
If you look up 47 minutes on the chart, you can bill for a maximum of 3 units (38 to 52 minutes). Each of the codes were performed for more than 15 minutes so each should be billed for 1 unit. You should then assign the extra unit to 97712 since it was treated for the longer amount of time. So you bill for 1 unit of 97110 and 2 units of 97112
Full Answer
Can a physical therapist bill Medicare for evaluation?
Medicare allows physical therapists to bill for initial evaluations in order to establish the plans of care, and, in some cases, physical therapists can bill for reevaluations if there has been a significant change in the client’s progress. Can you bill for co-treatments?
What is the Medicare-approved amount for physical therapy?
The Medicare-approved amount is the amount you as the physical therapist agree to be paid for services rendered, and the client is responsible for the remaining 20%. You should avoid waiving copays or deductibles, although you can offer financial assistance if necessary.
What is the CPT code for physical therapy evaluation?
Three new codes—97161, 97162, and 97163—replace the single 97001 CPT code for physical therapy evaluation
Does your physical therapy practice need to Bill and collect payment?
But if you’re serious about helping people, your practice needs to be able to cover its costs (and yours), and that means billing and collecting payment for your services. Billing is an inevitable part of owning a physical therapy practice, but it doesn’t need to be complicated or overwhelming.

Does Medicare pay for physical therapy evaluation?
Do I need a referral for physical therapy under Medicare? Medicare only pays for physical therapy if a doctor refers you. It will not cover physical therapy if you are not under a doctor's care.
What is the CPT code for PT evaluation?
Physical Therapy CPT Codes 97161: Physical therapy evaluation, low complexity.
When should I charge a re eval for physical therapy?
Under Medicare guidelines, a re-evaluation is medically necessary (and therefore payable) only if the therapist determines that the patient has had a significant improvement, or decline, or other change in his or her condition or functional status that was not anticipated in the POC (emphasis added).
What is the CPT code for re-evaluation of physical therapy established plan of care?
For PT, the new re-evaluation code is 97164 (Reevaluation of physical therapy established plan of care) and will require these components: An examination including a review of history and use of standardized tests and measures; and.
What is the difference between 97161 97162 and 97163?
The new PT codes are: 97161- Low Complexity Evaluation; 97162- Moderate Complexity Evaluation; 97163- High Complexity Evaluation; 97164- PT re-evaluation. Each evaluation level has certain components and are different between PT and OT. PT has four components to each evaluation code and OT has three.
How many units is a PT eval?
How many units is a PT eval?8 – 22 minutes1 unit38 – 52 minutes3 units53 – 67 minutes4 units68 – 82 minutes5 units83 minutes6 unitsJun 7, 2022
In which situation is a billable re-evaluation appropriate?
When medical necessity is supported, a re-evaluation is appropriate and is separately billable for: A patient who is currently receiving therapy services and develops a newly diagnosed related condition e.g., a patient that is currently receiving therapy treatment for TKA.
What is difference between progress note and re-evaluation?
Re-evaluations are not routine and shouldn't be billed routinely. Progress notes are routine and are completed at every 10th visit or every 30 days (whichever comes first).
What is re-evaluation in physical therapy?
A re-evaluation is focused on evaluation of progress toward current goals and making a professional judgment about continued care, modifying goals and/or treatment or terminating services.
Can 97164 and 97110 be billed together?
That's because CMS—at the behest of the APTA—has agreed to accept these pairs without the use of a modifier. In other words, you can perform the following services—and receive payment for them—without needing to affix modifier 59: 97110 with 97164. 97112 with 97164.
Can 97530 and 97112 be billed together?
No greater than 1-2 services/units of this code should be used on each visit date. If this code is used in conjunction with CPT 97110 or CPT 97530 on any given visit date, only 1-2 services/units of CPT 97112 are generally covered. Documentation must support the number of services/units for each visit date.
What is PT Eval Mod complex 30 min?
Moderate Complexity – Typically, 30 minutes are spent face-to-face with the patient and/or family. High Complexity – Typically, 45 minutes are spent face-toface with the patient and/or family.
How long does a physical therapist have to be on Medicare?
The rule stipulates that you need to provide direct treatment for a minimum of 8 minutes to be reimbursed by Medicare for a time-based code.
What happens if you are not credentialed by Medicare?
If you are not credentialed, you will not be allowed to treat or collect payment from Medicare patients, even if Medicare offers cover for those services.
What is an ABN for Medicare?
An Advance Beneficiary Notice of Noncoverage (ABN) is a signed declaration that the client will accept financial responsibility if Medicare (and it’s likely they will) denies the claim.
