How do you verify a patient is eligible for Medicare?
The best way to check eligibility and enroll in Medicare online is to use the Social Security or Medicare websites. They are government portals for signing up for Medicare, and they offer free information about eligibility.
How do I find Medicare claims as a provider?
Log into (or create) your secure Medicare account. You'll usually be able to see a claim within 24 hours after Medicare processes it. A notice you get after the doctor, other health care provider, or supplier files a claim for Part A or Part B services in Original Medicare.
How do providers call Medicare?
1-800-MEDICARE (1-800-633-4227)
What are the 3 requirements for Medicare?
You're 65 or older.You are a U.S. citizen or a permanent legal resident who has lived in the United States for at least five years and.You are receiving Social Security or railroad retirement benefits or have worked long enough to be eligible for those benefits but are not yet collecting them.More items...•Nov 15, 2021
How do providers bill Medicare?
Payment for Medicare-covered services is based on the Medicare Physicians' Fee Schedule, not the amount a provider chooses to bill for the service. Participating providers receive 100 percent of the Medicare Allowed Amount directly from Medicare.
What is a Medicare provider?
A Medicare provider is a physician, health care facility or agency that accepts Medicare insurance. Providers earn certification after passing inspection by a state government agency. Make sure your doctor or health care provider is approved by Medicare before accepting services.
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
Who is the best person to talk to about Medicare?
You can make an appointment with a Social Security representative at your local office by calling 1-800-772-1213. You can also call Medicare directly at 1-800-633-4227. Finally, your State Health Insurance Assistance Program (SHIP) provides free counseling and education to help you choose coverage.
Does Medicare call to update information?
The Social Security Administration and Centers for Medicare and Medicaid Services (CMS) do not call customers to update their information. They will never ask for your financial information.Jul 21, 2021
Which of the following customers are eligible for Medicare?
Medicare is the federal health insurance program for: People who are 65 or older. Certain younger people with disabilities. People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
Who is eligible for Medicare Part B reimbursement?
How do I know if I am eligible for Part B reimbursement? You must be a retired member or qualified survivor who is receiving a pension and is eligible for a health subsidy, and enrolled in both Medicare Parts A and B. 2.
Can I get Medicare if I never worked?
You can still get Medicare if you never worked, but it will likely be more expensive. Unless you worked and paid Medicare taxes for 10 years — also measured as 40 quarters — you will have to pay a monthly premium for Part A. This may differ depending on your spouse or if you spent some time in the workforce.
How to Verify Patient Eligibility
Medicare requires providers use self-service technology for inquiries regarding patient eligibility. Our call center staff is not able to respond to these inquiries. Providers can use the WPS Government Health Administrators Portal or our Interactive Voice Response (IVR) system to verify patient eligibility.
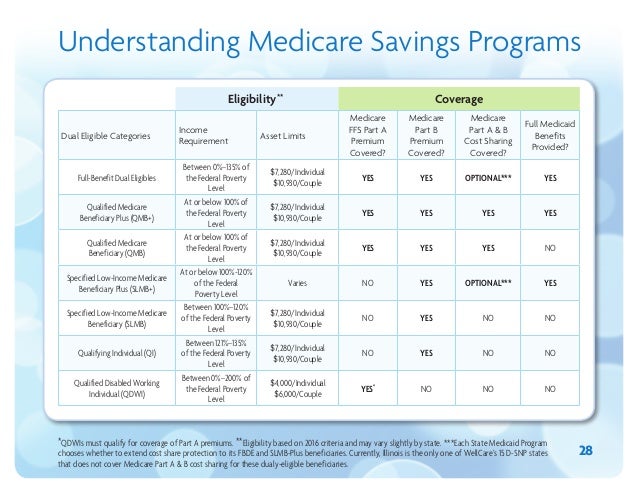
Checking Eligibility for Qualified Medicare Beneficiaries (QMB)
When using the portal or IVR to check eligibility, you will not receive information regarding Medicare applied deductible or coinsurance for patients in the QMB program. The portal will return information explaining the patient is part of the QMB program. For more information on the QMB program, see Qualified Medicare Beneficiary (QMB) Program.
Medicare Secondary Payer (MSP) and Eligibility
Although we process Medicare Secondary Payer (MSP) claims, we do not maintain MSP records. The Benefits Coordination & Recovery Center (BCRC) is responsible for establishing MSP occurrence records on the Common Working File (CWF).
What is Medicare entitlement?
Medicare is a Health Insurance Program for people age 65 or older, certain qualified disabled people under age 65, and people of all ages with end-stage renal disease (ESRD) (permanent kidney failure treated with dialysis or a transplant).
What is a CWF?
Common Working File (CWF) is a system that contains all Medicare beneficiary information as well as claim transactions, which includes Medicare Part A, Part B and Durable Medical Equipment. The Fiscal Intermediary Standard System and Multi-Carrier System processing systems interface with CWF to process claims.
