
Why is Medicare considered so helpful?
Medicare is considered helpful because it covers so many people. Medicare Costs Very Little Every Month Many Medicare enrollees qualify for premium -free Part A but must pay a small, out-of-pocket amount every month for Part B.
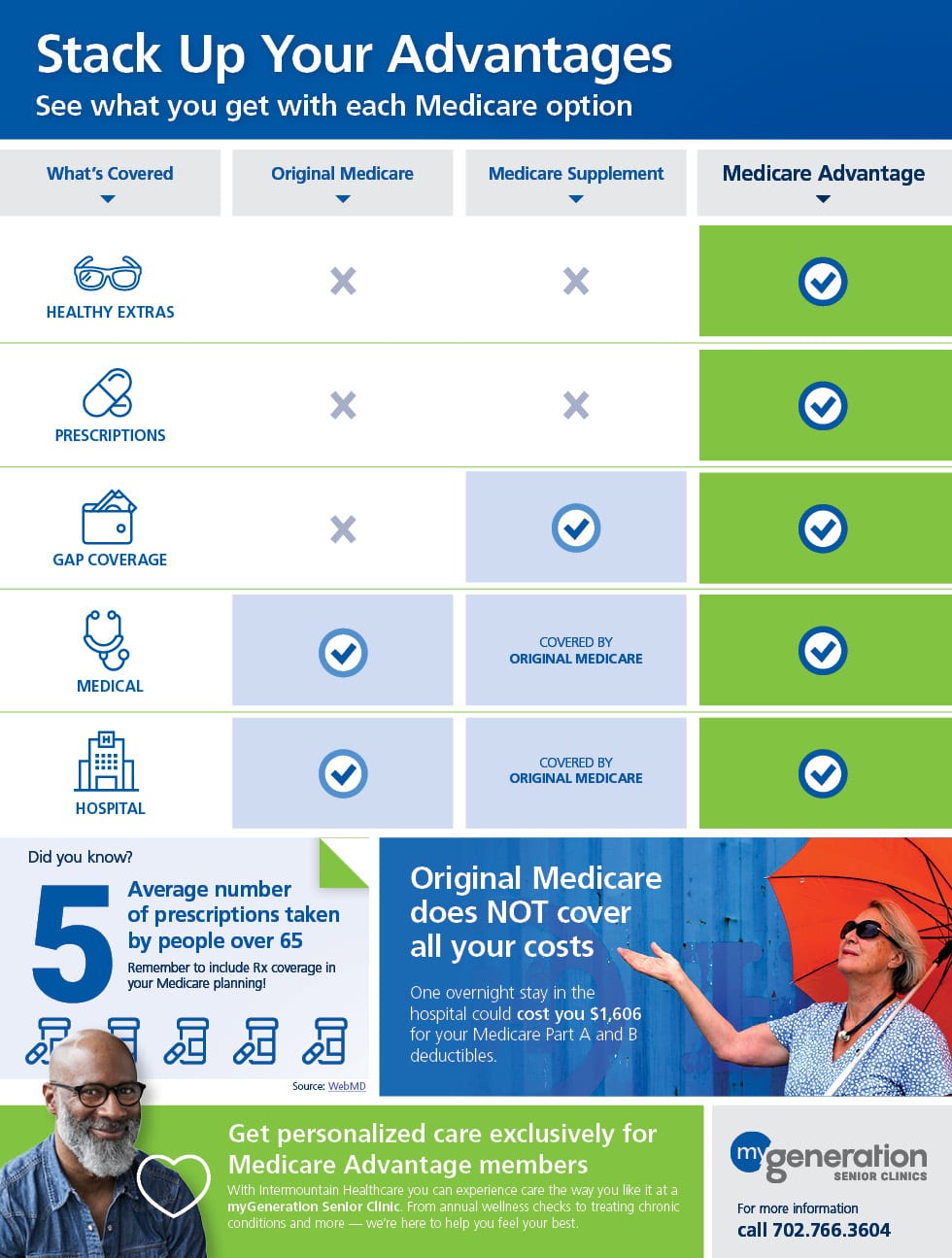
What benefits do you get with Medicare Advantage?
You get all the Medicare program benefits of Part A hospital insurance and Part B medical insurance, together known as Original Medicare,* when you enroll in Medicare Advantage. Plus, many Medicare Advantage plans can also provide additional benefits (dental, vision, hearing, etc.) at a minimal cost.
