Once your application is submitted, you can check on its status by: Logging in to your My Social Security account Visiting your local Social Security office
Social Security Administration
The United States Social Security Administration is an independent agency of the U.S. federal government that administers Social Security, a social insurance program consisting of retirement, disability, and survivors' benefits. To qualify for most of these benefits, most workers pay Social …
Full Answer
How do I check the status of my revalidation request?
Revalidation letter – Confirm if you have been sent a revalidation request; this requires your NPI or PTAN. PECOS Tracking ID - Check the status of applications submitted through Internet-based PECOS; you need a tracking ID number. … … … … Please enter your PTAN or NPI to obtain a list of pending submissions currently in process.
When do you get a revalidation notice from Medicare?
You’ll receive a revalidation notice via email or U.S. postal mail about three to four months prior to your due date. Medicare Administrative Contractors (MACs) send notifications to providers, group practices, and non-DMEPOS suppliers.
What happens if I don’t revalidate my Medicare billing privileges?
Failing to revalidate on time could result in a hold on your Medicare reimbursement or deactivation of your Medicare billing privileges. If your Medicare billing privileges are deactivated, you’ll need to re-submit a complete Medicare enrollment application to reactivate your billing privileges.
Do providers need to revalidate?
Providers who are enrolled in Medicare solely to order, certify and/or prescribe or have opted out of Medicare, are not required to revalidate and will not appear on lookup tool Providers/Suppliers listed on website, with a due date, should submit their revalidation application.
How long is Medicare revalidation good for?
every 5 yearsAll providers and suppliers are required to revalidate their enrollment information every 5 years and every 3 years for DMEPOS suppliers. CMS also reserves the right to request off-cycle revalidations. 24.
How often is CMS revalidation?
every five yearsYou're required to revalidate—or renew—your enrollment record periodically to maintain Medicare billing privileges. In general, providers and suppliers revalidate every five years but DMEPOS suppliers revalidate every three years. CMS also reserves the right to request off-cycle revalidations.
How do I reactivate my Medicare?
Reactivation of Billing Privileges Otherwise, to reactivate enrollment billing privileges submit a completed CMS-855A and CMS-588 paper application or submit electronically via PECOS. Submit a copy of a voided check or bank confirmation letter with the CMS-588.
How do I revalidate Pecos?
1:057:06So to do this just submit an initial enrollment. You'll need to click on the new application buttonMoreSo to do this just submit an initial enrollment. You'll need to click on the new application button shown on the previous screen. And then this submission is what will count towards your revalidation.
What is Medicare recertification?
The recertification statement must contain an adequate written record of the reasons for the continued need for extended care services, the estimated period of time required for the patient to remain in the facility, and any plans, where appropriate, for home care.
What is the revalidation process?
Revalidation is based on a local evaluation of doctors' practice through appraisal. Through a formal link with an organisation, determined usually by employment or contracting arrangements, each doctor relates to a senior doctor in the organisation, the responsible officer.
What happens if my Medicare Part B lapses?
If you didn't get Part B when you're first eligible, your monthly premium may go up 10% for each 12-month period you could've had Part B, but didn't sign up. In most cases, you'll have to pay this penalty each time you pay your premiums, for as long as you have Part B.
Why is my Medicare showing inactive?
Depending on the type of Medicare plan you are enrolled in, you could potentially lose your benefits for a number of reasons, such as: You no longer have a qualifying disability. You fail to pay your plan premiums. You move outside your plan's coverage area.
Can you lose Medicare?
Yes, if you qualify for Medicare by disability or health problem, you could lose your Medicare eligibility. If you qualify for Medicare by age, you cannot lose your Medicare eligibility.
What does revalidate mean?
to validate again or anewDefinition of revalidate transitive verb. : to validate again or anew: such as. a : to make (something) legal or valid again Her mother had revalidated her Cuban teaching credentials and begun teaching school.— Linda Marx also : to grant official sanction to (something) again had to get his visa revalidated.
What is a CMS 855 form?
CMS 855A. Form Title. Medicare Enrollment Application - Institutional Providers.
How do I submit my Pecos 855R?
Providers and suppliers are able to submit their reassignment certifications either by signing section 6A and 6B of the paper CMS-855R application or, if completing the reassignment via Internet-based PECOS, by submitting signatures electronically or via downloaded paper certification statements (downloaded from www. ...
How long does it take to see a Medicare claim?
Log into (or create) your secure Medicare account. You’ll usually be able to see a claim within 24 hours after Medicare processes it. A notice you get after the doctor, other health care provider, or supplier files a claim for Part A or Part B services in Original Medicare.
What is Medicare Part A?
