare-covered diabetes screening every 12 months if you: have hypertension; have dyslipidemia (any kind of cholesterol problem); have a prior blood test showing low glucose (sugar) tolerance; are obese (body mass index of 30 or more); or. meet at least two of the following:
How often is a PSA test covered by Medicare?
Screening PSA tests are covered at a frequency of once every 12 months for men who have attained age 50 (i.e., starting at least one day after they have attained age 50), if at least 11 months have passed following the month in which the last Medicare-covered screening prostate specific antigen test was performed.
What is a PSA test?
Diagnostic PSA tests are defined as those performed when the patient has signs or symptoms. If a patient has no signs or symptoms of prostate cancer, submit the appropriate code for a screening PSA. If a patient does have signs or symptoms of prostate cancer, submit the appropriate code for a diagnostic PSA.
What is the code for prostate cancer screening?
Screening PSAs. Submit HCPCS code G0103 for screening PSA tests. Medicare coverage for screening PSAs is limited to once every 12 months.
What is prostate specific antigen?
Prostate Specific Antigen (PSA), a tumor marker for adenocarcinoma of the prostate, can predict residual tumor in the post-operative phase of prostate cancer. Three to 6 months after radical prostatectomy, PSA is reported to provide a sensitive indicator of persistent disease.
Does Medicare cover prostate cancer screening?
Medicare allows for coverage of both screening and diagnostic Prostate Specific Antigen (PSA) tests. Screening PSA tests are defined as those that are performed in the absence of signs or symptoms of prostate cancer. Diagnostic PSA tests are defined as those performed when the patient has signs or symptoms.
How is the coverage of a PSA test determined?
The coverage, and subsequent payment, for a PSA test is determined by the contractual agreement with the patient's insurance company. Some insurance companies pay and others do not for procedures and other services with different diagnoses.
Does Medicare pay for PSA test?
If the PSA test is ordered with one of the diagnoses, such as cancer of the prostate, elevated PSA level, etc., Medicare will pay for it any number of times that the test is considered to be medically necessary during the year, but they will not pay for a PSA test for any other diagnoses, other than a "screening" test, as discussed below.
Does Medicare require a 25 modifier?
The simple answer is yes, it is true. For Medicare, you no longer need to use a –25 modifier on an E&M code when billed in conjunction with uroflow (51741–complex uroflowmetry or 51736–simple uroflowmetry). The reason is very simple: Medicare changed the rules.