How does Medicare work?
In many senses, Medicare works. Thanks to the program, millions of aging adults have been able to receive coverage. Medicare also covers many younger Americans with disabilities. Medicare is considered helpful because it covers so many people.
How does Medicare improve health care delivery?
It is pushing for better delivery of health care, with initiatives to improve quality and coordination, prevent avoidable readmissions to the hospital and reduce infections caught while at the hospital. Increasingly, it is paying doctors and hospitals for quality of care rather than the volume of services. Medicare works efficiently.
Is Medicare an in Kind program?
Defining In-Kind Benefits One example of a U.S. in-kind transfer program is Medicare, which subsidizes health care for senior citizens and the disabled. Veterans' benefits and Stafford student loans are other examples.
What is the main benefit of Medicare Part A?
What Part A covers. Medicare Part A hospital insurance covers inpatient hospital care, skilled nursing facility, hospice, lab tests, surgery, home health care.
What is a benefit in Medicare?
The way that Original Medicare measures your use of hospital and skilled nursing facility (SNF) services. A benefit period begins the day you're admitted as an inpatient in a hospital or SNF. The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row.
Is Medicare always the primary insurance?
If you don't have any other insurance, Medicare will always be your primary insurance. In most cases, when you have multiple forms of insurance, Medicare will still be your primary insurance.
What is the difference between Medicare Part A and B?
If you're wondering what Medicare Part A covers and what Part B covers: Medicare Part A generally helps pay your costs as a hospital inpatient. Medicare Part B may help pay for doctor visits, preventive services, lab tests, medical equipment and supplies, and more.
What is Medicare Part A and B mean?
Part A provides inpatient/hospital coverage. Part B provides outpatient/medical coverage. Part C offers an alternate way to receive your Medicare benefits (see below for more information). Part D provides prescription drug coverage.
What is the Medicare Part A benefit period?
In Medicare Part A, which is hospital insurance, a benefit period begins the day you go into a hospital or skilled nursing facility and ends when you have been out for 60 days in a row. If you go back into the hospital after 60 days, then a new benefit period starts, and the deductible happens again.
What is not covered under Medicare Part A?
Medicare Part A will not cover long-term care, non-skilled, daily living, or custodial activities. Certain hospitals and critical access hospitals have agreements with the Department of Health & Human Services that lets the hospital “swing” its beds into (and out of) SNF care as needed.
What is Part A Medicare coverage?
Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. coverage if you or your spouse paid Medicare taxes for a certain amount of time while working. This is sometimes called "premium-free Part A." Most people get premium-free Part A.
Is it better to have Medicare as primary or secondary?
Medicare is always primary if it's your only form of coverage. When you introduce another form of coverage into the picture, there's predetermined coordination of benefits. The coordination of benefits will determine what form of coverage is primary and what form of coverage is secondary.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
Can I have Medicare and private insurance at the same time?
It is possible to have both private insurance and Medicare at the same time. When you have both, a process called “coordination of benefits” determines which insurance provider pays first. This provider is called the primary payer.
Why is Medicare important?
Medicare is useful because it covers so many people.
What is the purpose of Medicare and Medicaid?
With the creation of Medicaid and Medicare, Congress created a set of standards for hospital enrollment in the programs. As time went on, the government became more involved in overseeing these standards and now requires public reporting on things such as hospital infection rates and readmissions.
What is Medicare Part D?
The addition of Medicare Part D Prescription Drug Plans and Medicare Advantage Prescription Drug Plans—both sold through private insurance companies—also gave Americans wider access to prescription medicines. Medicare beneficiaries have had access to these plans since 2006, and enrollments have increased every year since.
How much does Medicare cost per month?
This number is estimated to cost around $135.50 per month. When you compare this to the out-of-pocket cost of operations, prescriptions, and other associated costs, the savings are huge.
How many people were on Medicare in 2006?
In 2006, 22.5 million (52%) people on Medicare were enrolled in Part D compared to 43 million (72%) in 2018, according to the Kaiser Family Foundation. With millions of Americans receiving Medicare prescription drug benefits, this may have given pharmaceutical companies more opportunities to develop drugs for this market.
How much does Medicare cost?
Medicare Costs a Huge Amount to Administrate. In 2018, Medicare spending totaled $731 billion. Currently, that’s approximately 15% of the overall federal budget. That number isn’t expected to get smaller, with many estimating that the percentage will go up to around 18% over the next decade.
