
The provider would have to write-off the $7.00 difference between the provider's actual charge and the amounts paid by the primary and secondary payers ($72.00 - $65.00 = $7.00). Example 2 Provider submits a claim for procedure code 99214 with a submitted amount of $72.00
Full Answer
How do you calculate allowed amount for insurance write off?
Jan 22, 2020 · $252 per month for those who paid Medicare taxes for 30-39 quarters. Medicare Part B premium. While zero-premium liability is typical for Part A, the standard for Medicare Part B is a premium that changes annually, determined by modified adjusted gross income and tax filing status. For 2020, the standard monthly rate is $144.60.
How do you calculate primary and secondary Medicare payments?
Oct 08, 2018 · The provider would have to write-off the $7.00 difference between the provider's actual charge and the amounts paid by the primary and secondary payers ($72.00 - $65.00 = $7.00). Example 2 Provider submits a claim for procedure code 99214 with a …
How much can you deduct from Medicare premiums?
Get an estimate of when you're eligible for Medicare and your premium amount. If you don't see your situation, contact Social Security (or the Railroad Retirement Board if you get railroad benefits) to learn more about your specific eligibility or premium.
How is the beneficiary's obligation for Medicare calculated?
The difference between the billed amount and the system allowed amount will be the write off, if the EOB allowed amount is less than the system allowed amount. Otherwise the difference between the billed amount and the EOB allowed amount would be the write off.

What is the write-off process in medical billing?
Generally, a write-off refers to any amount deducted from a medical bill. Offices often allow write-offs when they do not expect to collect payment. While there are several types of write-offs, including those for hardship care, bad debt, and small balances, the contractual adjustment is one of the most frequent.
What does Medicare contractual write-off mean?
Contractual write off are those wherein the excess of billed amount over the carrier's allowed amount is written off. The fee schedules of each carrier will be loaded in the billing system. When you are posting the EOBs these fee schedules in the system also called system allowed amount would pop up.
How are Medicare payments calculated?
Medicare primary payment is $375 × 80% = $300.Primary allowed of $500 is the higher allowed amount.Primary allowed minus primary paid is $500 - $400 = $100.The lower of Step 1 or 3 is $100. ( Medicare will pay $100)Nov 19, 2021
What is estimated write-off Adjustment?
The write-off adjustment enables you to adjust account balances that you do not think will be paid. There are five pre-defined write-off types, and you can customize them for your practice. More... When you enter a write-off adjustment, the software expects the amount entered to be a negative amount.
How is billed amount calculated in medical billing?
It is the balance of allowed amount – Co-pay / Co-insurance – deductible. The paid amount may be either full or partial. i.e. Full allowed amount being paid or a certain percentage of the allowed amount being paid. If the billed amount is $100.00 and the insurance allows $80.00 but the payment amount is $60.00.
How do I find out my deductible?
A deductible can be either a specific dollar amount or a percentage of the total amount of insurance on a policy. The amount is established by the terms of your coverage and can be found on the declarations (or front) page of standard homeowners and auto insurance policies.
How is Medicare secondary payment calculated?
The Medicare secondary payment is the lowest of the following: (1) The gross amount payable by Medicare (that is, the amount payable without considering the effect of the Medicare deductible and coinsurance or the payment by the primary payer), minus the applicable Medicare deductible and coinsurance amounts.
What income is used to determine Medicare premiums?
modified adjusted gross incomeMedicare uses the modified adjusted gross income reported on your IRS tax return from 2 years ago. This is the most recent tax return information provided to Social Security by the IRS.
What is Medicare Part A deductible for 2021?
Medicare Part A Premiums/Deductibles The Medicare Part A inpatient hospital deductible that beneficiaries will pay when admitted to the hospital will be $1,484 in 2021, an increase of $76 from $1,408 in 2020.Nov 6, 2020
What is the difference between contractual adjustment and write-off?
A contractual adjustment is the amount that the carrier agrees to accept as a participating provider with the insurance carrier. A write off is the amount that cannot be collected from patient due to several issues. Documentation is required for any patient balance adjustment for auditing purposes.
What does PPO write-off mean?
The difference between the actual charge and the allowable charge, which a network provider cannot charge to a patient who belongs to a health insurance plan that utilizes the provider network. See Allowable Charge for more information.
What does bad debt write-off mean on a medical bill?
Bad-Debt Write-off: Cancelling or removing a balance from an account after several unsuccessful attempts to collect. The balance is written off as bad debt. This doesn't, however, dismiss responsibility for payment. A collection agency may be assigned to collect this debt from the policyholder.
What is the Medicare Physician Fee Schedule?
