Can you get Medicare Part B while still employed?
Can you add Medicare Part B at any time?
How do you pay for Medicare Part B if you are not collecting Social Security?
Can you get Medicare while working?
How long does it take for Medicare Part B to go into effect?
Do you have to enroll in Medicare Part B every year?
Is Medicare Part B premium automatically deducted from Social Security?
Are you automatically enrolled in Medicare if you are on Social Security?
Does Medicare come out of your Social Security check?
How does working affect Medicare?
What documents do I need to apply for Medicare?
- your Social Security number.
- your date and place of birth.
- your citizenship status.
- the name and Social Security number of your current spouse and any former spouses.
- the date and place of any marriages or divorces you've had.
How long before you turn 65 do you apply for Medicare?
It lasts for 7 months, starting 3 months before you turn 65, and ending 3 months after the month you turn 65. My birthday is on the first of the month.
What happens if you don't sign up for Part A and Part B?
If you don’t sign up for Part A and Part B, your job-based insurance might not cover the costs for services you get.
When do you need to sign up for Medicare?
If the employer has less than 20 employees: You might need to sign up for Medicare when you turn 65 so you don’t have gaps in your job-based health insurance. Check with the employer.
What is a Medicare leave period?
A period of time when you can join or leave a Medicare-approved plan.
Does Medicare work if you are still working?
If you (or your spouse) are still working, Medicare works a little differently. Here are some things to know if you’re still working when you turn 65.
Does private insurance pay for services?
Some private insurance has rules that lower what they pay (or don’t pay at all) for services you get if you’re eligible for other coverage, like Medicare.
Do you have to tell Medicare if you have non-Medicare coverage?
Each year, your plan must tell you if your non-Medicare drug coverage is creditable coverage. Keep this information — you may need it when you’re ready to join a Medicare drug plan.
When do you have to enroll in Medicare Part B?
When You Must Enroll in Medicare Part B. You may be required to get Medicare Part B even when you’re still working. There are two situations in which you must get Part B when you turn 65. If your employer has fewer than 20 employees. If you’re covered by a spouse’s employer, and the employer requires covered dependents to enroll in Medicare ...
How much does Medicare Part B cost?
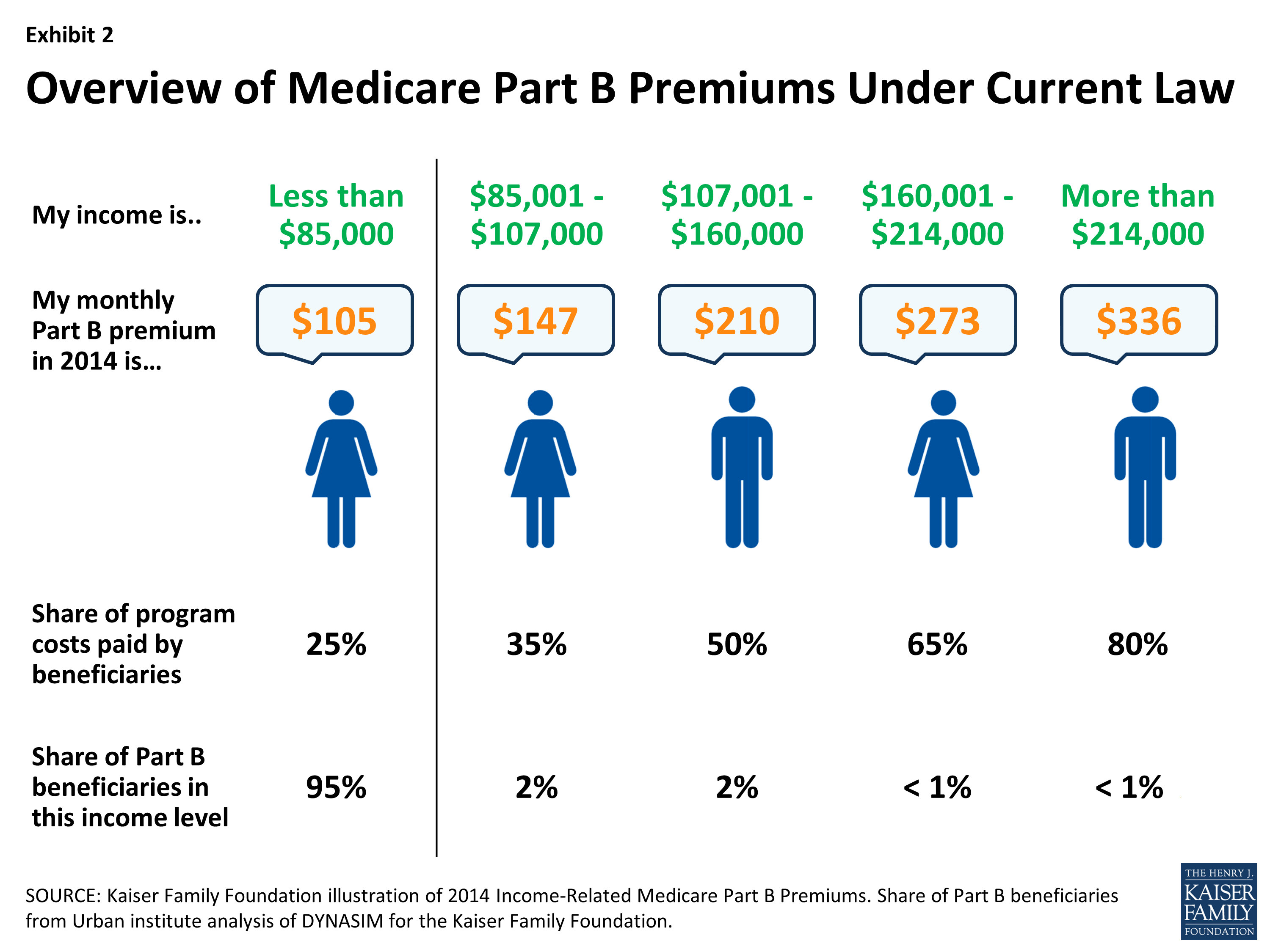
