
If you are currently a participating provider and wish to become non-participating, you will need to submit a letter (on office letterhead) to your local carrier or administrative contractor stating your intent. This letter must include the original signature of the authorized representative or individual provider.
What is a non par Medicare provider?
There are two types of Medicare providers. Participating providers (PAR) accept payment directly from Medicare. At the office you pay your deductible and the doctor waits for payment from Medicare. Non-participating providers (NON-PAR) collect the entire fee at the time of your visit and the patient waits for reimbursement from Medicare. NON-PAR fees are set by Medicare not by the provider.
What doctors accept Medicare?
They provide home visiting doctor care services, home nurse visit, preventive care, and elder care at the comfort of your home. Octaplus Medicare is proud to announce its Doctor Vist at Home service in Mangalore, providing first-class medical assistance to patients from the comfort of their homes.
How to find doctors who accept your Medicare Advantage plan?
- Your plan may pay less toward your care. ...
- The fees for health services may be higher. ...
- Any amount you pay might not contribute to your plan deductible, if you have one.
- You may need preauthorization for any services you receive in order for any coverage to apply.
How do you find a Medicare provider?
- Providers can enter data via the Interactive Voice Response (IVR) telephone systems operated by the MACs.
- Providers can submit claim status inquiries via the Medicare Administrative Contractors’ provider Internet-based portals.
- Some providers can enter claim status queries via direct data entry screens.
Does Medicare pay non-participating providers?
Non-participating providers haven't signed an agreement to accept assignment for all Medicare-covered services, but they can still choose to accept assignment for individual services. These providers are called "non-participating."
What does non-participating provider mean Medicare?
Non-participating providers accept Medicare but do not agree to take assignment in all cases (they may on a case-by-case basis). This means that while non-participating providers have signed up to accept Medicare insurance, they do not accept Medicare's approved amount for health care services as full payment.
What is a non-participating provider?
A health care provider who doesn't have a contract with your health insurer. Also called a non-preferred provider. If you see a non-participating provider, you'll pay more. Top Top.
What advantages might a participating provider in the Medicare program have over a non par provider?
The advantages of being a participating provider: Higher allowances (5% higher than non-participating providers). Direct payment (Medicare sends payment directly to the provider, not the patient). Medigap transfer (Medicare forwards claims on to Medigap insurers for providers).
What are the advantages of a non-participating provider?
Non-Par Providers can also take payment in full at the time of service directly from the beneficiary, so they are not waiting for a 3rd Party Payor to reimburse them. Furthermore, the billing can be up to 115% of the Medicare Fee Schedule, so you can get a little more money for your time as a Non-Par Provider.
When a provider is non-participating they will expect?
When a provider is non-participating, they will expect: 1) To be listed in the provider directory. 2) Non-payment of services rendered. 3) Full reimbursement for charges submitted.
What is the difference between out of network and non-participating?
If you see a doctor or use a hospital that does not participate with your health plan, you are going out-of-network. You usually have to pay more for out-of-network care. Some plans won't cover any amount of out-of-network care, while others cover a percentage of care.
Can a Medicare patient be self pay?
True Blue. The Social Security Act states that participating providers must bill Medicare for covered services. The only time a participating-provider can accept "self-payments" is for a non-covered service. For Non-participating providers, the patient can pay and be charged up to 115% of the Medicare Fee Schedule.
Does Medicare reimburse for out of network?
Coverage for out-of-network doctors depends on your Medicare Advantage plan. Many HMO plans do not cover non-emergency out-of-network care, while PPO plans might. If you obtain out of network care, you may have to pay for it up-front and then submit a claim to your insurance company.
What is the difference between a participating and non-participating provider?
Participating Provider versus Non-Participating Provider - Medigap information is transferred. - A non-participating provider has not entered into an agreement to accept assignment on all Medicare claims.
What percentage of doctors do not accept Medicare assignment?
In all states except for 3 [Alaska, Colorado, Wyoming], less than 2% of physicians in each state have opted-out of the Medicare program.
What is the incentive to Medicare participating providers?
Medicare provides a number of incentives for physicians to participate: The Medicare payment amount for PAR physicians is 5% higher than the rate for non-PAR physicians. Directories of PAR physicians are provided to senior citizen groups and individuals who request them.
How much can a non-participating provider bill Medicare?
Medicare will then send any reimbursement directly to the patient. As a Non-Participating Medicare Provider, you can bill the patient up to 115% of the Medicare Fee Schedule.
What is the relationship status of a physical therapist with Medicare?
There are three possibilities for a Physical Therapist’s relationship-status with Medicare: 1) No relationship at all (notthe same as a “Non-Participating Provider” and also notthe same as “opting out”) 2) Participating Provider. 3) Non-Participating Provider.
