Common Types of Durable Medical Equipment Generally, equipment meets the definition of DME for Medicare when it is reusable, designed for clinical use in the home and expected to withstand use for at least 3 years. These items must be determined as medically necessary and require a health care professional’s referral or prescription.
Full Answer
Does Medicaid cover DME?
“Medicare does not currently pay for over-the-counter ... As of Jan. 15, people with private health insurance have been eligible for coverage of up to eight at-home tests per month, per person ...
What DME does Medicare pay for?
What durable medical equipment does Medicare cover? Medicare covers a range of items, supplies and equipment such as durable medical equipment. The list of DME that is covered by Medicare includes (but is not limited to): Air-fluidized beds and various other support surfaces Blood pressure monitors Blood sugar monitors Blood sugar test strips Canes
What DME does Medicare cover?
Medicare may help pay for your manual wheelchair if all of the following conditions are met:
- Your health makes it hard to move around in your home. ...
- You can safely use the wheelchair yourself, or you always have someone with you to help you use it.
- Your doctor signs a written order for the equipment. ...
- You get equipment from a Medicare-approved supplier.
Does Medicare pay for DME?
Medicare pays for different kinds of DME in different ways. Depending on the type of equipment: You may need to rent the equipment. You may need to buy the equipment. You may be able to choose whether to rent or buy the equipment. Medicare will only cover your DME if your doctors and DME suppliers are enrolled in Medicare.

What is considered to be DME?
Equipment and supplies ordered by a health care provider for everyday or extended use. Coverage for DME may include: oxygen equipment, wheelchairs, crutches or blood testing strips for diabetics.
How does Medicare price DME?
Medicare payment for durable medical equipment (DME), prosthetics and orthotics (P&O), parenteral and enteral nutrition (PEN), surgical dressings, and therapeutic shoes and inserts is equal to 80 percent of the lower of either the actual charge for the item or the fee schedule amount calculated for the item, less any ...
What is a Medicare DME claim?
covers. medically necessary. Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine. DME if your doctor prescribes it for use in your home.
What are the DME codes?
DME procedure codes with most claims in 2020E0601. Continuous positive airway pressure (CPAP) Device. ... E0114. Crutches underarm, other than wood, adjustable or fixed pair, with pads, tips and handgrips. ... E0562. Humidifier, heated, used with positive airway pressure (PAP) device. ... E0700. ... E1390. ... E1399. ... E0570. ... E0776.More items...
What is the CMS fee schedule?
A fee schedule is a complete listing of fees used by Medicare to pay doctors or other providers/suppliers. This comprehensive listing of fee maximums is used to reimburse a physician and/or other providers on a fee-for-service basis.
What does NR mean on Medicare DME fee?
California Non-RuralIn the 2016 changes to the Official Medical Fee Schedule (OMFS), the California DWC introduces two new columns to the DME file: CA (NR) and CA (R). CA(NR) stands for California Non-Rural. CA(R) stands for California Rural.
Are L codes considered DME?
L-Codes: Splinting and Bracing Before you can bill L-codes to Medicare, you must be a certified DME provider. If you haven't received your DME certification yet, here are some tips for billing Medicare for orthotic services: Bill 97760 for the initial assessment; Bill the patient for the device or supplies; and.
What is the ICD 10 code for durable medical equipment?
Claims for DME for a disabled parent must be submitted using HCPCS code A9999 (miscellaneous DME supply or accessory, not otherwise specified), ICD-10-CM diagnosis code Z73. 6 and modifier SC.
Which of the following is excluded from Medicare coverage?
Non-medical services, including a private hospital room, hospital television and telephone, canceled or missed appointments, and copies of x-rays. Most non-emergency transportation, including ambulette services. Certain preventive services, including routine foot care.
How do I submit a DME claim to Medicare?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
What is modifier RR?
Categories for using common modifiers Use modifiers RR, NU and UE for the following categories: Capped rental item. Oxygen equipment without contents. Items that require frequent and substantial servicing. Routinely purchased items or inexpensive ones.
What is a category code?
