What is an appeal for Medicare?
This is called an appeal, and you can use it for concerns about each part of Medicare, including: You can use an appeal in a few different situations, such as denial of coverage for a test or service or if you’re charged a late fee you think is in error.
What evidence do I need to appeal a Medicare late enrollment penalty?
Evidence to appeal will include proof of adequate coverage comparable with that of Medicare Part B or Part D. Learn more about Medicare late enrollment penalties here. Here is another example: Medicare assesses a person’s income as reported on their tax return from 2 years ago to calculate the Medicare Part B and Part D premiums.
How long do you have to appeal a Medicare denial?
You have 120 days from a Medicare denial or penalty to file an appeal. Medicare will let you know in writing if your coverage has been denied or you’ve been assessed a penalty. The notice you’ll receive will let you know the steps you can take to file an appeal.
How do you appeal a medical malpractice case?
People should include as much supporting information as possible with the appeal. Information from doctors, healthcare providers, or suppliers can help toward getting a favorable decision. If waiting for a decision would affect a person’s health, they can ask for a fast appeal.
How long does Medicare have to respond to an appeal?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 days. Payment request—60 days.
What should I say in a Medicare appeal?
What are the steps for filing an appeal for original Medicare?your name and address.your Medicare number (as shown on your Medicare card)the items you want Medicare to pay for and the date you received the service or item.the name of your representative if someone is helping you manage your claim.More items...•
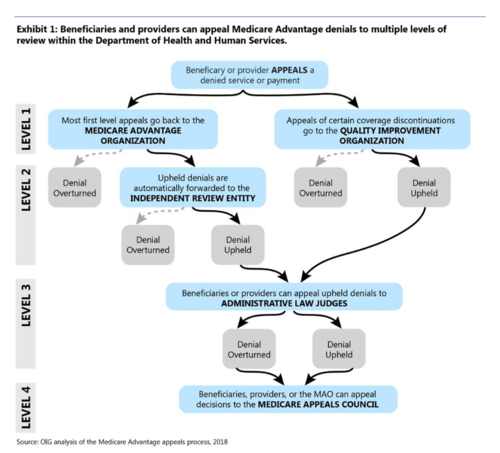
How many steps are there in the Medicare appeal process?
The appeals process has 5 levels. If you disagree with the decision made at any level of the process, you can generally go to the next level. At each level, you'll get instructions in the decision letter on how to move to the next level of appeal.
What are the five levels for appealing a Medicare claim?
The Social Security Act (the Act) establishes five levels to the Medicare appeals process: redetermination, reconsideration, Administrative Law Judge hearing, Medicare Appeals Council review, and judicial review in U.S. District Court. At the first level of the appeal process, the MAC processes the redetermination.
Who pays if Medicare denies a claim?
The denial says they will not pay. If you think they should pay, you can challenge their decision not to pay. This is called “appealing a denial.” If you appeal a denial, Medicare may decide to pay some or all of the charge after all.
Who has the right to appeal denied Medicare claims?
You have the right to appeal any decision regarding your Medicare services. If Medicare does not pay for an item or service, or you do not receive an item or service you think you should, you can appeal. Ask your doctor or provider for a letter of support or related medical records that might help strengthen your case.
Which of the following are reasons a claim may be denied?
Here are the top 5 reasons why claims are denied, and how you can avoid these situations.Pre-Certification or Authorization Was Required, but Not Obtained. ... Claim Form Errors: Patient Data or Diagnosis / Procedure Codes. ... Claim Was Filed After Insurer's Deadline. ... Insufficient Medical Necessity. ... Use of Out-of-Network Provider.
Which of the following is the highest level of the appeals process of Medicare?
The levels are: First Level of Appeal: Redetermination by a Medicare Administrative Contractor (MAC) Second Level of Appeal: Reconsideration by a Qualified Independent Contractor (QIC) Third Level of Appeal: Decision by the Office of Medicare Hearings and Appeals (OMHA)
What are the four levels of appeals?
There are four stages to the appeal process — reconsideration, hearing, council, and court.
What is the difference between reconsideration and redetermination?
Any party to the redetermination that is dissatisfied with the decision may request a reconsideration. A reconsideration is an independent review of the administrative record, including the initial determination and redetermination, by a Qualified Independent Contractor (QIC).
What is the purpose of the appeals process is it an effective process?
The first thing to understand is what the purpose of the appeals process actually is. Rather than being a re-trying of your case, it is a judicial review of the decision of the trial court that heard it initially. A judge will review all the relevant facts and determine if a harmful legal error occurred.
How many Medicare appeals are there?
5 appeal levelsThis booklet tells health care providers about Medicare's 5 appeal levels in Fee-for-Service (FFS) (original Medicare) Parts A & B and includes resources on related topics.
How many levels of appeal are there for Medicare?
There are five levels of appeal for services under original Medicare, and your claim can be heard and reviewed by several different independent organizations. Here are the levels of the appeal process: Level 1. Your appeal is reviewed by the Medicare administrative contractor. Level 2.
What happens if Medicare Appeals Council isn't in your favor?
If the decision of the Medicare Appeals Council isn’t in your favor, you can present your case to a judge in federal district court. The amount of money you’re asking Medicare to pay must meet a set amount to proceed with an appeal in court.
What to do if Medicare won't pay for your care?
If Medicare won’t cover your care, you can start the appeals process then. Pay for your continued care out of pocket.
What is the Medicare number?
your Medicare number (as shown on your Medicare card) the items you want Medicare to pay for and the date you received the service or item. the name of your representative if someone is helping you manage your claim. a detailed explanation of why Medicare should pay for the service, medication, or item.