What is the maximum amount of Medicare Physician Fee Schedule?
If you are a Non-Participating provider, providing covered services and collecting payment from beneficiaries at the time of service, the maximum amount you may charge is 115% of the approved fee schedule amount for Non-Participating providers; which is 95% of the normal Medicare Physician Fee Schedule (MPFS).
What is the most common Medicare Advantage plan?
There are coordinated care options such as HMOs or PPOs, private fee-for-service (PFFS) plans, and medical savings account (MSA) plans. The most common form of Medicare Advantage plan is the HMO. Apparently, there are a number of Medicare Advantage plans in which coverage is limited to only in-network providers.
Can a Medicare beneficiary see you out of network?
If a beneficiary with a Medicare Advantage plan wants to see you on a cash-pay basis, and you are out-of-network with that plan , you need to call the plan and ask them if it is okay for you to provide them with covered services and that the beneficiary pay you directly out-of-pocket.
Can non-par providers take payment in full?
This is hugely important for some practices in certain areas with certain demographics. Non-Par Providers can also take payment in full at the time of service directly from the beneficiary, so they are not waiting for a 3rd Party Payor to reimburse them.
Can you be a non-par provider for Medicare?
If you feel that you need to be able to treat Medicare beneficiaries, either financially or personally, but don’t want to wait for Medicare reimbursement (or denials), then being a Non-Par Provider might be a an option to consider regardless of the extra 15% you can bill.
How to become a Medicare provider?
Become a Medicare Provider or Supplier 1 You’re a DMEPOS supplier. DMEPOS suppliers should follow the instructions on the Enroll as a DMEPOS Supplier page. 2 You’re an institutional provider. If you’re enrolling a hospital, critical care facility, skilled nursing facility, home health agency, hospice, or other similar institution, you should use the Medicare Enrollment Guide for Institutional Providers.
How to get an NPI?
If you already have an NPI, skip this step and proceed to Step 2. NPIs are issued through the National Plan & Provider Enumeration System (NPPES). You can apply for an NPI on the NPPES website.
How long does it take to change your Medicare billing?
To avoid having your Medicare billing privileges revoked, be sure to report the following changes within 30 days: a change in ownership. an adverse legal action. a change in practice location. You must report all other changes within 90 days. If you applied online, you can keep your information up to date in PECOS.
Do you need to be accredited to participate in CMS surveys?
ii If your institution has obtained accreditation from a CMS-approved accreditation organization, you will not need to participate in State Survey Agency surveys. You must inform the State Survey Agency that your institution is accredited. Accreditation is voluntary; CMS doesn’t require it for Medicare enrollment.
Can you bill Medicare for your services?
You’re a health care provider who wants to bill Medicare for your services and also have the ability to order and certify. You don’t want to bill Medicare for your services, but you do want enroll in Medicare solely to order and certify.
What is a non-participating provider?
A nonparticipating provider is a provider involved in the Medicare program who has enrolled to be a Medicare provider but chooses to receive payment in a different method and amount than Medicare providers classified as participating. The nonparticipating provider may receive reimbursement for rendered services directly from their Medicare patients.
What is the maximum amount of Medicare fee for a non-participating physician?
The maximum amount that a nonparticipating physician, other practitioner or supplier is permitted to charge for a Medicare beneficiary for unassigned services paid under the physician fee schedule is 115% of the Medicare allowed charge.
What happens when a physician bills a primary insurer but receives no payment?
When a physician bills a primary insurer above his limiting charge, but receives no payment because the insurer applies the amount to the patient's deductible, the physician must adjust his bill to the limiting charge or lower and may then bill Medicare.
When does limiting charge apply to Medicare?
The limiting charge applies when Medicare is the secondary payer, unless the claim to the primary payer is assigned, or the primary payer requires the physician to accept its payment as payment in full.
What is elective surgery for Medicare?
Elective surgery for Medicare purposes is defined as surgery that can be scheduled in advance, is not an emergency and would not result in death or permanent impairment of health if delayed.
Is limiting charge still monitored by Medicare?
The limiting charges submitted by nonparticipating providers are still monitored by Medicare staff. In the absence of the limiting charge exception reports, providers, other practitioners and suppliers can use their remittance notices to calculate the limiting charge amounts.
Can a physician bill Medicare if the primary insurer is less than the limiting charge?
When a physician bills a primary insurer above his or her limiting charge and receives payment from the primary insurer that is less than the Medicare limiting charge, he/she is not obligated to accept the primary's payment as full payment and therefore, can submit a bill to Medicare.
What is a Medicare participating provider?
Medicare participating providers must adhere to the following: A participating provider is one who voluntarily and in advance enters into an agreement in writing to provide all covered services for all Medicare Part B beneficiaries on an assigned basis. Agrees to accept Medicare approved amount as payment in full.