When did the therapy cap start?
Introduced in 1997 , the Therapy Cap caps physical therapy and speech therapy services at a yearly amount, which does not reset for each diagnosis. You need to monitor your clients’ cap and apply for an exemption if the client needs medical necessary care despite exceeding their cap.
Is physical therapy a profitable business?
Physical therapy practice owners in America have a lot going on from scheduling and treating clients, to running a profitable small business covering marketing, accounting, and much more. If you have to add keeping track of PT Medicare billing nuances to the list, it’s more than most therapists can handle.
What is 97164 in a re-evaluation?
Use: Re-evaluation (97164) This could include any improvement, decline, or other change in functional status that: you didn’t anticipate when you originally established the plan of care, and. requires further evaluation to ensure the best therapy outcomes.
What is 97164 in medical?
Use: Re-evaluation (97164) If you are treating a patient, and he or she presents with a second diagnosis that is either related to the original diagnosis or is a complication resulting from the original diagnosis, you’ll need to complete a re-evaluation and create an updated plan of care.
How long do you have to wait to start a Medicare case?
Unfortunately, there isn’t a whole lot of solid guidance on this scenario. However, in the case of Medicare, if 60 days have passed, you must start the case over with an initial evaluation. That’s because Medicare automatically discharges a case when no claims have been submitted for 60 days. But again, this rule specifically applies to Medicare. For those patients with commercial insurances, you should defer to the payer—as well as your state practice act if it includes guidance on when evaluations and re-evaluations are appropriate.
What is 97164 in healthcare?
Use: Re-evalua tion (97164) If, during the course of care, you determine that the original plan isn’t having the intended effect on the patient, you may feel it necessary to change the plan of care. In this case, you would perform—and bill for—a re-evaluation.
Can you re-evaluate after surgery?
Re-evaluations also may be appropriate for patients who received therapy treatment prior to surgery and then returned for additional rehabilitation after surgery. The catch in this situation is that some commercial payers may consider the post-op treatment period a new episode of care, in which case you’d need to use an evaluation code.
Should you defer to the payer for a rotator cuff evaluation?
For those patients with commercial insurances, you should defer to the payer—as well as your state practice act if it includes guidance on when evaluations and re-evaluations are appropriate . Example: You treat a 30-year-old carpenter for right rotator cuff weakness and discharge him or her from care.
Why do you need to bill for physical therapy?
But in order to stay in business long enough to actually make a difference in your patients’ lives, you absolutely must bill—and collect payment— for your services.
What is CPT medical?
Developed by the American Medical Association (AMA), the Current Procedural Terminology (CPT®) is “the most widely accepted medical nomenclature used to report medical procedures and services under public and private health insurance programs.”.
What software do providers use to submit claims?
Software. A lot of providers use a billing software to prepare and submit their claims. The really smart ones use an electronic medical record system that includes (or integrates with) a top-notch therapy billing software (hello, WebPT ).
When to use modifier 59?
Practices and facilities that offer their patients both physical and occupational therapy may need to affix modifier 59 or modifier XP to claims when patients receive same-day services that form NCCI edit pairs. According to Castin, modifier XP would be appropriate if, say, “an OT takes over treatment in the middle of a PT session” and modifier 59 would be appropriate if the payer doesn’t yet recognize X modifiers or there’s another reason to provide “otherwise linked services that should, given the circumstances, be reimbursed separately.” For example, you would use modifier 59 if, say, a PT provides gait training (97116) and an OT provides therapeutic activity (97530). As such, you’re notifying Medicare that the services—97116 and 97530—were performed separately and distinctly from one another and thus, should both be paid.
What is the most common claim form?
However, some payers—a dwindling few—do still accept paper ones. The most common form is the Universal Claim Form ( CMS 1500 ), although some payers may request that you use their own.
How long does it take for a physician to sign a plan of care?
Initial certification: Medicare requires ordering physicians to “approve or certify the plan of care via signature in a timely manner (within 30 days of the evaluation).”. The initial certification covers the first 90 days of treatment.
When will rehab therapist assistants be paid?
In the 2019 final rule, CMS announced that, beginning in 2022, it will only pay 85% of services performed either in full or in part by a rehab therapist assistant. Thus, beginning in 2020, if a PTA performs at least 10% of a given service, then you must affix the CQ modifier to the claim line for that service, notifying Medicare about the assistant’s participation in the service. That said, payment reductions won’t occur until two years later.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
Refer to Local Coverage Determination (LCD) L35036, Therapy and Rehabilitation Services (PT, OT), for reasonable and necessary requirements and frequency limitations. The Current Procedural Terminology (CPT)/Healthcare Common Procedure Coding System (HCPCS) code (s) may be subject to National Correct Coding Initiative (NCCI) edits.
