
How do I check the status of a Medicare claim?
Dec 01, 2021 · Providers have a number of options to obtain claim status information from Medicare Administrative Contractors (MACs): • Providers can enter data via the Interactive Voice Response (IVR) telephone systems operated by the MACs. • Providers can submit claim status inquiries via the Medicare Administrative Contractors’ provider Internet-based portals.
How can providers obtain claim status information from Medicare administrative contractors?
To check the status of Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, ... Log into (or create) your secure Medicare account. You’ll usually be able to see a claim within 24 …
How can providers obtain claim status information from Macs?
Jun 06, 2021 · How do providers check Medicare claim status? Providers can enter data via the Interactive Voice Response (IVR) telephone systems operated by the MACs. Providers can submit claim status inquiries via the Medicare Administrative Contractors’ provider Internet-based portals. Some providers can enter claim status queries via direct data entry screens.
How do I view claim information?
Use the eligibility response to prepare accurate Medicare claims, determine patient liability, or check eligibility for specific services. MAC Online Provider Portal Each MAC offers its own Medicare online provider portal so you can access information anytime. Find your MAC’s website to register for your MAC’s portal. MAC IVR System
How long does it take Medicare to process claims?
approximately 30 daysMedicare takes approximately 30 days to process each claim. Medicare pays Part A claims (inpatient hospital care, inpatient skilled nursing facility care, skilled home health care and hospice care) directly to the facility or agency that provides the care.
How do I check my Medicare claim status Australia?
If you already have a Medicare online account, sign in through myGov. If you don't have a myGov account or a Medicare online account, you'll need to set them up. You can use your Medicare online account to manage details and claims, access statements and get letters online.Dec 20, 2021
What is a 277 claim status?
The Claim Status Response (277) transaction is used to respond to a request inquiry about the status of a claim after it has been sent to a payer, whether submitted on paper or electronically. Once we return an acknowledgment that a claim has been accepted, it should be available for query as a claim status search.
How do I check the status of my noridian Medicare portal?
InquiryGo to Claim Status from the main menu and the Claim Status Inquiry tab.Enter the required Beneficiary Details fields. Medicare Number. First and Last Name. Date of Birth.Dec 7, 2021
Can I see my Medicare bill online?
You can use your online MyMedicare account to view your Medicare premium bills, check your payment history and set up Medicare Easy Pay for auto payments.Mar 22, 2021
How do I get a copy of my Medicare Summary Notice?
Log into (or create) your Medicare account. Select "Get your Medicare Summary Notices (MSNs) electronically" under the "My messages" section at the top of your account homepage. You'll come to the "My communication preferences" page where you can select "Yes" under "Change eMSN preference," then "Submit."
How do I read a 277 file?
0:1413:38How to read and reconcile a 277 file - YouTubeYouTubeStart of suggested clipEnd of suggested clipFile itself we're going to talk about it in the context of the claim adjudication process and theMoreFile itself we're going to talk about it in the context of the claim adjudication process and the steps of billing. Between trading partners the acknowledgments received the status acknowledgments.
What is rejection code A7?
A7 - Acknowledgement/Rejected for Invalid Information - The claim/encounter has invalid information as specified in the Status details and has been rejected.
How many types of providers may be identified?
How many different types of providers may need to be identified? It may be necessary to identify four different types of providers. If another physician sent the patient, they need to be identified as the referring or ordering physician.
How do you access the Medicare portal?
This Web site can be accessed from the link: www.Medicare.gov. The beneficiary will enter their established Login ID and Password for that application in the Secure Sign In section of the web page.Dec 1, 2021
What is noridian Medicare portal used for?
Thank you for your interest in the Noridian Medicare Portal, Noridian Healthcare Solutions' application allowing access for authorized Medicare suppliers and providers; hereafter referred to as providers, to Medicare eligibility and claim information.
What is the noridian Medicare portal?
The Noridian Medicare Portal (NMP) is a free and secure, internet-based portal that allows users access to beneficiary and claim information. The portal is available for all Part A, Part B and Durable Medical Equipment (DME) users in the Jurisdictions of JA, JD, JE and JF.
How to check Medicare Part A?
To check the status of#N#Medicare Part A (Hospital Insurance)#N#Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.#N#or#N#Medicare Part B (Medical Insurance)#N#Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.#N#claims: 1 Log into (or create) your secure Medicare account. You’ll usually be able to see a claim within 24 hours after Medicare processes it. 2 Check your#N#Medicare Summary Notice (Msn)#N#A notice you get after the doctor, other health care provider, or supplier files a claim for Part A or Part B services in Original Medicare. It explains what the doctor, other health care provider, or supplier billed for, the Medicare-approved amount, how much Medicare paid, and what you must pay.#N#. The MSN is a notice that people with Original Medicare get in the mail every 3 months. It shows:#N#All your Part A and Part B-covered services or supplies billed to Medicare during a 3-month period#N#What Medicare paid#N#The maximum amount you may owe the provider
What is a Medicare summary notice?
