
To file your claim, you’ll need to fill out a Patient’s Request for Medical Payment Medical billing is a payment practice within the United States health system. The process involves a healthcare provider submitting, following up on, and appealing claims with health insurance companies in order to receive payment for services rendered; such as testing, treatments, and procedures. The same process is used for most insurance companies, whether they are private companies or g…Medical billing
How to file your claims with Medicare?
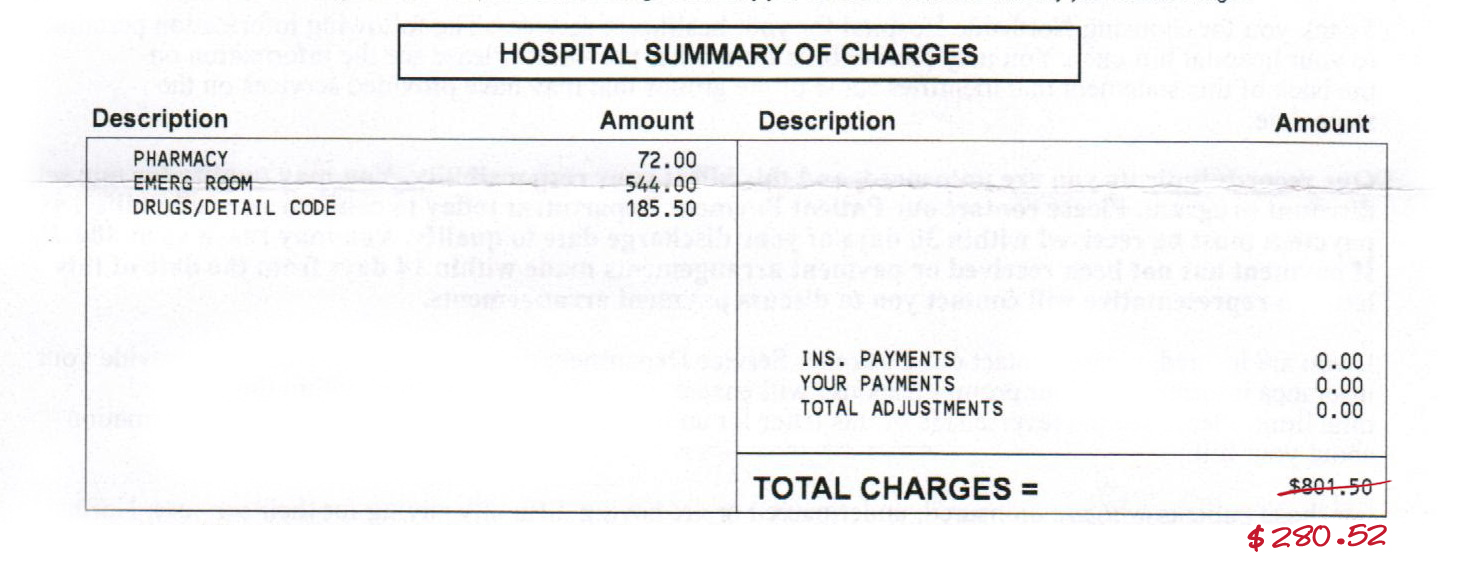
- The date of your treatment
- Where you received treatment (hospital, doctor’s office, etc.)
- Description of each treatment or medical supply received
- Itemized charge (s) for each treatment or medical supply
Do I need to file any claims with Medicare?
You usually don’t have to file a Medicare claim. Doctors or hospitals typically file Original Medicare claims for you. Private insurers that administer Medicare Advantage and Part D plans handle those claims. In the rare cases when you have to file a claim, Medicare provides a form to download and mail in.
How do I make a Medicare claim?
Claim Medicare benefits at your doctor’s office. The quickest and easiest way to claim is at your doctor’s office straight after you pay. To do this you need to both: be enrolled in Medicare. show your Medicare card. If your doctor bulk bills, you don’t need to pay. When you pay at the doctor’s office, ask if they can make an electronic ...
How long do you have to submit a claim to Medicare?
Medicare Part A and B claims are submitted directly to Medicare by the healthcare provider (such as a doctor, hospital, or lab). Medicare then takes approximately 30 days to process and settle each claim. However, if there are queries or issues with the claim, the process can be a lot longer.