Check the status of a claim. To check the status of. Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. or.
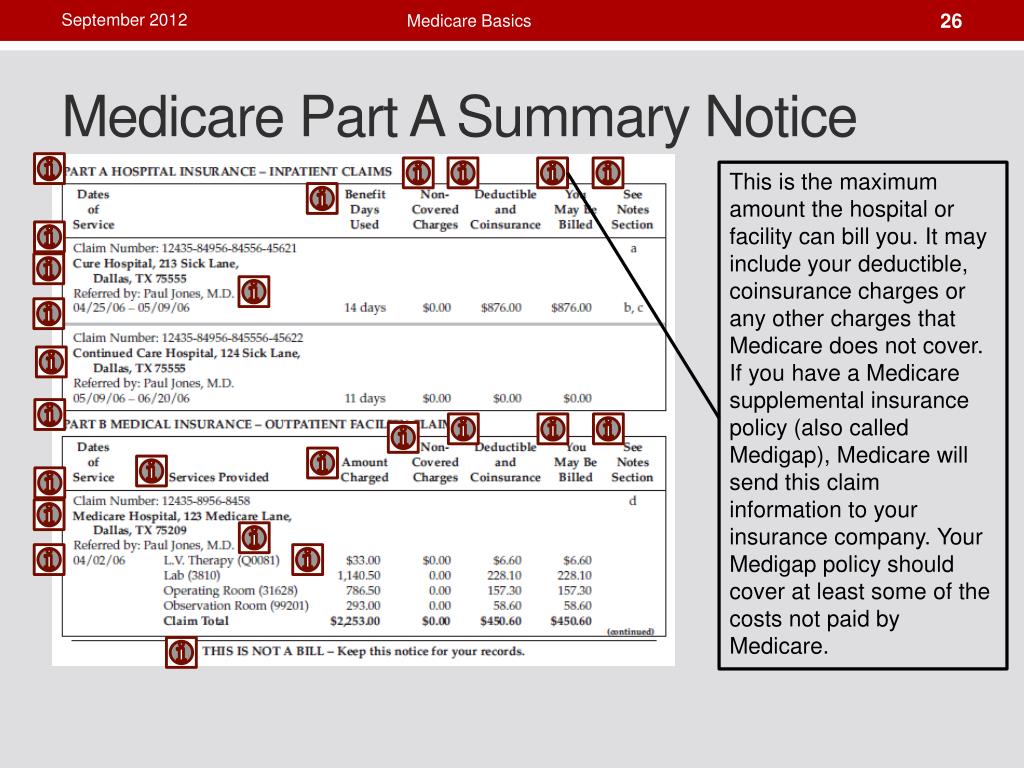
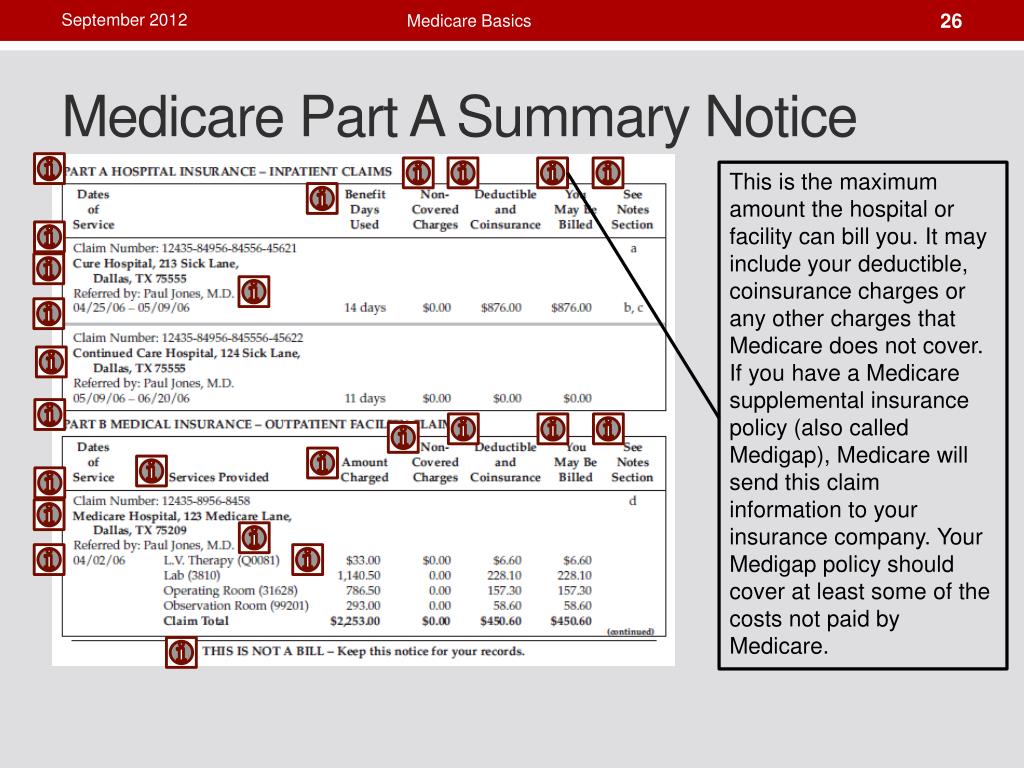
What is MSN in Medicare?
