Full Answer
How do I become a Medicare supplier?
The most important step to becoming a supplier is to obtain DME accreditation. To do that, you have to comply with the supplier standards set for the Medicare program, as well as with the defined quality standards.
What makes a good Medicare contract supplier?
All Medicare contract suppliers have to meet the Competitive Bidding Program requirements, federal quality standards, and state licensure requirements. They also have to be in good standing with Medicare, and be accredited by an independent accreditation organization.
How do I apply for Medicare as a DMEPOS supplier?
The NSC processes all Medicare applications for DMEPOS suppliers. You can check in with the NSC regarding your enrollment status. Contact the NSC. DMEPOS suppliers are required to post a surety bond in the amount of $50,000 for each NPI they maintain. Post a Surety Bond. It’s important to keep your enrollment information up to date.
What are the requirements for the Medicare competitive bidding program?
All Medicare contract suppliers have to meet the Competitive Bidding Program requirements, federal quality standards, and state licensure requirements. They also have to be in good standing with Medicare, and be accredited by an independent accreditation organization. Medicare contract suppliers must:
How do you get a Medicare product approved?
Go to an in-person doctor visit, where your doctor will write an order for the DME. Take the order to a Medicare-approved DME supplier. Depending on the product, ask the supplier if they will deliver it to your home. Find out if Medicare requires prior authorization for your DME.
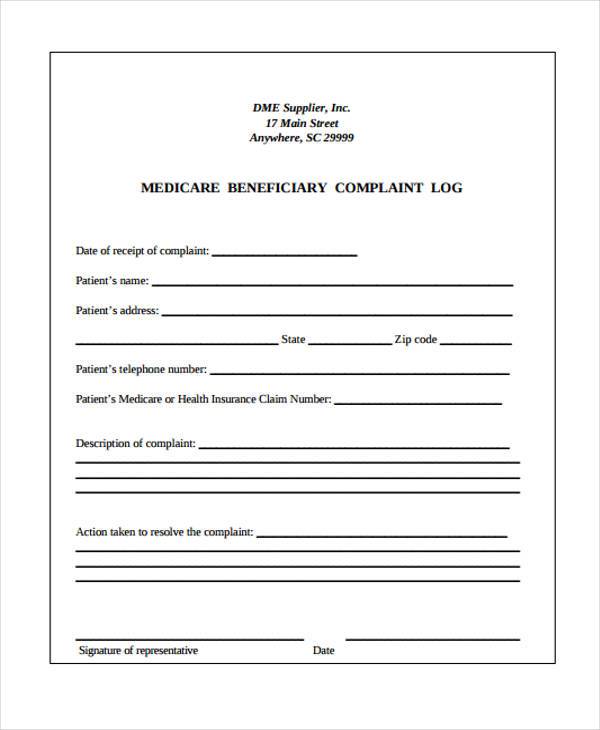
What is a Medicare Dmepos supplier?
DMEPOS stands for durable medical equipment, prosthetics, orthotics and supplies. Page 2. DMEPOS supplier means an entity or individual, including a physician or a Part A provider, which sells or rents Part B covered items to Medicare beneficiaries and which meets the standards in paragraphs (c) and (d) of this section ...
What is a supplier under Medicare?
Supplier is defined in 42 CFR 400.202 and means a physician or other practitioner, or an entity other than a provider that furnishes health care services under Medicare.
What does it mean to be credentialed with Medicare?
Credentialing is the process of approving a physician, agency or other medical provider as part of the Medicare supply chain.
Can you dropship medical supplies?
You can consider dropshipping items like feeding tubes or exam gloves to medical professionals. Besides, you can also sell home health supplies, such as medical beds, canes, or home diagnostic kits. As you can see, the medical supplies niche is so widespread. It has a consistent, growing demand in the market.
What is DME accreditation?
Durable Medical Equipment accreditation is available to DME suppliers that provide sleep-related DME to patients. This includes both free-standing suppliers and sleep facilities that provide DME equipment to their patients. Complete your DME application now or contact us for more information.
What is a Part B supplier?
Participating supplier means a supplier that has an agreement with CMS to participate in Part B of Medicare in effect on the date of the service. Payment on an assignment-related basis means payment for Part B services -
Who can be an authorized official?
An Authorized Official (AO) is a staff user for an employer organization who has been vetted and approved by either EUS or PECOS, and who has the legal authority to sign for and speak on behalf of that organization. AOs have access to all business functions for the employer organizations they represent.
How do I become a provider in Texas?
If you have questions, call your local area TMHP provider relations representative. To find your area representative, go to the Provider Enrollment Regional Support web page or call 800-568-2413.
What is Caqh and credentialing?