Can I submit claims directly to Medicare?
If you have Original Medicare and a participating provider refuses to submit a claim, you can file a complaint with 1-800-MEDICARE. Regardless of whether or not the provider is required to file claims, you can submit the healthcare claims yourself.
What form is used to send claims to Medicare?
CMS-1500 claim formThe CMS-1500 claim form is used to submit non-institutional claims for health care services provided by physicians, other providers and suppliers to Medicare.
What is the KX modifier for Medicare?
The KX modifier, described in subsection D., is added to claim lines to indicate that the clinician attests that services at and above the therapy caps are medically necessary and justification is documented in the medical record.
What is the first step in submitting Medicare claims?
The first thing you'll need to do when filing your claim is to fill out the Patient's Request for Medical Payment form. ... The next step in filing your own claim is to get an itemized bill for your medical treatment.More items...•
What is the difference between UB 04 and CMS 1500?
The UB-04 (CMS-1450) form is the claim form for institutional facilities such as hospitals or outpatient facilities. This would include things like surgery, radiology, laboratory, or other facility services. The HCFA-1500 form (CMS-1500) is used to submit charges covered under Medicare Part B.
How do I fill out a CMS 1500 for Medicare?
14:5319:58How-to Accurately Fill Out the CMS 1500 Form for Faster PaymentYouTubeStart of suggested clipEnd of suggested clipField 1 is the very first field on the CMS 1500 form and it tells the insurance carrier the categoryMoreField 1 is the very first field on the CMS 1500 form and it tells the insurance carrier the category of insurance that the policy falls into. It can be left blank.
What is KY modifier used for?
The KY Modifier is used to identify a wheelchair accessory that is for use with a base that was not part of the competitive bid program. This modifier is only for use in former competitive bid areas and is important to ensure appropriate pricing on the wheelchair accessories.
What is the KF modifier used for?
Although not associated with a specific , the KF modifier is required for claim submission of this HCPCS code as well. This information will be added to the applicable -related Policy Articles in an upcoming revision....Publication History.Publication DateDescription08/29/19Originally PublishedFeb 19, 2020
What is a RR modifier used for?
Hence when DME is a rental, the modifier RR is used for enhancing billing and collections. It comes under the Level II HCPCS modifiers which consist of two digits beginning from AA through VP and usually comprise alpha/alphanumeric characters. This modifier must be used on all claim forms for rental DME.
Does Medicare accept secondary paper claims?
Currently, Medicare does not accept electronically filed claims when there is more than one payer primary to Medicare. Claims that involve more than one primary payer to Medicare must be submitted on the 1500 paper claim form, with all appropriate attachments.
How does Medicare reimburse physician services?
Traditional Medicare reimbursements Instead, the law states that providers must send the claim directly to Medicare. Medicare then reimburses the medical costs directly to the service provider. Usually, the insured person will not have to pay the bill for medical services upfront and then file for reimbursement.
Who is eligible for Medicare reimbursement?
You must be a retired member or qualified survivor who is receiving a pension and is eligible for a health subsidy, and enrolled in both Medicare Parts A and B. 2.
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
How Do I File a Medicare Reimbursement Claim?
To file your claim, you’ll need to fill out a Patient’s Request for Medical Payment form. You then send both this form and the bill from your provider to your state’s Medicare contractor.
What To Submit With The Claim
When filling out the form, you must choose the service type then provide the following information:
Where to Send Your Medicare Claim
Each state has a different address to send your claim. There are two places where you can find the address. You can find the address on the claim form on page two, or on your quarterly Medicare Summary Notice.
What if My Healthcare Provider is Not Sending the Claims Promptly?
The first thing you should do is call the provider and ask them to send your claim. If they do not file the claim, call Medicare and find out how much time is left to file the claim. If it’s close to the end of the allowed time and your healthcare provider has not filed the claim, you should go ahead and file the claim.
FAQs
When a claim is submitted to Medicare, it should come straight from the doctor or other provider of services. If for some reason they don’t submit the claim on your behalf, then you can call Medicare and submit it yourself. You can also submit the claim online.
How long does it take for Medicare to process a claim?