The Medicare Physician Fee Schedule (MPFS) uses a resource-based relative value system (RBRVS) that assigns a relative value to current procedural terminology (CPT) codes that are developed and copyrighted by the American Medical Association (AMA) with input from representatives of health care professional associations and societies, including ASHA. The relative weighting factor (relative value unit or RVU) is derived from a resource-based relative value scale. The components of the RBRVS for each procedure are the (a) professional component (i.e., work as expressed in the amount of time, technical skill, physical effort, stress, and judgment for the procedure required of physicians and certain other practitioners); (b) technical component (i.e., the practice expense expressed in overhead costs such as assistant's time, equipment, supplies); and (c) professional liability component.
What are the two categories of Medicare?
There are two categories of participation within Medicare. Participating provider (who must accept assignment) and non-participating provider (who does not accept assignment). You may agree to be a participating provider (who does not accept assignment). Both categories require that providers enroll in the Medicare program.
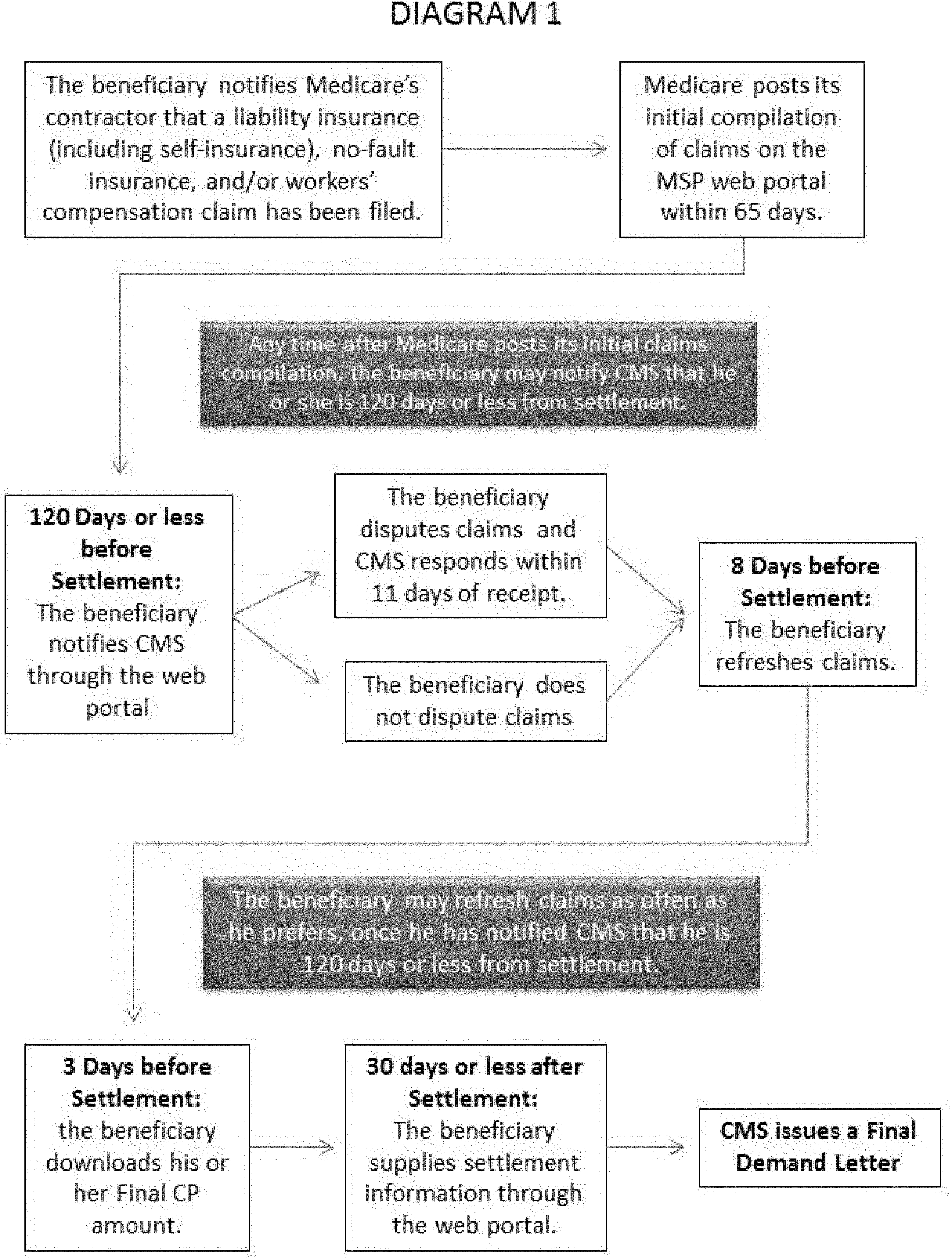
What is MSP payment?