Category codes are user defined codes to which you can assign a title and a value. The title appears on the appropriate screen next to the field in which you type the code.
What is assignment in Medicare?
Assignment —An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance.
Does Medicare pay for DME repairs?
Medicare will pay 80% of the Medicare-approved amount (up to the cost of replacing the item) for repairs. You pay the other 20%. Your costs may be higher if the supplier doesn’t accept assignment.
What is DME in Medicare?
Medicare payment for durable medical equipment (DME), prosthetics and orthotics (P&O), parenteral and enteral nutrition (PEN), surgical dressings, and therapeutic shoes and inserts is equal to 80 percent of the lower of either the actual charge for the item or the fee schedule amount calculated for the item, less any unmet deductible.
What is the MLR for DME?
This rule also proposes the implementation of budget-neutral fee schedules for splints and casts, and intraocular lenses (IOLs) inserted in a physician’s office. Finally, this rule would make a few technical amendments and corrections to existing regulations related to payment for DMEPOS items and services in the End-Stage Renal Disease Prospective Payment System Proposed Rulemaking. View CMS-1526-P .
When will CMS increase fee schedule?
On May 11, 2108, CMS published an interim final rule with comment period (IFC) that increases the fee schedule rates for items furnished from June 1, 2018, through December 31, 2018, for certain durable medical equipment (DME) and enteral nutrition furnished in rural and non-contiguous areas of the country not subject to the Durable Medical Equipment, Prosthetics, Orthotics and Supplies (DMEPOS) Competitive Bidding Program (CBP). To safeguard beneficiary access to necessary items and services, this rule increases the fee schedule amounts for certain DME and enteral nutrition in rural and noncontiguous areas to a blend of 50 percent of the fee schedule amounts that would have been paid from June 1, 2018, through December 31, 2018, had no adjustments been made and 50 percent of the adjusted fee schedule amounts. For areas other than rural or non-contiguous areas, the fee schedules for certain DME and enteral nutrition codes will continue to be based on 100 percent of the adjusted fee schedule amounts from June 1, 2018 through December 31, 2018.
When was the Medicare non-mail order for diabetic testing supplies passed?
Diabetic Testing Supplies Provisions of the American Taxpayer Relief Act of 2012. On Wednesday, January 2, 2013, the President signed into law the American Taxpayer Relief Act of 2012 . Section 636 of this new law revises the Medicare non-mail order fee schedule amounts for diabetic testing supplies.
When will the oxygen and oxygen equipment fee be changed?
The Consolidated Appropriations Act of 2021 (Public Law 116-260) was signed into law on December 27, 2020. Effective April 1, 2021, section 121 of this Act eliminates the budget neutrality requirement set ...
When did the DME and P&O fee schedules start?
OBRA of 1990 added a separate subsection, 1834 (h), for P&O. The DME and P&O fee schedules were implemented on January 1, 1989 with the exception of the oxygen fee schedules, which were implemented on June 1, 1989. Section 13544 of OBRA of 1993, which added section 1834 (i) to the Social Security Act, mandates a fee schedule for surgical dressings;
Is a continuous glucose monitor durable?
CMS issued a ruling on January 12, 2017 concluding that certain continuous glucose monitors (CGMs), referred to as therapeutic CGMs, that are approved by the Food and Drug Administration for use in making diabetes treatment decisions are considered durable medical equipment.
How long does a DME last?
Generally, equipment meets the definition of DME for Medicare when it is reusable, designed for clinical use in the home and expected to withstand use for at least 3 years. These items must be determined as medically necessary and require a health care professional’s referral or prescription.
Why do we need medical equipment?
Certain medical conditions require the use of medical equipment to help address mobility issues, administer medication, or provide relief from symptoms of an illness or injury.
Can social workers order DME?
Although they may not be qualified to order equipment directly, social workers and certain agency representatives may also help patients secure the appropriate order for DME if their primary care physician is unavailable.
Does Medicare cover DME?
Medicare Coverage for Durable Medical Equipment. When you’re navigating the costs associated with DME, your Medicare Part B terms apply. This means that in order for Medicare Part B to help mitigate the costs of your DME, you must be up-to-date on your monthly premium.