Does Medicare offer preventive care?
Granted, Medicare does offer a significant number of free preventive programs to enrollees that can cut down on health problems. Many of the individuals on Medicare suffer from preventive conditions (particularly before the implementation of ACA).
What happens if you increase your earnings by 1?
At a notch, a household that increases earnings by $1 may lose much more than $1 in benefits when the value of in-kind benefits is correctly accounted for (see Blundell and MaCurdy 1999 for some important examples).
Why do governments want to target transfers to the needy?
A popular economic justification for in-kind transfers is based on the idea that governments want to target transfers to the needy for efficiency reasons, but that they cannot accurately identify the poor. Hence the government must rely on individuals to self-identify as needy.
Do elderly people count as beneficiaries?
For one thing, many programs count the elderly as their primary beneficiaries , even though most elderly are no longer participating in the labour market. And there are many examples of in-kind programs that discourage labour supply by creating large “notches” in budget constraints.
How does Medicare help?
It is pushing for better delivery of health care, with initiatives to improve quality and coordination, prevent avoidable readmissions to the hospital and reduce infections caught while at the hospital.
Why is the Medicare program important?
And it helps insulate beneficiaries from rising health care costs. People enrolled in the program may still pay thousands of dollars a year for health care, but their access to health care is vastly better than before the program existed.
What is Medicare for older people?
Medicare is a lifeline that puts health care in reach of millions of older Americans. But it does much more: By helping older Americans stay healthy and independent, Medicare eases a potential responsibility for younger family members. Knowledge that Medicare's protections will be there when needed brings peace of mind to people as they get older. ...
When was Medicare enacted?
When Medicare was enacted in 1965 nearly 1 in 3 seniors lived in poverty. Older people were more likely to be poor than any other age group. Yet in its first 10 years, Medicare helped cut their poverty rate in half.
Does Medicare pay for hospice?
Finally, for the terminally ill, Medicare offers a hospice benefit that helps individuals get compassionate, end-of-life care, typically in their own home. Medicare can lead the way to better care for everyone.
Does Medicare cover health insurance?
Here are some of the many ways Medicare matters: Medicare guarantees affordable health insurance. Before Medicare, almost 1 in 2 older Americans had no health insurance and faced a bleak future if they got seriously ill.
What is Medicare benefit period?
Medicare benefit periods mostly pertain to Part A , which is the part of original Medicare that covers hospital and skilled nursing facility care. Medicare defines benefit periods to help you identify your portion of the costs. This amount is based on the length of your stay.
How long does Medicare Advantage last?
Takeaway. Medicare benefit periods usually involve Part A (hospital care). A period begins with an inpatient stay and ends after you’ve been out of the facility for at least 60 days.
How much coinsurance do you pay for inpatient care?
Days 1 through 60. For the first 60 days that you’re an inpatient, you’ll pay $0 coinsurance during this benefit period. Days 61 through 90. During this period, you’ll pay a $371 daily coinsurance cost for your care. Day 91 and up. After 90 days, you’ll start to use your lifetime reserve days.
How long does Medicare benefit last after discharge?
Then, when you haven’t been in the hospital or a skilled nursing facility for at least 60 days after being discharged, the benefit period ends. Keep reading to learn more about Medicare benefit periods and how they affect the amount you’ll pay for inpatient care. Share on Pinterest.
What facilities does Medicare Part A cover?
Some of the facilities that Medicare Part A benefits apply to include: hospital. acute care or inpatient rehabilitation facility. skilled nursing facility. hospice. If you have Medicare Advantage (Part C) instead of original Medicare, your benefit periods may differ from those in Medicare Part A.
Why is it important to check deductibles each year?
It’s important to check each year to see if the deductible and copayments have changed, so you can know what to expect. According to a 2019 retrospective study. Trusted Source. , benefit periods are meant to reduce excessive or unnecessarily long stays in a hospital or healthcare facility.
How much is Medicare deductible for 2021?
Here’s what you’ll pay in 2021: Initial deductible. Your deductible during each benefit period is $1,484. After you pay this amount, Medicare starts covering the costs. Days 1 through 60.
How many people will have Medicare Advantage in 2020?
People who enroll in Medicare Advantage pay their Part B premium and whatever the premium is for their Medicare Advantage plan, and the private insurer wraps all of the coverage into one plan.) About 24 million people had Medicare Advantage plans in 2020, and CMS projects that it will grow to 26 million in 2021.