Part B is different. Unlike Part A, Medicare Part B has a monthly premium, which can cost $148.50 to $504.90 depending on income. It has a late enrollment penalty for anybody who enrolls without qualifying for a Special Enrollment Period.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
How long does it take to enroll in Medicare if you lose your employer?
When you lose your employer coverage, you will get an 8-month Special Enrollment Period during which to enroll in Medicare Part B, and Part A if you haven’t done so already. You’ll also be able to enroll in a Medicare Advantage (Part C) plan or Part D prescription drug plan in the first two months of this period.
Where does the dollar sign move in the HSA?
Another stippled circle labeled "Qualified Health Expense" appears to the right. The dollar sign now moves from the HSA circle toward the stippled circle and floats over it.
When do dependents have to enroll in Medicare?
If you’re covered by a spouse’s employer, and the employer requires covered dependents to enroll in Medicare when they turn 65. If you’re not married but living in a domestic partnership and are covered by your partner’s employer health insurance.
Can you build up balances in HSA?
PHIL: So you can build up some pretty big balances in an HSA, and I've actually advised people in some settings to not use their HSA.
When will Social Security enroll you in Part A and Part B?
If you are, Social Security will automatically enroll you in Part A and Part B just before your 65th birthday. The letter sent to you with your Medicare card explains your right to opt out of Part B if you have employer insurance. To opt out, follow the instructions included in that letter within the specified deadline.
How long do you have to sign up for Part B?
When you eventually retire, or leave work, you'll be entitled to a special enrollment period of eight months to sign up for Part B without incurring a late penalty. This also applies to most people who are covered beyond age 65 by insurance from the employer of their working spouse. It also applies to same-sex married couples, ...
When do you have to enroll in Part D?
Your employer plan can tell you whether it's creditable or not. If it's not, you would need to enroll in Part D during your initial enrollment period at age 65 to avoid late penalties if and when you eventually signed up.
Can you delay Part B enrollment?
It's confusing, but different rules apply to Part B and Part D in either of these situations: Part B: You can delay Part B enrollment without penalty only while you or your spouse is still actively working for the employer that provides your health insurance.
Is Medicare primary or secondary?