Medicare claims to providers take about 30 days to process. The provider usually gets direct payment from Medicare. What is the Medicare Reimbursement fee schedule? The fee schedule is a list of how Medicare is going to pay doctors. The list goes over Medicare’s fee maximums for doctors, ambulance, and more.
What happens if you see a doctor in your insurance network?
If you see a doctor in your plan’s network, your doctor will handle the claims process. Your doctor will only charge you for deductibles, copayments, or coinsurance. However, the situation is different if you see a doctor who is not in your plan’s network.
What to do if a pharmacist says a drug is not covered?
You may need to file a coverage determination request and seek reimbursement.
Does Medicare cover out of network doctors?
Coverage for out-of-network doctors depends on your Medicare Advantage plan. Many HMO plans do not cover non-emergency out-of-network care, while PPO plans might. If you obtain out of network care, you may have to pay for it up-front and then submit a claim to your insurance company.
Do participating doctors accept Medicare?
Most healthcare doctors are “participating providers” that accept Medicare assignment. They have agreed to accept Medicare’s rates as full payment for their services. If you see a participating doctor, they handle Medicare billing, and you don’t have to file any claim forms.
Do you have to pay for Medicare up front?
But in a few situations, you may have to pay for your care up-front and file a claim asking Medicare to reimburse you. The claims process is simple, but you will need an itemized receipt from your provider.
Do you have to ask for reimbursement from Medicare?
If you are in a Medicare Advantage plan, you will never have to ask for reimbursement from Medicare. Medicare pays Advantage companies to handle the claims. In some cases, you may need to ask the company to reimburse you. If you see a doctor in your plan’s network, your doctor will handle the claims process.
How long does it take to see a Medicare claim?
Log into (or create) your secure Medicare account. You’ll usually be able to see a claim within 24 hours after Medicare processes it. A notice you get after the doctor, other health care provider, or supplier files a claim for Part A or Part B services in Original Medicare.
What is Medicare Part A?
Check the status of a claim. To check the status of. Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. or.
What is MSN in Medicare?
The MSN is a notice that people with Original Medicare get in the mail every 3 months. It shows: All your Part A and Part B-covered services or supplies billed to Medicare during a 3-month period. What Medicare paid. The maximum amount you may owe the provider. Learn more about the MSN, and view a sample.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
Is Medicare paid for by Original Medicare?
Medicare services aren’t paid for by Original Medicare. Most Medicare Advantage Plans offer prescription drug coverage. or other. Medicare Health Plan. Generally, a plan offered by a private company that contracts with Medicare to provide Part A and Part B benefits to people with Medicare who enroll in the plan.
Does Medicare Advantage offer prescription drug coverage?
Medicare Advantage Plans may also offer prescription drug coverage that follows the same rules as Medicare drug plans. Check your Explanation of Benefits (EOB). Your Medicare drug plan will mail you an EOB each month you fill a prescription. This notice gives you a summary of your prescription drug claims and costs.
What is the CMS format for billing?
You may use roster billing format or submit individual claims using the CMS-1500 form (PDF) or the 837P electronic format. CMS systems will accept roster bills for 1 or more patients that get the same type of shot on the same date of service.
What is the MBI for Medicare?
All Medicare patients have a red, white, and blue Medicare card with an MBI, including those enrolled in a Medicare Advantage Plan. If your patients don’t have their Original Medicare card or don’t know their MBI, use the MBI look-up tool in your MAC’s secure portal (PDF).
Do you have to include the code on a claim for a free shot?
Don’t include the vaccine codes on the claim when the vaccines are free. You must administer the vaccine with no out-of-pocket cost to your patients for the vaccine or administration of the vaccine. If you want to administer the vaccine for free, you don’t have to submit a claim to Medicare, Medicaid, or another insurer.
Can you bill Medicare for additional in home care?
You should only bill for the additional in-home payment amount if the sole purpose of the visit is to administer a COVID-19 vaccine. You shouldn’t bill for the additional amount if you provide and bill Medicare for another service in the same home on the same date.

When Do I Need to File A Claim?
- You should only need to file a claim in very rare cases
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicar…
How Do I File A Claim?
- Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
What Do I Submit with The Claim?
- Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1. The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2. The itemized bill from your doctor, supplier, or other health care provider 3. A letter explaining in detail your reason for subm…