5 Tips on How to Bill Medicare for DME Supplies
- Show Proof of “Reasonable and Necessary” Supplies. Every document you submit with a claim needs to show medical necessity. ...
- Review Documents to Ensure Legibility. All documents must be legible, whether you’re submitting an electronic or paper claim. ...
- Be Clear and Concise. ...
- Use Up-to-Date Codes and Modifiers. ...
- Submit Claim Documents. ...
How to file your claims with Medicare?
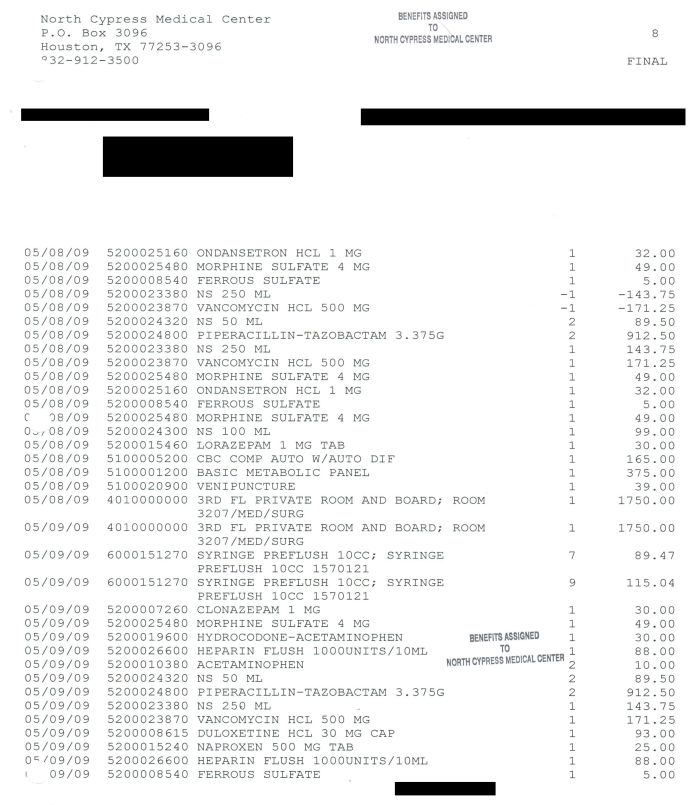
- The date of your treatment
- Where you received treatment (hospital, doctor’s office, etc.)
- Description of each treatment or medical supply received
- Itemized charge (s) for each treatment or medical supply
Do I need to file any claims with Medicare?
You usually don’t have to file a Medicare claim. Doctors or hospitals typically file Original Medicare claims for you. Private insurers that administer Medicare Advantage and Part D plans handle those claims. In the rare cases when you have to file a claim, Medicare provides a form to download and mail in.
How do I make a Medicare claim?
Claim Medicare benefits at your doctor’s office. The quickest and easiest way to claim is at your doctor’s office straight after you pay. To do this you need to both: be enrolled in Medicare. show your Medicare card. If your doctor bulk bills, you don’t need to pay. When you pay at the doctor’s office, ask if they can make an electronic ...
How long do you have to submit a claim to Medicare?
Medicare Part A and B claims are submitted directly to Medicare by the healthcare provider (such as a doctor, hospital, or lab). Medicare then takes approximately 30 days to process and settle each claim. However, if there are queries or issues with the claim, the process can be a lot longer.

Can I submit claims directly to Medicare?
If you have Original Medicare and a participating provider refuses to submit a claim, you can file a complaint with 1-800-MEDICARE. Regardless of whether or not the provider is required to file claims, you can submit the healthcare claims yourself.
What form do you use to bill Medicare?
The Form CMS-1450, also known as the UB-04, is the standard claim form to bill Medicare Administrative Contractors (MACs) when a paper claim is allowed.
What is the first step in submitting Medicare claims?
The first thing you'll need to do when filing your claim is to fill out the Patient's Request for Medical Payment form. ... The next step in filing your own claim is to get an itemized bill for your medical treatment.More items...•
What is the KX modifier for Medicare?
The KX modifier, described in subsection D., is added to claim lines to indicate that the clinician attests that services at and above the therapy caps are medically necessary and justification is documented in the medical record.
What is the difference between UB 04 and CMS 1500?
The UB-04 (CMS-1450) form is the claim form for institutional facilities such as hospitals or outpatient facilities. This would include things like surgery, radiology, laboratory, or other facility services. The HCFA-1500 form (CMS-1500) is used to submit charges covered under Medicare Part B.
What is the difference between UB 04 and UB 92?
A number of things were added to the UB92 form when it underwent the revision to become UB04. The main change is the addition of the field in which to input a National Provider Identifier (NPI). Additional fields were also added like more diagnosis code fields.
How do doctors bill Medicare?
Payment for Medicare-covered services is based on the Medicare Physicians' Fee Schedule, not the amount a provider chooses to bill for the service. Participating providers receive 100 percent of the Medicare Allowed Amount directly from Medicare.
What is an ICN number and when is it needed?
What is an ICN number and when is it needed? It is a 15-digit number that uniquely identifies one payment of one claim (NC Medicaid). This number is required when performing a “void” or “replacement” of an original paid claim.
How do I fill out a CMS 1500?
14:5319:58How-to Accurately Fill Out the CMS 1500 Form for Faster PaymentYouTubeStart of suggested clipEnd of suggested clipField 1 is the very first field on the CMS 1500 form and it tells the insurance carrier the categoryMoreField 1 is the very first field on the CMS 1500 form and it tells the insurance carrier the category of insurance that the policy falls into. It can be left blank.