MSP Payment Calculation Examples. The Medicare Secondary Payer (MSP) process may pay secondary benefits when a physician, supplier, or beneficiary submits a claim to the beneficiary's primary insurance and the primary insurance does not pay the entire charge. Medicare will not make a secondary payment if the physician/supplier accepts, ...
What is an allowed amount?
Allowed Amount (SA): The allowed amount is the amount the primary insurance company allowed for the submitted charges. This may also be referred to on an EOB as eligible charges. This amount should equal the OTAF amount.
Is Medicare a supplemental insurance?
Important: Medicare is not a supplemental insurance, even when secondary, and Medicare's allowable is the deciding factor when determining the patient's liability. The payment information received from the primary insurer will determine the amount Medicare will pay as secondary payer.
What happens if you don't meet the therapy threshold?
That is, the PC Pricer changes the HIPPS code you entered to reflect the HIPPS code that applies for fewer than 10 therapy visits. This change appears on the payment report in the following fields:
Does LUPA claim vary from typical claims?
The entry of LUPA claims does not vary from the entry of typical claims. Enter all the required claim fields, including the HIPPS code of the claim and the numbers of visits.
What is a write off for a practice?
A write-off is an amount that a practice deducts from a charge and does not expect to collect, thereby “writing it off” the accounts receivable or list of monies owed them by payers or patients.
What is administrative write off?
Administrative write-offs are those approved by the manager based on service issues. For instance, if the practice assures the patient that they are participating with the patient’s insurance, then it turns out that the practice is not in-network, the manager may approve a write-off based on the practice’s error.
What is a contractual write off?
Contractual write-offs are the difference between the practice fee schedule and the allowable fee schedule you’ve agreed to accept.
What is a charity write off?
Charity write-offs are the difference between the practice fee schedule and anything collected. Charity write-offs may be in accordance with a community indigent care effort, a policy adhered to in a faith-led healthcare system, or a financial assistance program.
What is a bad debt write off?
Bad debt write-offs are balances that you have decided to write-off and not pursue further. These are balances that for whatever reason, you are forgiving forever. Collection agency write-offs are those that are written off the main A/R (accounts receivable) and transferred to a third-party collection agency to collect on your behalf.
What is prompt payment discount?
Prompt payment discounts and self-pay (no insurance) discounts are write-offs for patients paying in full at time of service, and/or patients who receive a discount off the retail price because they do not have insurance coverage.
What is allowable charge?
Allowable charges are available to participating providers to help avoid refund situations. They are for informational purposes and not intended for providers to establish allowable charges. Blue Cross regularly audits our allowable charge schedule to ensure that the allowable charge amounts are accurate.
What is co-insurance in insurance?
Co-insurance = Allowed amount – Paid amount – Write-off amount. • Deductible: Deductible is the amount the patient has to pay for his health care services, whereas only after the patient meets the deductible the health insurance plan starts its coverage. The patient has to meet the Deductibles every year.
Does a physician have to inform BCBSKS of the existence of agreements?
The physician agrees to fully and promptly inform BCBSKS of the existence of agreements under which such physician agrees to accept an amount for any and or all services as payment in full which is less than the amount such physician accepts from BCBSKS as payment in full for such services.
Standard 20% Co-Pay
- All Part B services require the patient to pay a 20% co-payment. The MPFS does not deduct the co-payment amount. Therefore, the actual payment by Medicare is 20% less than shown in the fee schedule. You must make "reasonable" efforts to collect the 20% co-payment from the beneficiary.
Non-Participating Status & Limiting Charge
- There are two categories of participation within Medicare. Participating provider (who must accept assignment) and non-participating provider (who does not accept assignment). You may agree to be a participating provider (who does not accept assignment). Both categories require that providers enroll in the Medicare program. You may agree to be a participating provider with …
Facility & Non-Facility Rates
- The MPFS includes both facility and non-facility rates. In general, if services are rendered in one's own office, the Medicare fee is higher (i.e., the non-facility rate) because the pratitioner is paying for overhead and equipment costs. Audiologists receive lower rates when services are rendered in a facility because the facility incurs overhead/equipment costs. Skilled nursing facilities are the …
Geographic Adjustments: Find Exact Rates Based on Locality
- You may request a fee schedule adjusted for your geographic area from the Medicare Administrative Contractor (MAC) that processes your claims. You can also access the rates for geographic areas by going to the CMS Physician Fee Schedule Look-Up website. In general, urban states and areas have payment rates that are 5% to 10% above the national average. Likewise, r…
Multiple Procedure Payment Reductions
- Under the MPPR policy, Medicare reduces payment for the second and subsequent therapy, surgical, nuclear medicine, and advanced imaging procedures furnished to the same patient on the same day. Currently, no audiology procedures are affected by MPPR.