When will Medicare Part D change to Advantage?
Some of them apply to Medicare Advantage and Medicare Part D, which are the plans that beneficiaries can change during the annual fall enrollment period that runs from October 15 to December 7.
What is the maximum out of pocket limit for Medicare Advantage?
The maximum out-of-pocket limit for Medicare Advantage plans is increasing to $7,550 for 2021. Part D donut hole no longer exists, but a standard plan’s maximum deductible is increasing to $445 in 2021, and the threshold for entering the catastrophic coverage phase (where out-of-pocket spending decreases significantly) is increasing to $6,550.
What is the Medicare premium for 2021?
The standard premium for Medicare Part B is $148.50/month in 2021. This is an increase of less than $4/month over the standard 2020 premium of $144.60/month. It had been projected to increase more significantly, but in October 2020, the federal government enacted a short-term spending bill that included a provision to limit ...
How much is the Medicare coinsurance for 2021?
For 2021, it’s $371 per day for the 61st through 90th day of inpatient care (up from $352 per day in 2020). The coinsurance for lifetime reserve days is $742 per day in 2021, up from $704 per day in 2020.
What is the income bracket for Medicare Part B and D?
The income brackets for high-income premium adjustments for Medicare Part B and D will start at $88,000 for a single person, and the high-income surcharges for Part D and Part B will increase in 2021. Medicare Advantage enrollment is expected to continue to increase to a projected 26 million. Medicare Advantage plans are available ...
How long is a skilled nursing deductible?
See more Medicare Survey results. For care received in skilled nursing facilities, the first 20 days are covered with the Part A deductible that was paid for the inpatient hospital stay that preceded the stay in the skilled nursing facility.
Why are in-kind programs considered paternalistic?
On the other hand, in-kind programs have sometimes been deemed “paternalistic” because they dictate that people spend assistance money on things governments deem most necessary. Nevertheless, the vast majority of federal and state assistance programs are in the form of in-kind benefits.
Why are cash transfers better than in-kind?
Through various pieces of research, economists have consistently found that cash transfers make the recipients happier than in-kind benefits. A lot of this is due to freedom of choice. An individual who receives unemployment benefits, for instance, is free to spend that money in any way, whether by defraying immediate living expenses ...
What is in-kind transfer?
An in-kind transfer is also a type of public spending to help specific populations. Unlike a cash transfer, it takes the form of specific goods and services, which recipients get for free or at a reduced rate. One example of a U.S. in-kind transfer program is Medicare, which subsidizes health care for senior citizens and the disabled.
What is Medicare Advantage Plan?
Medicare Advantage plans offer the same coverage as Original Medicare Part A and Part B, but these plans typically include additional benefits and possibly reduced costs on things like premiums and co-pays. You can usually enroll in a Medicare Advantage plan at any time after reaching Medicare eligibility without penalty, but delaying this type of coverage plan could mean that you end up paying more than you need to for healthcare expenses without the additional coverage afforded by a Medicare Advantage plan.
Why is Medicare Part A delayed?
Delaying Medicare Part A. Medicare Part A helps pay for inpatient treatment in a hospital or skilled nursing facility. This type of coverage is automatic for most people if they meet the criteria, become eligible due to age or disability, and have worked for 10 years.
Does Medicare cover injectables?
It does not cover injectable drugs or other forms of medications that must be administered by a healthcare professional in a clinic or care facility.
Can you delay Medicare coverage?
Enrolling in Medicare is something that most people will do at some point, and the benefits of being a Medicare recipient are numerous; however, there may be some reasons to delay coverage that actually work out in your favor. Delaying enrollment can also be detrimental in some situations, so it pays to be informed as to what your options are.
Is MA the same as Medicare?
Additionally, although MA plans include the same coverage as Medicare Part A and Part B coverage, there may be differences in how prescription coverage is treated compared to Original Medicare Part D. Compare drug plans before enrolling as costs and coverage can vary.
Does Medicare Part B require a monthly premium?
This type of coverage does require a monthly premium in order to stay enrolled, so if you currently have healthcare insurance provided by an employer or your own private insurance policy, delaying enrollment means you will not have to pay the monthly premium. Keep in mind that you can have both employer-sponsored healthcare insurance and Medicare at the same time.