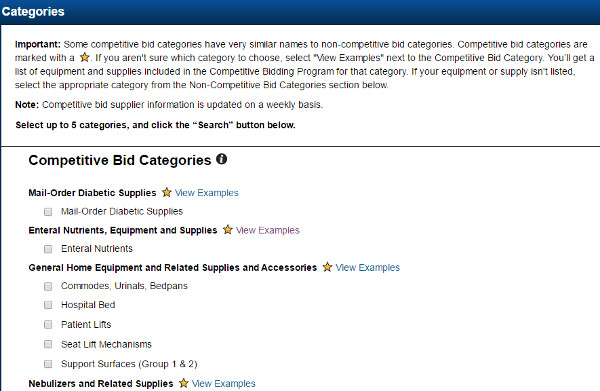
What is a DMEPOS file?
The DMEPOS public use file contains fee schedules for certain items that were adjusted based on information from the DMEPOS Competitive Bidding Program in accordance with Section 1834 (a) (1) (F) of the Act.
What is gap filling in Medicare?
For newly covered items of DMEPOS paid on a fee schedule basis where a Medicare fee does not exist , the Centers for Medicare & Medicaid Services (CMS) uses a process to establish fees called gap-filling. This allows Medicare to establish a price that aligns with the statutory requirements for the DMEPOS fee schedule.
What is Medicare Accessibility Act?
CMS is implementing the Patient Access and Medicare Protection Act to ensure that beneficiaries have access to wheelchair accessories and seat and back cushions when furnished with Group 3 complex rehabilitative power wheelchairs. To ensure beneficiary access to these accessories particularly for these vulnerable populations, advance payment may be available for suppliers. Prior to July 1, suppliers will be paid the adjusted fee schedule rates. The average reduction during this period for these items is approximately 10%. During this time, CMS has announced that suppliers are able to submit a single advance payment request for multiple claims if the conditions described in CMS regulations at 42 CFR Section 421.214 are met. Additional information is below.
What is TTFT in Medicare?
TTFT is a system consisting of an electromagnetic field generator and transducer arrays and will be covered under the Medicare Part B benefit for durable medical equipment (DME) for items and services furnished on or after September 1, 2019.
When will Medicare change the KU modifier?
As aforementioned, these system changes will be implemented on July 1, 2020.
What is a CGM?
CGMs are items of durable medical equipment (DME) that provide critical information on blood glucose levels to help patients with diabetes manage their disease . In January 2017, CMS issued a ruling providing for Medicare coverage of therapeutic CGMs.
When will CMS reprocess claims?
Claims for these accessories submitted prior to July 1, 2020, with dates of service from January 1, 2020 through June 30, 2020, will need to be reprocessed to ensure that CMS pays the unadjusted fee schedule amounts, as required by section 106 of the Further Consolidated Appropriations Act, 2020.
Medicare Allowed Amount Definition
Maximum amount on which payment is based for covered health care services. This may be called “eligible expense,” “payment allowance” or “negotiated rate.” If your provider charges more than the medicare allowed amount, patient no need to pay that amount when they are participating with Medicare insurance.
Medicare Maximum Allowable Reimbursements
Unless otherwise indicated, for these Rules, the Medicare procedures and guidelines are effective upon adoption and implementation by the CMS. The particular procedure or guideline to be used is that which is in effect on the date the service is rendered.
What is the DME rule?
The rule aims to prevent potential problems with access to medically necessary DME in rural and non-contiguous areas of the country. The rule also makes conforming changes to the regulations related to sections 5004 (b) and 16007 (a) of the 21 st Century Cures Act (Cures Act).
How much is the 50/50 fee schedule for Medicare?
It is estimated that these 50/50 blended fee schedule adjustments would cost over $290 million in Medicare benefit payments and $70 million in Medicare beneficiary cost sharing. For dual eligible beneficiaries, Medicaid pays the cost sharing. The impact for Medicaid is split between a Federal portion and the States’ portion, which for this rule is $10 million and $10 million, respectively.