How much is the Medicare limit for non-participating providers?
As a non-participating provider and not willing to accept assignment, the patient is responsible to pay you the Limiting Charge of $34.00. You cannot accept your regular fee of $35.00 even though you are non-participating. You bill Medicare the Limiting Charge of $34.00.
How much does Medicare reimburse you?
Medicare will reimburse you $24.00, which is 80% of the Non-Par Fee Allowance (assuming the deductible has been met). Just a side note, at the present time DCs cannot “opt-out” of the Medicare program – so if you choose to treat Medicare patients, then you must follow the above rules.
Can a non-participating provider accept assignment?
Medicare non-participating providers must adhere to the following: A non-participating provider has not entered into an agreement to accept assignment on all Medicare claims. Can elect to accept assignment or not accept assignment on a claim-by-claim basis. Cannot bill the patient more than the limiting charge on non-assigned claims.
Can Medicare collect more than deductible?
May not collect more than applicable deductible and coinsurance for covered services from patient. Payment for non-covered services may also be collected. Charges are not subject to the limiting charge. Medicare payment paid directly to the provider. Mandatory claims submission applies. Reimbursement is 5 percent higher than ...
PAR and non-PAR Providers with Medicare
The Center for Medicare & Medicaid Services (CMS) is a federal agency within the Department of Health and Human Services which manages and oversees the Medicare program for beneficiaries. Physicians are required to comply with numerous laws and regulations related to various aspects of their practice within the Medicare program.
Participating (PAR) Providers with Medicare
Participating in the Medicare program means the health care professional agrees to accept assignments for all services provided to Medicare beneficiaries. By accepting an assignment, it states that the provider agrees to accept the amount approved by Medicare as the total payment for covered services.
Why you should be PAR with Medicare?
Your Medicare fee schedule amount is 5% higher than that of a non-participating provider.
Non-Participating (non-PAR) Provider with Medicare
If a provider makes the decision to not be a participating provider in the Medicare program, they will have to choose either to accept or not accept assignments on Medicare claims on a claim-by-claim basis.
PAR Vs Non-PAR Providers
Participating providers must accept assignments; while non-participating providers may collect up-front from the patient. Essentially, if you are a participating provider, your patient will only pay any deductible and/or co-insurance at the time of service and then Medicare reimburses the allowed fee after the claim is billed.
Changing the Status
If you are currently a non-participating provider and wish to become participating, you will have to contact your carrier for a participation agreement.
What is Medicare Participating Provider versus Non-Participating Provider?
Medicare Participating Provider versus Non-Participating Provider. beneficiaries on an assigned basis . not entered into an agreement to accept assignment on all Medicare claims. to accept Medicare-approved amount as payment in full. or not accept assignment on a claim-by-claim basis.
What does "non-participating provider" mean?
A non-participating provider has. not entered into an agreement to accept assignment on all Medicare claims. Agrees. to accept Medicare-approved amount as payment in full. Can elect to accept assignment. or not accept assignment on a claim-by-claim basis. May not.
When is open enrollment for Medicare?
Toward the end of each calendar year there is an open enrollment period. The open enrollment period generally is from mid-November through December 31. During this period, if you are enrolled in the Medicare Program, you can change your current participation status beginning the next calendar year on January 1.

Restrictions
- If a physician chooses not to participate in the Medicare program, there are special rules that must be followed. The following restrictions apply to non-participating providers: 1. A Special Charge Limit is Applied - A non-participating physician is limited on the amount he or she can charge Medicare patients for his/her services. The actual charge cannot exceed the limiting char…
Limiting Charges
- The limiting charge is the maximum dollar amount that the Federal Government allows a non-participating physician to charge Medicare patients for a given service. Effective for services rendered on or after January 1, 1991, the limiting charge applies only to services billed on a non-assigned basis. Under current legislation, all services listed with relative value units (RVUs) on th…
Notice of Elective Surgery
- The Omnibus Budget Reconciliation Act of 1986 (OBRA) requires that when a nonparticipating surgeon does not accept assignment for elective surgery performed on a Medicare beneficiary, he/she must provide certain information, in writing, to the beneficiary before the surgery. This requirement only applies to elective surgery for which charges are $5...
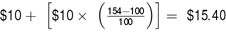
Sample Elective Surgery Notice
- Dear Patient: I do not plan to accept assignment on your surgery. The law requires that where assignment is not taken and the charge is $50000 or more, an estimate of the charge and your liability must be provided prior to surgery. These estimates assume that you have met the $10000 annual Medicare Part B deductible: Type of surgery: Estimated charge (item 1): Medicare estima…