CAQH is an online data repository of credentialing data. Practitioners self report demographic, education and training, work history, malpractice history, and other relevant credentialing information for insurance companies to access.
What is initial credentialing?
Initial credentialing is one of the key components of a process that each health plan utilizes when a provider seeks to join a health plan network. Providers must successfully complete the credentialing process prior to an affiliation with a health plan.
What is the difference between Medicare Part A and Part B?
Part A is hospital coverage, while Part B is more for doctor's visits and other aspects of outpatient medical care. These plans aren't competitors, but instead are intended to complement each other to provide health coverage at a doctor's office and hospital.
How to become a supplier for Medicare?
The most important step to becoming a supplier is to obtain DME accreditation . To do that, you have to comply with the supplier standards set for the Medicare program, as well as with the defined quality standards. You also need to provide a $50,000 DMEPOS surety bond as a part of the enrollment after receiving your accreditation.
How long does it take to get Medicare accreditation?
The accreditation can take up to nine months from the time of your application. Once you have obtained it, you have to undergo the Medicare enrollment with the CMS. Institutional providers have to use CMS-855A Form, while DMEPOS suppliers have to complete CMS-855S Form.
How much surety bond do I need for CMS?
You have to provide a $50,000 surety bond to the CMS. This amount is necessary for each NPI you have and want to use. Thus, you may need a larger bond amount if you have numerous practice locations as an organizational supplier. In order to get bonded, you have to pay a bond premium, which is a fraction of the required amount.
What is DMEPOS in Medicare?
Medical practitioners and medical service providing organizations that want to be able to bill the Medicare system for supplying Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) need to undergo a rigorous process.
Do dentists have to be accredited to use DMEPOS?
While there are exemptions, it is applicable to medical practitioners who want to act as suppliers of: Since the beginning of 2019, dentists providing DMEPOS to patients are also required to undergo an accreditation process and meet relevant requirements.
Do I need a NPI number for DME?
While this is not a part of the accreditation itself, getting a National Provider Identifier (NPI) number is necessary for meeting the DME license requirements. Existing providers typically have the number already, as it is required by the CMS and commercial healthcare insurers.
How to contact Medicare?
Medicare has specific rules for marketing to people with Medicare. Suppliers can’t make uninvited contact with you by phone about supplying a Medicare-covered item unless one of these situations applies: 1 You've given written permission to the supplier to contact you about a Medicare-covered item that you need to rent or buy. 2 The supplier is contacting you to coordinate delivery of the item. 3 The supplier is contacting you about providing a Medicare-covered item other than a covered item you already have, and the supplier has provided at least one covered item to you during the previous 15-month period.
Do Medicare contract suppliers have to accept assignment?