ICD-10-CM Codes that Support Medical Necessity
It is the provider's responsibility to select codes carried out to the highest level of specificity and selected from the ICD-10-CM code book appropriate to the year in which the service is rendered for the claim (s) submitted.
ICD-10-CM Codes that DO NOT Support Medical Necessity
All those not listed under the "ICD-10 Codes that Support Medical Necessity" section.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
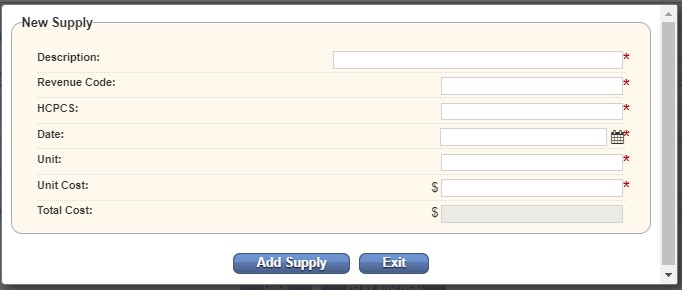
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
What is a re-evaluation in Medicare?
The AOTA describes a re-evaluation as the “reappraisal of the patient’s performance and goals to determine the type and amount of change that has taken place. Medicare and other third-party payers may have particular rules about when a re-evaluation may be reimbursed.
What is the AMA CPT?
In sum, the AMA CPT descriptions provide the basics of when a re-evaluation may be billed and what must be included in a PT and OT re-eval. You should note that Medicare and other payers can and sometimes do impose additional conditions that must be met to be paid for a reevaluation.
Why are therapists uncertain about re-evaluation?
Therapists are understandably uncertain as to when a re-evaluation can be billed because of conflicting terminology and confusion with “reassessment” requirements in PT and OT Acts. To determine if and when a re-evaluation is billable, we need to look at all of the following rules:
What is the time required for a standardized patient assessment?
2. Revised plan of care using a standardized patient assessment instrument and/or measurable assessment of functional outcome. Typically, 20 minutes are spent face-to-face with the patient and/or family.
Does Tricare have a re-eval?
The major commercial payers and Tricare do not have any unique guidance regarding re-evals. Their PT/OT policies basically include the AMA’s CPT descriptions for 97164 and 97168 if they include anything at all. Medicare’s more restrictive re-evaluation rules do not necessarily apply to these payers.
Is a re-evaluation required by Medicare?
Under Medicare guidelines, a re-evaluation is medically necessary (and therefore payable) only if the therapist determines that the patient has had a significant improvement, or decline, or other change in his or her condition or functional status that was not anticipated in the POC (emphasis added).
How many minutes of therapy do you need for Medicare?
The 8-Minute Rule. The 8-Minute rule as known as “the eight rule” specifies how many support unit therapists will bill Medicare for the given service date. In order to obtain reimbursement from Medicare for a time-based code, you must have direct treatment for at least eight minutes, according to the law. However, although it sounds basic, there ...
When is a POC change required?
Change into the POC is required if the patient is unable to respond to the treatment given in the current POC. You discover additional clinical findings in the course of treatment, which are somehow similar to the original treating condition.
What is an ABN in Medicare?
ABNs. Patients should sign an Advance Beneficiary Notice of Noncoverage (ABN) in order to offer Medicare patients services that they consider are not covered by Medicare or not required medically. This means that the patient will bear the financial cost of treatment if claims are declined by Medicare. Tags.
What is the therapy cap?
The Therapy Cap. The therapy cap was planned as a provisional solution to regulate Medicare costs and was announced as part of the Balanced Budget Act (BBA) of 1997. Despite a long-term force to cancel the cap, Congress lasted to renew the cap every year from its establishment.
What does the GA modifier mean on a claim?
If you declare an ABN because you think that specific services are not reasonable and medically required, then the GA modifier should be incorporated into the claim to indicate that you have an ABN on file.
Can you waive copays?
Copays. If he or she is expected to pay a copayment through your patient’s policy, you can receive the payment when you offer your services. In most cases, waiving copayments or deductibles isn’t a good idea. There are however other avenues in which you can offer support to patients in need.
Do physical therapists have to have billing information?
Yeah, no wonder you’ve got less time than you would like to keep up with all the ins and outs of physical therapy billing. For a physical therapist, it is necessary to have thorough information and all ins and outs of physical therapy billing. The following are the most important rules for physical therapy billing.