If so, Medicare would become your primary coverage (meaning it pays bills first) and the employer coverage would be secondary. In this case, you need to find out exactly how the employer plan will work with Medicare. If you are in an unmarried domestic partnership (same sex or opposite sex) and receive health insurance under your partner’s employer ...
Can I draw on my health savings account?
You can draw on funds already in your account, but you cannot add to them. For details, see "Can I Have a Health Savings Account as Well as Medicare?". You'll be able to sign up for Part A without risking a late penalty during the same special enrollment period when you enroll in Part B, after you finally stop working.
Do you have to take Medicare at age 65?
By law, people who continue to work beyond age 65 still must be offered the same health insurance benefits (for themselves and their dependents) as younger people working for the same employer. So your employer cannot require you to take Medicare when you turn 65 or offer you a different kind of insurance — for example, ...
What happens if you don't sign up for Part B?
If you don’t sign up for Part B during your IEP, you can sign up during the GEP. The GEP runs from January 1 through March 31 of each year. If you sign up during a GEP, your Part B coverage begins July 1 of that year. You may have to pay a late enrollment penalty if you sign up during the GEP. The cost of your Part B premium will go up 10% for each 12-month period that you could have had Part B but didn’tsign up. You may have to pay this late enrollment penalty aslong as you have Part B coverage.
How long do you have to be a SEP?
You have a SEP if you were volunteering outside of the United States for at least 12 months for a tax-exempt organization and had health insurance (through the organization) that provided coverage for the duration of the volunteer service.
What happens if you don't have Part B insurance?
If you don’t, your employer’s group plan can refuse to pay your claims. Your insurance might cover claims even if you don’t have Part B, but we always recommend enrolling in Part B. Your carrier can change that at any time, with no warning, leaving you responsible for outpatient costs.
What determines if you are a primary or secondary employer for Medicare?
The size of your employer will determine how your Medicare benefits will coordinate with your employer coverage. If you’re aging into Medicare while working for an employer with over 20 employees, your group plan is primary and Medicare secondary.
What happens if you leave Medicare without a creditable coverage letter?
Without creditable coverage during the time you’ve been Medicare-eligible, you’ll incur late enrollment penalties. When you leave your group health coverage, the insurance carrier will mail you a creditable coverage letter. You’ll need to show this letter to Medicare to protect yourself from late penalties.
How many employees are eligible for creditable insurance?
For your outpatient and medication insurance, a plan from an employer with over 20 employees is creditable coverage. This safeguards you from having to pay late enrollment penalties for Part B and Part D, respectively.
Can you drop your Medicare coverage at 65?
An employer can never force you to drop your group coverage and enroll in Medicare once you turn 65. You can always choose to have Medicare and decline your group plan, but your employer can never force that decision.
Is Medicare billed first or second?
If your employer has fewer than 20 employees, then Medicare becomes primary. This means Medicare is billed first, and your employer plan will be billed second. If you have small group insurance, it’s HIGHLY recommended that you enroll in both Parts A and B as soon as you’re eligible. If you don’t, your employer’s group plan can refuse ...
Is it better to have Medicare and employer insurance?
It can be beneficial for some to have both Medicare and employer insurance. In other cases, taking Medicare could make more sense than holding onto an employer’s policy. First, we’ll explain how employer coverage works with Medicare.
When do you have to enroll in Medicare?
If you work for a smaller employer, you must enroll in Part A and Part B when you turn 65, and then Medicare pays claims first and your employer plan becomes your secondary insurance. Medicare has strict enrollment rules that affect people differently according to their circumstances.
How much does Medicare premium increase if you don't sign up?
(See "When Does the Part B Late Penalty Clock Start Ticking?" ) If you don't sign up within your initial enrollment period or a special enrollment period (whichever is appropriate to you), your monthly premium will permanently increase 10 percent for each 12-month period you were eligible but did not enroll.
When does the eight month special enrollment period start?
The eight-month special enrollment period starts at the end of the month in which you stop working or lose your employer insurance, whichever is first. Generally, people eligible for Social Security benefits do not pay for Part A.
How much does a premium increase for a 12 month period?
If you don't sign up within your initial enrollment period or a special enrollment period (whichever is appropriate to you), your monthly premium will permanently increase 10 percent for each 12-month period you were eligible but did not enroll.