They also have to be in good standing with Medicare, and be accredited by an independent accreditation organization. Medicare contract suppliers must: Accept Assignment for all contract items. This means they can’t charge you more than the Medicare-approved amount .
What documents are needed to get Medicare?
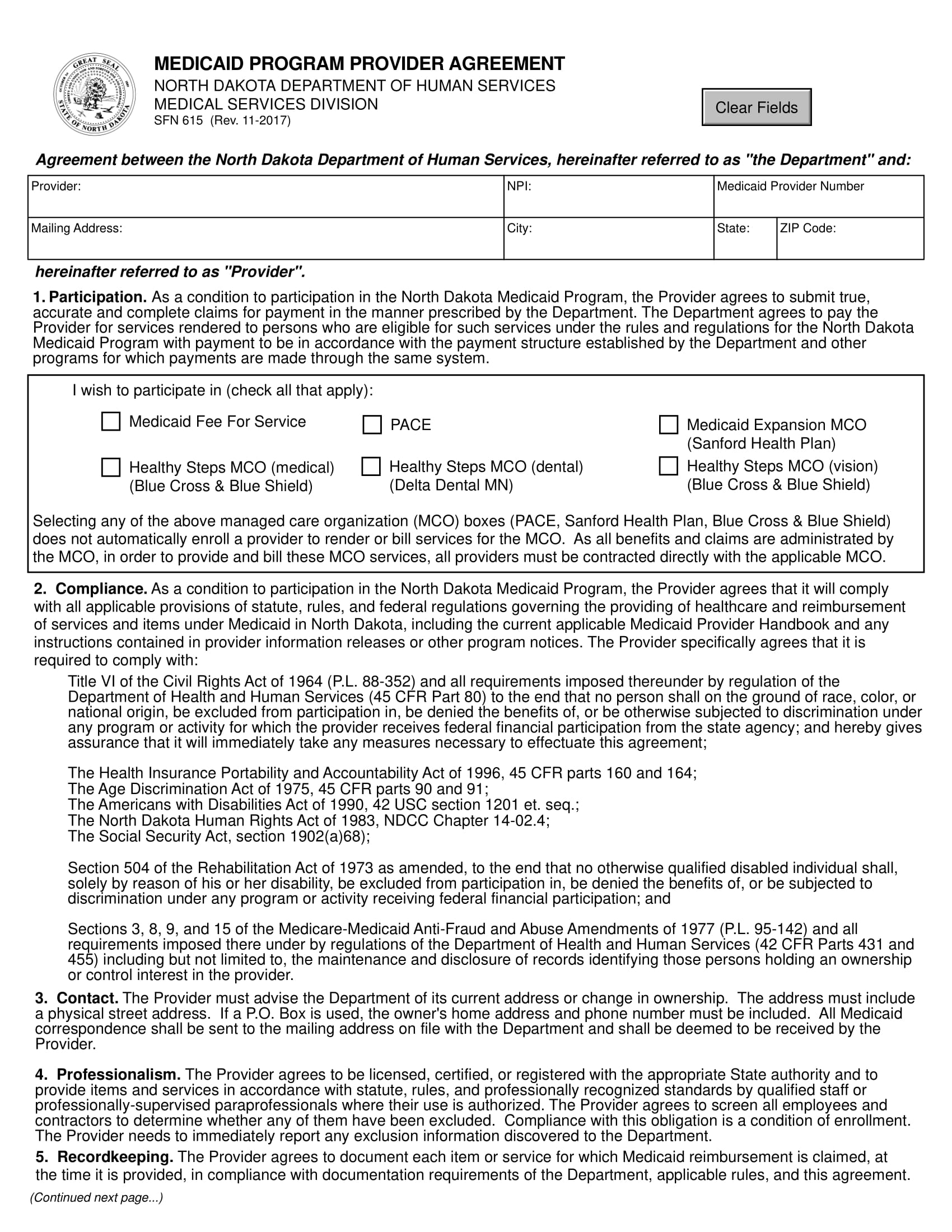
The documents needed are: Written confirmation from the Internal Revenue System (IRS) that has your legal business name and tax ID number. Banking information if you have an agreement with a bank to cover Medicare payments.
How long does it take to reassign Medicare benefits?
Don’t Forget the required documents – Make sure you have all the necessary documents to process your application. The process may take 90 days or longer, and if you need additional documents to submit, the processing time will reset. The documents needed are:
Do you need to fill out 855A?
You must fill out CMS 855A if you are an institutional provider like home health agencies, outpatient physical therapy services, and hospice. But if you sell supplies or medical equipment, fill out CMS 855S, this is also called the MEA for Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS).
How long does it take to change your Medicare billing information?
It’s important to keep your enrollment information up to date. To avoid having your Medicare billing privileges revoked, be sure to report any change within 30 days. Changes include, but are not limited to: a change in ownership. an adverse legal action. a change in practice location.
What is DMEPOS in Medicare?
Suppliers who receive Medicare reimbursement for durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS) are required to: If your business doesn’t dispense or furnish DMEPOS, you should use the Medicare Enrollment Guide for Providers & Suppliers.
What to do if your business doesn't dispense DMEPOS?
If your business doesn’t dispense or furnish DMEPOS, you should use the Medicare Enrollment Guide for Providers & Suppliers. If you’re enrolling a hospital, critical care facility, skilled nursing facility, home health agency, hospice, or other similar institution, you should refer to the Medicare Enrollment Guide for Institutional Providers.
What is Medicare application?
application is used to initiate a reassignment of a right to bill the Medicare program and receive Medicare payments (Note: only individual physicians and non-physician practitioners can reassign the right to bill the Medicare program).
What is NPI in Medicare?
The National Provider Identifier (NPI) will replace health care provider identifiers in use today in standard health care transactions. Suppliers must obtain their NPI prior to enrolling in the Medicare program. Enrolling in Medicare authorizes you to bill and be paid for services furnished to Medicare beneficiaries.
What is CMS in healthcare?
The Centers for Medicare & Medicaid Services (CMS) provides direction and technical guidance for the administration of the Federal effort to plan, develop, manage and evaluate health care financing programs and policies.
What is SBS in CMS?
CMS has a full time Small Business Specialist (SBS) co-located at CMS. The SBS is a member to the Health and Human Services (HHS) Office of Small and Disadvantaged Business Utilization (OSDBU) headquartered in the Hubert H. Humphrey Building in DC. The SBS is CMS' OSDBU representative ensuring that all reasonable action is taken to increase awards to small, small disadvantaged, HUBZones, and women-owned businesses. Company profiles and capability statements for all types of services are maintained by this office.