The MSN is a notice that people with Original Medicare get in the mail every 3 months. It shows: All your Part A and Part B-covered services or supplies billed to Medicare during a 3-month period. What Medicare paid. The maximum amount you may owe the provider. Learn more about the MSN, and view a sample.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
Is Medicare paid for by Original Medicare?
Medicare services aren’t paid for by Original Medicare. Most Medicare Advantage Plans offer prescription drug coverage. or other. Medicare Health Plan. Generally, a plan offered by a private company that contracts with Medicare to provide Part A and Part B benefits to people with Medicare who enroll in the plan.
Does Medicare Advantage offer prescription drug coverage?
Medicare Advantage Plans may also offer prescription drug coverage that follows the same rules as Medicare drug plans. Check your Explanation of Benefits (EOB). Your Medicare drug plan will mail you an EOB each month you fill a prescription. This notice gives you a summary of your prescription drug claims and costs.
How often do you have to revalidate Medicare?
The Patient Protection and Affordable Care Act established a requirement for all enrolled providers/suppliers to revalidate their Medicare enrollment information roughly every five years. Revalidation is the process of reviewing all information that is on file with Medicare is correct. All information can be found in CMS Internet Only ...
What does TBD mean in revalidation?
All providers/suppliers not yet up for revalidation will display a "TBD" (To Be Determined) in due date field. If nothing is showing when and National Provider Identifier (NPI) is viewed, be sure there is not a space after the NPI. This will cause inaccurate information to display.
What happens if Noridian deactivates?
Deactivation of an organization will cause no payment to be made for any members associated to the organization. A lapse in coverage will occur from date of deactivation to when Noridian receives an application to reactivate enrollment. No payment will be made during those dates.
What happens if there is no space at the end of NPI?
If there is no space at end of NPI, and no due date populates, enrollment is not requested to revalidate at this time. If enrollment has revalidated successfully, or application is still in processing, due date will still populate on website.
How long before Noridian due date?
Reminder Emails. Noridian will also send out a reminder email roughly four months before due date. If correspondence email address is valid, another email will be sent a month and a half before due date again. This will be a generic email stating that your enrollment is due for revalidation.
Can you revalidate NPI if you are sole owner?
If you are a sole owner, meaning you have type 1 and a type 2 NPI, must revalidate BOTH enrollments at same time. This will apply even if one of enrollments has not been asked to revalidate. If completing application via PECOS, must submit two separate applications.
Does Noridian require documentation for Medicare?
Noridian will process the application as if it were a new enrollment. If supporting documentation currently exists in provider's file, the provider or supplier is not required to submit that documentation again during enrollment process. Application must be fully completed for enrollment to be active in Medicare.
How often does Medicare require revalidation?
Medicare requires all enrolled providers and suppliers to revalidate enrollment information every five years. To ensure compliance with these requirements, existing regulations at 42 CFR §424.515 (d) provide that (CMS is permitted to conduct off-cycle revalidations for certain program integrity purposes). 2.
Do I need to submit a CMS-855A?
You will need to submit a complete CMS-20134, CMS-855A, CM S-855B or CMS-855I application, depending on your provider / supplier type. If you enrolled in more than one state in our jurisdiction, you are required to submit a separate application for each state.
Does revalidation change enrollment?
No, the revalidation effort does not change other aspects of the enrollment process. Continue to submit changes (i.e., change of ownership, change in practice location or reassignment, final adverse action, etc.) as you always have. If you also receive a request for revalidation, respond separately to that request.
Do you need separate revalidation applications for each state?
If this occurs, separate revalidation applications are required for each state in which you must revalidate. If someone is completing the application on behalf of an individual provider, that person is strongly encouraged to coordinate with all groups / entities to ensure all reassignments remain intact. 10.
Can you use PECOS for revalidation?
If you wish to use internet-based PECOS to submit your revalidation application, you will have to select ‘ New Enrollment’ and complete the application under this scenario. You can also complete the paper application, which does allow you to select ‘Revalidation’ as a submission reason.