How long do you have to bill Medicare for therapy?
According to the rule, you must provide direct treatment for at least eight minutes in order to receive reimbursement from Medicare for a time-based code. But, while it sounds simple, there are some tricky 8-Minute Rule scenarios that could trip you up.
What is an ABN in Medicare?
In order to provide Medicare patients with services that you believe are either not covered by Medicare or not medically necessary (e.g., the services extend beyond the therapy cap ), you must have your patient sign an Advance Beneficiary Notice of Noncoverage (ABN), thereby indicating that he or she will accept financial responsibility if—but really more like when—Medicare denies the claim.
What is billable time?
1. Billable Time. To put it simply, billable time is time spent treating a patient. However, there are some nuances to keep in mind. For instance, you can’t bill for: unskilled prep time, multiple timed units due to multiple therapists, rest periods or other break times, supervision, or.
What is one on one therapy?
A one-on-one service is an individual therapy service—one that involves direct, one-on-one contact with a patient. While a group service still requires constant attendance, it does not involve one-on-one contact with each patient. Rather, according to CMS, it “consists of simultaneous treatment to two or more patients who may or may not be doing the same activities.”
Can you round up your billable time?
Additionally, when calculating your billable time, you shouldn’t ever round up . However, you can bill for evaluations and reevaluations—in some cases. Most payers, including Medicare, allow therapists to bill for the initial evaluations necessary to establish plans of care.
Can you waive copays?
If your patient’s insurance requires him or her to pay a copay, you can collect that payment when you provide your services. In most cases, it is not a good idea to waive copayments or deductibles. However, there are other ways you can provide financial assistance to patients who need it. To learn more about what your payers consider acceptable when it comes to helping patients cover the cost of your services, thoroughly read your insurance contracts. If you still come up empty-handed, contact your payers directly.
Can a therapist bill Medicare Part A?
However, therapists who bill under Medicare Part A may bill separate, full treatment sessions with a patient —as long as each therapist is of a different discipline and provides different treatments to the same patient at the same time. For clarity on billing for co-treatment—and a few examples—check out this resource. 4.
A Current Patient Develops A Newly Diagnosed, Related Condition.
A Current Patient Develops A Newly Diagnosed, Unrelated Condition.
- Use: Initial Evaluation (97161–97163) Conversely, when a patient with an active plan of care presents with a second condition that is totally unrelated to the primary issue, you should select the appropriate initial evaluation code. The nuance for therapists to remember is that a re-evaluation is triggered by a significant clinical change in the co...
A Patient Undergoes Surgery Mid-Plan of Care.
- Use: Re-evaluation (97164) Re-evaluations also may be appropriate for patients who received therapy treatment prior to surgery and then returned for additional rehabilitation after surgery. The catch in this situation is that some commercial payers may consider the post-op treatment period a new episode of care, in which case you’d need to use an evaluation code. Example: You treat …
Introduction
What Are The Codes?
- The International Classification of Diseases
In order to successfully bill for your services, you’ll need to diagnose your patients’ conditions in a manner that demonstrates the medical necessity of those services—and you’ll need to do so using the latest version of the International Classification of Diseases (ICD), which, as of October 2015… - The Current Procedural Terminology
Developed by the American Medical Association (AMA), the Current Procedural Terminology (CPT®) is “the most widely accepted medical nomenclature used to report medical procedures and services under public and private health insurance programs.” According to the …
What’s The Terminology?
- Looking for a refresher on your billing terminology? Here are some definitions we’ve adapted from this APTA resource and this WebPT oneto bring you back up to speed: 1. Treatment:Includes all therapeutic services. 2. Time-based (constant attendance) CPT codes:These codes allow for variable billing in 15-minute increments when a practitioner provides a patient with one-on-one s…
What Are The Forms?
- Today, most payers—and providers—prefer electronic claim forms. However, some payers—a dwindling few—do still accept paper ones. The most common form is the Universal Claim Form (CMS 1500), although some payers may request that you use their own. Once you provide your services, you’ll submit a bill to either your patientor a third-party payer. Occasionally, you may act…
What’s The Process?
- Get credentialed.
If you haven’t already received credentialing, you may want to consider changing that. Being credentialed by an insurance company allows you to become an in-network provider, which may help you reach—and serve—a larger pool of potential patients. Some payers—like Medicare—do … - Negotiate payer contracts.
Just as rules are (sometimes) meant to be broken, contracts are (always) meant to be negotiated. This especially holds true when it comes to your private payer contracts. After all, these rates establish what you’re able to earn—and that number should be an accurate reflection of the valu…