How long does it take for Medicare to issue a decision?
The Office of Medicare Hearings and Appeals should issue a decision in 90 to 180 days. If you don’t agree with the decision, you can apply for a review by the Medicare Appeals Council.
What happens if Medicare refuses to pay for medical care?
If Medicare refuses to cover care, medication, or equipment that you and your healthcare provider think are medically necessary, you can file an appeal. You may also wish to file an appeal if Medicare decides to charge you with a late enrollment penalty or premium surcharge.
How to communicate with Medicare?
If you communicate with Medicare in writing, name your representative in the letter or e-mail. Know that you can hire legal representation. If your case goes beyond an initial appeal, it may be a good idea to work with a lawyer who understands Medicare’s appeals process so your interests are properly represented.
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
Here is a bit of information that you might find helpful if you are on Medicare and about to get inappropriately discharged from the hospital
If you are on Medicare, then you can stay in the hospital only if there is a good medical reason.
When you call, you or your representative must be available to discuss the case. You may also submit written evidence to back your appeal
The BFCC-IO then contacts the hospital, which is required to issue a detailed notice containing your case facts and the applicable Medicare coverage rule . The burden is on the hospital, not you, to produce evidence to support the discharge.
The takeaway? A Medicare appeal may buy you 1 or 2 extra days, but the chances of winning are slim
Virginia Hammerle, Managing Attorney for Hammerle Finley Law Firm, has been recognized from 2012-2018 as a Super Lawyer, a Thompson Reuters Publication. See hammerle.com for her blog and newsletter sign-up. This column does not constitute legal advice.
What is a fast appeal?
If waiting for a decision would affect a person’s health, they can ask for a fast appeal. An example of the need for a fast decision might be if someone is an inpatient in a hospital or SNF and they are concerned that the facility is discharging them too soon.
What happens if Medicare denies coverage?
If Medicare denies coverage of an item or service, an individual has the right to appeal the decision. People must provide proof with a claim and submit this to Medicare with an application form.
Why do you appeal Medicare?
Reasons for appeal. Appeals process. Takeaway. You’ll receive a notice when Medicare makes any decisions about your coverage. You can appeal a decision Medicare makes about your coverage or price for coverage. Your appeal should explain why you don’t agree with Medicare’s decision. It helps to provide evidence that supports your appeals case ...
What is Medicare appeal?
It helps to provide evidence that supports your appeals case from a doctor or other provider. There might be times when Medicare denies your coverage for an item, service, or test. You have the right to formally disagree with this decision and encourage Medicare to change it. This process is called a Medicare appeal.
Why is Medicare denying my coverage?
There are a few reasons Medicare might deny your coverage, including: Your item, service, or prescription isn’t medically necessary.
What is a fast appeal?
In a few cases, you’ll file what’s called a fast appeal. Fast appeals apply when you’re notified that Medicare will no longer cover care that’s: at a hospital. at a skilled nursing facility. at a rehabilitation facility. in hospice.
How long does it take to get a decision from Medicare?
You’ll hear a decision about your appeal within 60 days.
What is level 3 appeal?
At level 3, you’ll have the chance to present your case to a judge. You’ll need to fill out a request form detailing why you disagree with your level 2 decision. Your appeal will only be elevated to level 3 if it reaches a set dollar amount. Office of Medicare Hearings and Appeals review.
How many levels of appeals are there?
The appeals process has five levels. Each level is a different review process with a different timetable. You’ll need to request an appeal at each level. If your appeal is successful at the first level, or if you agree with Medicare’s reasoning for denying your appeal, you can stop there. However, if your appeal was denied ...
What to do if you decide to appeal a health care decision?
If you decide to file an appeal, ask your doctor, health care provider, or supplier for any information that may help your case. If you think your health could be seriously harmed by waiting for a decision about a service, ask the plan for a fast decision.
What happens if my Medicare plan doesn't decide in my favor?
Then, if your plan doesn't decide in your favor, the appeal is reviewed by an independent organization that works for Medicare, not for the plan.
Why do people file an appeal for Medicare?
People may file an appeal for several reasons, including when Medicare, a health plan, or drug plan makes a decision that results in denial of a request for any of the following: to cover or pay for a piece of durable medical equipment (DME), healthcare service, or medication. to change the fee that an individual must pay for DME, ...
What is an appeal in Medicare?
Other program appeals. Winning an appeal. Summary. A person may appeal when Medicare makes a decision that denies coverage of any service. They may have a better chance of winning an appeal if they gather and include supporting information from a doctor or healthcare provider. The appeal process involves five levels.
How to file an appeal against a Medicare decision?
To file an appeal against an original Medicare decision, a person can complete a Redetermination Request Form and mail it to the company listed in the Appeals Information part of the MSN. Another method is to mail a written request to the company with the following information: the individual’s name, address, and Medicare number.
How long does it take to appeal a Medicare denial?
The deadline for filing is 60 days from the denial date. They should include the same information required for an original Medicare appeal.
What is Medicare Advantage?
Medicare Advantage is the alternative to original Medicare and provides at least the same coverage as original Medicare parts A and B. Advantage plans may also include prescription drug coverage and extra benefits such as dental care.
How often does Medicare get a summary notice?
A person enrolled in original Medicare — parts A and B — gets a Medicare Summary Notice (MSN) form every 3 months. The MSN lists the services or items that providers billed to Medicare and the amount Medicare paid for each.
How long does it take for Medicare to decide to cover a service?
Decision. In all other cases, a person is usually informed of the decision within 60 days of the appeal date. If Medicare decides to cover the service, it will appear on the individual’s next MSN. Learn more about original Medicare here.