What is KY modifier used for?
The KY Modifier is used to identify a wheelchair accessory that is for use with a base that was not part of the competitive bid program. This modifier is only for use in former competitive bid areas and is important to ensure appropriate pricing on the wheelchair accessories.
What is the KF modifier used for?
Although not associated with a specific , the KF modifier is required for claim submission of this HCPCS code as well. This information will be added to the applicable -related Policy Articles in an upcoming revision....Publication History.Publication DateDescription08/29/19Originally PublishedFeb 19, 2020
What is GY modifier?
The GY modifier is used to obtain a denial on a Medicare non-covered service. This modifier is used to notify Medicare that you know this service is excluded. The explanation of benefits the patient get will be clear that the service was not covered and that the patient is responsible.
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
How much is Medicare reimbursement for 2020?
Reimbursements match similar in-person services, increasing from about $14-$41 to about $60-$137, retroactive to March 1, 2020. In addition, Medicare is temporarily waiving the audio-video requirement for many telehealth services during the COVID-19 public health emergency. Codes that have audio-only waivers during the public health emergency are ...
What is the CPT code for Telehealth?
Medicare increased payments for certain evaluation and management visits provided by phone for the duration of the COVID-19 public health emergency: Telehealth CPT codes 99441 (5-10 minutes), 99442 (11-20 minutes), and 99443 (20-30 minutes)
Does Medicare cover telehealth?
Telehealth codes covered by Medicare. Medicare added over one hundred CPT and HCPCS codes to the telehealth services list for the duration of the COVID-19 public health emergency. Telehealth visits billed to Medicare are paid at the same Medicare Fee-for-Service (FFS) rate as an in-person visit during the COVID-19 public health emergency.
How long does it take for Medicare to process a claim?
The MAC evaluates (or adjudicates) each claim sent to Medicare, and processes the claim. This process usually takes around 30 days .
What form do you need to bill Medicare?
If a biller has to use manual forms to bill Medicare, a few complications can arise. For instance, billing for Part A requires a UB-04 form (which is also known as a CMS-1450). Part B, on the other hand, requires a CMS-1500. For the most part, however, billers will enter the proper information into a software program and then use ...
What is 3.06 Medicare?
3.06: Medicare, Medicaid and Billing. Like billing to a private third-party payer, billers must send claims to Medicare and Medicaid. These claims are very similar to the claims you’d send to a private third-party payer, with a few notable exceptions.
What is a medical biller?
In general, the medical biller creates claims like they would for Part A or B of Medicare or for a private, third-party payer. The claim must contain the proper information about the place of service, the NPI, the procedures performed and the diagnoses listed. The claim must also, of course, list the price of the procedures.
Is it harder to bill for medicaid or Medicare?
Billing for Medicaid. Creating claims for Medicaid can be even more difficult than creating claims for Medicare. Because Medicaid varies state-by-state, so do its regulations and billing requirements. As such, the claim forms and formats the biller must use will change by state. It’s up to the biller to check with their state’s Medicaid program ...
Can you bill Medicare for a patient with Part C?
Because Part C is actually a private insurance plan paid for, in part, by the federal government, billers are not allowed to bill Medicare for services delivered to a patient who has Part C coverage. Only those providers who are licensed to bill for Part D may bill Medicare for vaccines or prescription drugs provided under Part D.
Do you have to go through a clearinghouse for Medicare and Medicaid?
Since these two government programs are high-volume payers, billers send claims directly to Medicare and Medicaid. That means billers do not need to go through a clearinghouse for these claims, and it also means that the onus for “clean” claims is on the biller.
How long does it take to see a Medicare claim?
Log into (or create) your secure Medicare account. You’ll usually be able to see a claim within 24 hours after Medicare processes it. A notice you get after the doctor, other health care provider, or supplier files a claim for Part A or Part B services in Original Medicare.
What is Medicare Part A?
Check the status of a claim. To check the status of. Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. or.
What is MSN in Medicare?
The MSN is a notice that people with Original Medicare get in the mail every 3 months. It shows: All your Part A and Part B-covered services or supplies billed to Medicare during a 3-month period. What Medicare paid. The maximum amount you may owe the provider. Learn more about the MSN, and view a sample.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
Is Medicare paid for by Original Medicare?
Medicare services aren’t paid for by Original Medicare. Most Medicare Advantage Plans offer prescription drug coverage. or other. Medicare Health Plan. Generally, a plan offered by a private company that contracts with Medicare to provide Part A and Part B benefits to people with Medicare who enroll in the plan.
Does Medicare Advantage offer prescription drug coverage?
Medicare Advantage Plans may also offer prescription drug coverage that follows the same rules as Medicare drug plans. Check your Explanation of Benefits (EOB). Your Medicare drug plan will mail you an EOB each month you fill a prescription. This notice gives you a summary of your prescription drug claims and costs.
When Do I Need to File A Claim?
- You should only need to file a claim in very rare cases
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicar…
How Do I File A Claim?
- Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
Where Do I Send The Claim?
- The address for where to send your claim can be found in 2 places: 1. On the second page of the instructions for the type of claim you’re filing (listed above under "How do I file a claim?"). 2. On your "Medicare Summary Notice" (MSN). You can also log into your Medicare accountto sign up to get your MSNs electronically and view or download them anytime. You need to fill out an "Author…