When do I need to Bill HCPCS q2039?
Note: Claims billed for dates of service prior to 12/31/2017, if submitted on or after 01/01/2018, must bill HCPCS Q2039 for the claim to process correctly. Note: CPT® code 90694 is effective for claims processed with dates of service on or after 7/1/2020.
When does the CPT code change for 2020?
This revision is due to the 2020 Annual CPT/HCPCS Code Update and is effective on January 1, 2020. Under Associated Contract Numbers added contract numbers 10111, 10211, 10311, 11201, 11301, 11401 and 11501. Under Article Text removed the verbiage “Part B” from the first sentence and fourth bullet point.
When do you bill Medicare as the secondary payer?
When you find another insurer as the primary payer, bill that insurer first. (Page 16 of Chapter 3 of the Medicare Secondary Payer Manual provides guidance on finding other primary payers.) After receiving the primary payer remittance advice, bill Medicare as the secondary payer, if appropriate.
Why don't I get a bill from Medicare?
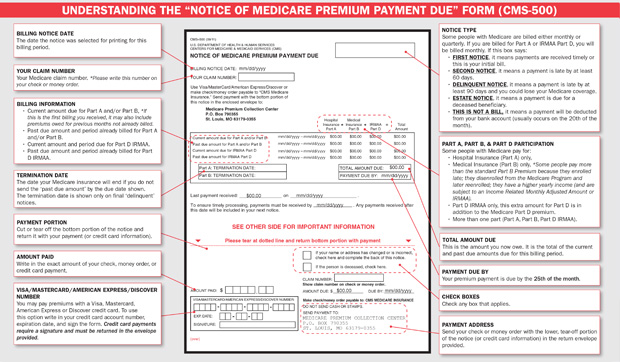
Most people don't get a bill from Medicare because they get these premiums deducted automatically from their Social Security (or Railroad Retirement Board) benefit.) Your bill pays for next month's coverage (and future months if you get the bill every 3 months).

How do you bill for re excision?
To report a re-excision procedure performed to widen margins at a subsequent operative session, see codes 11600-11646, as appropriate. Append a modifier 58 if the re-excision procedure is performed during the postoperative period of the primary excision procedure."
How do you bill for follow up visits?
Follow-up visits, like initial visits, should be coded using the appropriate evaluation and management (E/M) code (i.e., 99211–99215). Given the limited interaction with the patient and limited work involved, the level of service is likely to be low (e.g., 99211 or 99212).
How do you bill for fluoroscopy?
8. Fluoroscopy reported as CPT code 76000 is integral to many procedures including, but not limited, to most spinal, endoscopic, and injection procedures and shall not be reported separately. For some of these procedures, there are separate fluoroscopic guidance codes which may be reported separately.
How do you bill for circumcision?
There are two main circumcision medical billing codes. Although one code is used more often, there are two that are acceptable. The two medical billing codes used for newborns circumcision are 54150 and 54160. 54150 means, circumcision, using clamp or other device; newborn.
How do you code post op visits?
Post-operative visits should be reported with CPT code 99024 when the visit is furnished on the same day as an unrelated E/M service (billed with modifier 24).
Can you bill two office visits same day?
If a provider sees the patient twice on the same day for related problems and the payer doesn't allow you to report those services separately, then you should combine the work performed for the two visits and select a single E/ M service code that best describes the combined service.
Does Medicare cover fluoroscopy?
Answer: Yes, in 2017, fluoroscopy codes, codes +70002 and +77003 (see code descriptions below) have been revised and are now add-on codes. Under each code in the CPT manual, the primary codes these imaging codes may be used with are listed.
Does CPT 76000 need a modifier?
Modifier 59 or X modifiers can be used for CPT 76000 in order to indicate that it is a distinct or independent service.
When can you bill CPT 76000?
fluroscopyIn such scenario, when the fluroscopy is the only exam performed by the physician we can bill the CPT code 76000 as separate and independent procedure.
What is the CPT code for circumcision?
CPT® Code 54161 in section: Circumcision, surgical excision other than clamp, device, or dorsal slit.
What is the ICD 10 code for circumcision?
Z41.2ICD-10 Code for Encounter for routine and ritual male circumcision- Z41. 2- Codify by AAPC.
What is the ICD 10 PCS code for a routine circumcision?
Z41. 2 - Encounter for routine and ritual male circumcision | ICD-10-CM.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Language quoted from Centers for Medicare and Medicaid Services (CMS), National Coverage Determinations (NCDs) and coverage provisions in interpretive manuals is italicized throughout the policy.
Article Guidance
This article contains coding and other guidelines that complement the Local Coverage Determination (LCD) for EEG - Ambulatory Monitoring.
ICD-10-CM Codes that Support Medical Necessity
The correct use of an ICD-10-CM code listed below does not assure coverage of a service. The service must be reasonable and necessary in the specific case and must meet the criteria specified in the determination.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Title XVIII of the Social Security Act (SSA) §1833 (e) prohibits Medicare payment for any claim lacking the necessary documentation to process the claim
Article Guidance
Medicare provides preventive coverage only for certain vaccines. These include:
ICD-10-CM Codes that Support Medical Necessity
Covered ICD-10 codes for Influenza, Pneumococcal, Pneumococcal and Seasonal Influenza Virus Vaccines received during the same visit and Hepatitis B
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
This article contains coding and other guidelines that complement the local coverage determination (LCD) for Cardiac Catheterization and Coronary Angiography.
ICD-10-CM Codes that Support Medical Necessity
The use of an ICD-10-CM code listed below does not assure coverage of a service. The service must be reasonable and necessary in the specific case and must meet the criteria specified in the attached determination.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