Medicare Summary Notice (Msn) A notice you get after the doctor, other health care provider, or supplier files a claim for Part A or Part B services in Original Medicare. It explains what the doctor, other health care provider, or supplier billed for, the Medicare-approved amount, how much Medicare paid, and what you must pay. .
What is MSN in Medicare?
The MSN is a notice that people with Original Medicare get in the mail every 3 months. It shows: All your Part A and Part B-covered services or supplies billed to Medicare during a 3-month period. What Medicare paid. The maximum amount you may owe the provider. Learn more about the MSN, and view a sample.
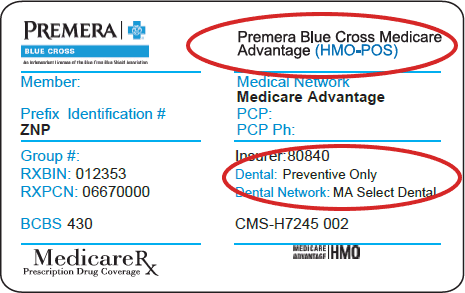
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
What is a PACE plan?
PACE plans can be offered by public or private companies and provide Part D and other benefits in addition to Part A and Part B benefits. claims: Contact your plan.
Does Medicare Advantage offer prescription drug coverage?
Medicare Advantage Plans may also offer prescription drug coverage that follows the same rules as Medicare drug plans. Check your Explanation of Benefits (EOB). Your Medicare drug plan will mail you an EOB each month you fill a prescription. This notice gives you a summary of your prescription drug claims and costs.
Claim Status Inquiry
View the status of claims, Medical Review comments and initiate a redetermination on finalized claims using the Claim Status tab.
Response
The claims that match the search criteria are displayed. Select the "View Claim" link to receive additional claim information.
Claim Processing Comments
NMP offers access to view claim processing comments if a claim had been selected for prepayment review in which Noridian requested documentation prior to making a claim decision.
Related Claim Details
NMP allows Part B providers access to gain more information about a finalized claim that was denied or received a reduced payment due to related services.
Expanded Denial Details
NMP provides claim denial details for the below claim denials. This will allow access to important details without a separate eligibility inquiry.
What is OneNet PPO?
OneNet PPO maintains the OneNet PPO Workers’ Compensation Network, a network of physicians, health care practitioners, hospitals and ancillary facilities used for work-related illness and injury. The network serves workers’ compensation programs administered by employers and TPAs contracted with Procura, an Optum Company.
What is virtual card payment?
Virtual Card Payments are subject to the terms and conditions governing card processing between you and your card service processor, and you are responsible for any charges and related third party fees, including interchange, merchant discount, or other card processing fees.
What is Direct Connect?
Using Direct Connect, you can track and manage overpayment requests, dispute an overpayment finding and submit refunds – reducing the letters and calls you receive from UnitedHealthcare, or the need to work with third-party vendors.
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
Claim Status Inquiry
- Available For: Part A, Part B, DME View the status of claims, Medical Review comments and initiate a redetermination on finalized claims using the Claim Status tab.
Inquiry
- Go to Claim Status from the main menu and the Claim Status Inquiry tab
- Enter the required Beneficiary Details fields.
Response
- The claims that match the search criteria are displayed. Select the "View Claim" link to receive additional claim information. Information received should match the Interactive Voice Response (IVR) system. Consult the Provider Contact Center if information returned is not as expected. The following table provides the field name and a description of...
Claim Processing Comments
- Available For: Part A, Part B, DME NMP offers access to view claim processing comments if a claim had been selected for prepayment review in which Noridian requested documentation prior to making a claim decision. Perform a Claim Status Inquiry as described above. If the claim had a history of being reviewed for additional documentation, the portal will offer a "Noridian Commen…
Related Claim Details
- Available For: Part B NMP allows Part B providers access to gain more information about a finalized claim that was denied or received a reduced payment due to related services. Types of claim situations providers can research include National Correct Coding Initiative edits, pre- or post-operative care following a service that had a global period, and/or duplicate claims. Perfor…
Expanded Denial Details
- Available For: Part A, Part B, DME NMP provides claim denial details for the below claim denials. This will allow access to important details without a separate eligibility inquiry. 1. Medicare Secondary Payer (MSP) Denial Details 2. Medicare Advantage/Health Maintenance Organization (HMO) Denial Details 3. Eligibility Denial Details 4. Date of Death Denial Details 5. Hospice Denia…